Aggressive and large aneurysmal bone cysts in proximity to the physis should be thoroughly curetted accompanied by packing of bone cement and preventive fixation to avert pathological fracture and provide support to the graft.
Dr. Shivam Mehra, Department of Orthopaedics, Padmashree Dr. D. Y. Patil School of Medicine, Navi Mumbai - 400 706, Maharashtra, India. E-mail: drshivammehra@gmail.com
Introduction: Aneurysmal bone cyst (ABC) is a benign, expansible, non-neoplastic tumor of usually long bones and is identified by blood vessels and spaces that are most often differentiated by fibrous septae. It is challenging to treat these rare, giant ABCs as they have a damaging effect on the bones and compress the nearby structures, especially in load-bearing bones of the body.
Case Report: We report a case of a giant ABC in the distal tibia one-third with soft tissue component of a 30-year-old male. The patient presented to our outpatient department with complaints of pain and swelling over left ankle for 1 year. The size of the swelling was 15 cm × 10 cm × 10 cm over medial aspect of ankle with 3 discharging sinuses which present over swelling. His blood parameters were suggestive of low hemoglobin count. X-rays showed cystic lesions over medial aspect of left ankle. Computed tomography scan and magnetic resonance imaging reports were suggestive of ABC.
Conclusion: Our case report is unique as it reminds us that when presented with a case of ABC, excision of fungating soft tissue with curettage followed by cementing can be a preferable and better treatment option. ABC was extensively curetted out, the formed cavity was packed with bone cement, and fixation with 3 cortico cancellous screws was carried out. At 4-month follow-up, the lesion had receded, and the patient was walking without pain and any deformity. We suggest that this method of treatment is beneficial for ABC at this site and at this age.
Keywords: Aneurysmal bone cyst, bone cement, curettage.
Aneurysmal bone cyst (ABC) is a benign expansible, non-neoplastic lesion of the bone, identified by blood vessels and spaces that are distinguished by fibrous septae. ABC has been reported to get transformed in some cases although most of them are benign lesions [1]. Usually, 75% of tumors are seen in the first 20 years of life, and almost 95% are seen in the first thirty of life [2]. Giant ABC is a rare condition which cannot be conveniently handled because of the aggressive and harmful effect of the cyst on the bones and compression on the adjacent structures, particularly in the load-bearing bones of the body. Treatment options suggested for ABC include curettage, curettage, or excision with cement filling or grafting of the bone, agents for fibrosis or bone marrow injections, embolization of the artery, radiotherapy or adjuvant cryotherapy, demineralized bone matrix applications, and segmental or en bloc resections. The advantage of en bloc resection is that it has the lowest recurrence rate, i.e., 0% [3]. We report a case of an ABC in the distal one-third tibia with soft tissue component.
A 30-year-old male presented with pain and swelling with 3 discharging sinuses over medial aspect of left ankle of size 15 cm × 10 cm × 10 cm in the past 1 year (Figs. 1 and 2).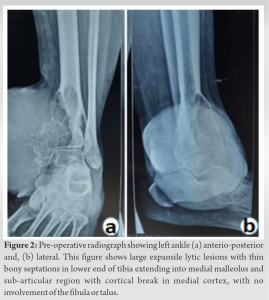


ABC is a lesion that usually occurs in the metaphysis of long bones, mainly the load-bearing ones. ABC can occur either as a primary or secondary lesion, for example, related with chondroblastoma or osteoblastoma. ABCs have a destructive and aggressive nature due to which apart from the metaphysis, physis of the bone also gets involved resulting to disturbances in growth plate and development of deformities [4]. ABC appears as a lytic and expansile lesion radiographically with septae and cortical thinning showing fluid-fluid levels on MRI, also observed in our case. Optimal treatment of ABC is arguable. In spite of several techniques reported in literature, the recurrence rate of ABCs lies anywhere between 5% and 40%, sometimes greater than that [5]. Even though newer techniques such as sclerotherapy (that uses sclerosing substances) and synthetic bone grafts have come into play, still they remain less effective in comparison to the conventional curettage method [6]. At present, curettage and packing the void with bone graft or polymethyl methacrylate are the cornerstone of treatment strategy [6]. Curettaging giant ABCs usually leave large defects which are difficult to treat. To reconstruct these large defects, multiple reconstructive alternatives such as autografts, allografts, and bone substitutes are available [7]. Amongst these, autografts are comparatively easier to incorporate than allografts as allografts experience a low-grade immune response and lack of osteocytes or both [8]. Recently, vascularized bone grafts have come into the picture as a treatment modality for large bone defects as they can be remodeled and incorporated faster; however, this is a challenging process [9]. Our choice was to use bone cement as they provide excellent structural bone support and are technically uncomplicated to use. Furthermore, literature shows brilliant long-term results of bone cementing [10]. In our patient, the final construct obtained was firm and allowed gradual weight-bearing without failure (Fig. 6 and 7). Post-operative clinical pictures and radiograph post 6-month follow-up are shown in Fig. 8 and 9.
