Lipoma arborescens (LAs) of the knee is relatively rare; however, it is important to consider, particularly in patients presenting with persistent pain and swelling and no recent history of trauma as the implications of a delayed or missed diagnosis of LA, especially of the bilateral knees may lead to early degenerative arthritis when left untreated.
Dr. Tyler M Goodwin, Department of Orthopaedic Surgery, University of Tennessee Health Science Center Chattanooga, Chattanooga, Tennessee. E-mail: goodwitm@gmail.com
Introduction: Lipoma arborescens (LAs) is a benign, intra-articular proliferation of fat cells in villous projections, creating a tree-like pattern on magnetic resonance imaging (MRI). The suprapatellar pouch is usually affected, and symptoms are typically gradual in nature, and patients may report painless swelling of the knee. Only ten cases of bilateral LA have been reported in the literature so far. Early recognition of this disease process and treatment may help to prevent prolonged symptoms and delays in care.
Case Report: A 49-year-old female with bilateral knee pain and intermittent swelling for over 20 years presented to our clinic with complaints of bilateral knee pain and swelling. She had previous steroid injection but no relief. After MRI was obtained concerning for LA, a surgical discussion was had with the patient about arthroscopic removal. She elected to proceed with surgery and underwent arthroscopic debridement of both knees. At her follow-up at 6 months for the right knee and 2 months for the left knee, she had a significant improvement in pain and quality of life.
Conclusion: LA of the knee is a rare condition, particularly bilateral, and in this patient, the diagnosis was missed for many years, and her definitive treatment was delayed. In her case, arthroscopic debridement of her bilateral LA proved to be a viable treatment option which significantly improved the patient’s quality of life and function.
Keywords: Lipoma arborescens, knee pain, benign tumor, knee arthroscopy.
Lipoma arborescens (LA) is benign proliferation of mature adipose cells in the synovium, most commonly seen in the knee, but has also been reported in other joints as well. It typically presents as chronic recurrent swelling that is recalcitrant to conservative measures and variable arthritic changes seen on X-rays [1]. Oftentimes patients will present with complaints of painless knee swelling. This is a relatively rare condition with an incidence of 0.25% as seen on magnetic resonance imaging (MRI) in patients with symptomatic knees [2, 3]. Bilateral involvement of knees is even rarer, with only ten reported cases reported in the literature [4, 5]. Arthroscopic debridement and open debridement have been the mainstays for treatment of this condition as steroid injections and conservative management often lead to recurrence of swelling and continued pain [5, 6].
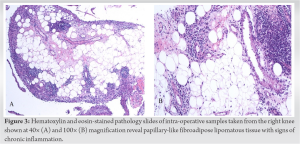
A 49-year-old physically active female with breast cancer in remission presented to clinic with complaints of bilateral knee pain and intermittent swelling for over 20 years. Her symptoms initially worsened steadily over the first 5 years and plateaued off in terms of severity and frequency of swelling. At the time of presentation, she was complaining of her right knee having more pain and effusion than her left. She did not experience any mechanical symptoms of locking, catching, or clicking. Previously, the patient had been treated by a physician with knee aspirations and steroid injections every 18 months with minimal relief. She was having issues walking, working, and having limitations in recreational hiking as well due to pain. Physical exam revealed bilateral knee effusions that were diffusely sore with no spot tenderness to palpation. No ligamentous instability, joint line tenderness, or patellar instability was appreciated in either knee. She had a negative rheumatology workup and bilateral knee MRIs revealed frond-like projections from the knee synovium (Fig. 1).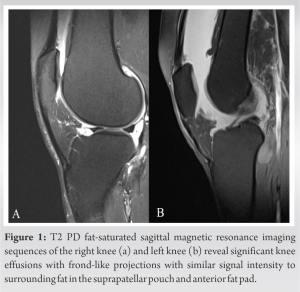
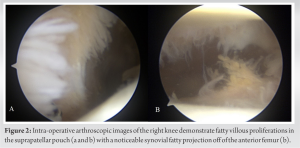
There is currently a paucity of cases reporting bilateral LA-treated arthroscopically. Historically, open resection was shown to be a viable treatment for LA, but arthroscopic debridement has become the procedure of choice with clinically favorable outcomes. Open resection, however, may still have a place in treatment for recurrence or lipomas that have a significant tumor burden making adequate arthroscopic debridement difficult or impractical [7, 8, 9]. No wound healing issues were appreciated with this patient, but a post-operative complication of left knee ecchymosis and suspected hematoma did occur. Notably, the left knee underwent a more extensive debridement. The most common complication for arthroscopic resection for LA is recurrence. There was no suspicion of recurrence at 6-month and 2-month follow-up for the right and left knee, respectively. Previous literature has shown that recurrence rate for arthroscopic resection and radiofrequency ablation is quite low at 2.8% but with a small relatively sample size pooled from multiple studies in mostly unilateral knees [1, 10].