Our case report is unique as it suggests us that when presented with a case of ABC, excision of fungating soft tissue with curettage with cementing can be a superior treatment option. ABC was curetted out extensively, the formed cavity was packed with bone cement, and fixation with 3 cortico cancellous screws was done. Depending on the location, aggressiveness, and extent of the tumor, the treatment for each ABC should be personalized. As per our recommendation, giant and aggressive ABCs near the physis of the bone should be thoroughly excised with a curettage accompanied by filling of bone cement and prophylactic fixation to avert pathological fracture and provide support to the graft.
In case of ABC present near the joint, proper curettage should be done and implant fixation along with bone cementing should be done for support.
References
- 1.Brindley GW, Greene JF Jr., Frankel LS. Case reports: Malignant transformation of aneurysmal bone cysts. Clin Orthop Relat Res 2005;438:282-7. [Google Scholar]
- 2.Bonakdarpour A, Levy WM, Aegerter E. Primary and secondary aneurysmal bone cyst: A radiological study of 75 cases. Radiology 1978;126:75-83. [Google Scholar]
- 3.Ramírez AR, Stanton RP. Aneurysmal bone cyst in 29 children. J Pediatr Orthop 2002;22:533-9. [Google Scholar]
- 4.McCarthy SM, Ogden JA. Epiphyseal extension of an aneurysmal bone cyst. J Pediatr Orthop 1982;2:171-5.. [Google Scholar]
- 5.Szendröi M, Cser I, Kónya A, Rényi-Vámos A. Aneurysmal bone cyst. A review of 52 primary and 16 secondary cases. Arch Orthop Trauma Surg 1992;111:318-22. [Google Scholar]
- 6.Dubois J, Chigot V, Grimard G, Isler M, Garel L. Sclerotherapy in aneurysmal bone cysts in children: A review of 17 cases. Pediatr Radiol 2003;33:365-72. [Google Scholar]
- 7.Güven M, Demirel M, Ozler T, Başsorgun IC, Ipek S, Kara S. An aggressive aneurysmal bone cyst of the proximal humerus and related complications in a pediatric patient. Strategies Trauma Limb Reconstr 2012;7:51-6. [Google Scholar]
- 8.Glancy GL, Brugioni DJ, Eilert RE, Chang FM. Autograft versus allograft for benign lesions in children. Clin Orthop Relat Res 1991;262:28-33. [Google Scholar]
- 9.Ghert M, Colterjohn N, Manfrini M. The use of free vascularized fibular grafts in skeletal reconstruction for bone tumors in children. J Am Acad Orthop Surg 2007;15:577-87. [Google Scholar]
- 10.Grzegorzewski A, Pogonowicz E, Sibinski M, Marciniak M, Synder M. Treatment of benign lesions of humerus with resection and non-vascularized, autologous fibular graft. Int Orthop 2010;34:1267-72. [Google Scholar]