Bilateral LAs can be treated with arthroscopic resection with satisfactory clinical outcomes, and clinical suspicion should be high in patients presenting with long history of knee pain and/or swelling with minimal other radiographic or clinical examination findings. We report that improvement in knee pain and swelling is favorable for patients undergoing arthroscopic LA debridement without previous underlying joint damage, regardless of the chronicity of the symptoms.
Although LA is a rare entity, it can cause significant discomfort and distress to patients. It is often overlooked as a diagnosis and may be a source of morbidity for patients for prolonged periods of time before being diagnosed and treated. Although rare, clinicians should consider this when evaluating patients with persistent knee effusions and pain in the setting of minimal or knee known intra-articular damage or injury. Despite being benign in nature, prolonged time to diagnosis and treatment may subject patients to unnecessary morbidity that can be treated favorably with arthroscopic debridement. Clinicians in these situations should have a high index of suspicion and low threshold for ordering advanced imaging in this setting.
References
- 1.Wang CK, Alfayez S, Marwan Y, Martineau PA, Burman M. Knee arthroscopy for the treatment of lipoma arborescens: A systematic review of the literature. JBJS Rev 2019;7:e8. [Google Scholar]
- 2.Miladore N, Childs MA, Sabesan VJ. Synovial lipomatosis: A rare cause of knee pain in an adolescent female. World J Orthop 2015;6:369-73. [Google Scholar]
- 3.Vilanova JC, Barceló J, Villalón M, Aldomà J, Delgado E, Zapater I. MR imaging of lipoma arborescens and the associated lesions. Skeletal Radiol 2003;32:504-9. [Google Scholar]
- 4.Zhu G, Tian X, Du D, Lei M, Guan L, Wang J, et al. Medical image analysis of knee joint lipoma arborescens and arthroscopic treatment. Comput Med Imaging Graph 2018;66:66-72. [Google Scholar]
- 5.Garnaoui H, Rahmi A, Messoudi A, Rafaoui A, Rafai M, Garch A, et al. Intra-articular lipoma arborescens of the knee: A report of two cases with bilateral localization. Int J Surg Case Rep 2018;51:224-7. [Google Scholar]
- 6.Nambiar M, Onggo JR, Jacobson A. Lipoma arborescens: A rare cause of clicking in the knee. BMJ Case Rep 2019;12:e227949. [Google Scholar]
- 7.Yilmaz E, Karakurt L, Akpolat N, Ozdemir H, Belhan O, Incesu M. Intra-articular lipoma of the knee joint in a girl. Arthroscopy 2005;21:98-102. [Google Scholar]
- 8.Cil A, Atay OA, Aydingöz U, Tetik O, Gedikoğlu G, Doral MN. Bilateral lipoma arborescens of the knee in a child: A case report. Knee Surg Sports Traumatol Arthrosc 2005;13:463-7. [Google Scholar]
- 9.Malkoc M, Korkmaz Ö. Results of arthroscopic synovectomy for treatment of synovial lipomatosis (lipoma arborescens) of the Knee. J Knee Surg 2018;31:536-40. [Google Scholar]
- 10.Pai SN, Ayyadurai P, Jeganathan PV, Perumal S, Arumugam S. Lipoma arborescens: Can we afford to miss it? ANZ J Surg 2022;92:218-22. [Google Scholar]