ACL injury in a poliotic limb can be challenging to manage due to neuromuscular weakness. However with proper preoperative planning, proper intraoperative execution and correct postoperative therapy, it can be managed with a good outcome.
Dr. Jignesh Y Tandel, Department of Orthopaedics, ESIS Hospital, Mumbai, Maharashtra, India. E-mail: drjigneshtandel@gmail.com
Introduction: Prevalence of polio was very high in India before its eradication, with a number of people living with its residual effects. Anterior cruciate ligament (ACL) injury is the most common knee injury. To the best of our knowledge, this is the first report in literature presenting ACL injury in a poliotic limb and its management.
Case Report: A 30-year-old male with poliotic limb and equinovarus deformity presented with ACL injury to the same limb. ACL reconstruction was done using Peroneus longus graft. Postoperatively patient was gradually returned to preinjury activity levels.
Conclusion: ACL tears in a poliotic limb can be a challenging case. Proper preoperative planning and anticipation of problems can help in managing the case with a good outcome.
Keywords: ACL injury, Polio, ACL reconstruction, peroneus longus Graft, foot deformity.
India had the highest polio prevalence among developing nations, with an average of 500–1000 children affected per day [1]. Trivalent oral poliovirus vaccine was added to the expanded programme on immunisation (EPI) in 1979, however the prevalence of polio did not decline to its pre-EPI level for at least a decade [1]. Since 2004, yearly pulse polio vaccination programmes have been carried out 10 times annually. Each child was tracked and given the vaccine [2]. Polio was endemic in India until its recent eradication in January 2011 [3]. With persistent and extreme efforts, transmission was eventually interrupted due to which India’s success story is globally acclaimed [4]. The virus enters the body through the faeco-oral route and attacks the central nervous system. The central nervous system is the target of spread through retrograde axonal transport or through the circulation [5] Although the infection is typically subclinical, it can cause headaches, gastrointestinal problems, malaise, and neck and back stiffness, which may result in paralysis [6]. If the condition affects the respiratory muscles, it may be fatal. Poliomyelitis is characterized by loss of motor neurons, which may cause flaccid paralysis, muscle wasting and hyporeflexia [7]. It can affect any motor neuron, but typically has varying severity and affects one or both lower limbs. The quadriceps muscle is commonly affected. Patients who have limb palsy are often found to have ligamentous laxity, abnormal limb alignment and generalised hypotonia, which lead to knee pathology at an early age [8]. Angular deformities, external rotation of the tibia, severe valgus alignment, bone loss, narrowing of the femoral and tibial canals, diminished quadriceps strength, flexion contractures and genu recurvatum are some of the characteristics in a poliotic limb. Additionally, a wide range of hindfoot and ankle abnormalities, such as equinus, calcaneus, varus, valgus, pes planus, and cavus, as well as combinations of these (such as equino-varus, equino-valgus, calcaneo-varus, calcaneo-cavo-valgus, and equino-cavo-varus), are also reported. These factors make a poliotic limb more prone to ligament injuries. The anterior cruciate ligament (ACL) is one of the most frequently injured ligaments of the knee in Indian and Asian population [9, 10]. The ACL has been regarded as the main restraint on the tibia’s anterior translation with respect to the femur [11]. Due to its particular orientation, the ACL also helps maintain the stability of the knee during rotation in both the frontal and transverse planes [12]. It has also been hypothesised that a lack of neuromuscular control during dynamic movements is the root cause of ACL injury. ACL reconstruction for treatment of ACL injuries has become the standard universally. In these report, we present a case of ACL injury in a poliotic limb with equinovarus deformity at foot, treated with reconstruction using a peroneus longus graft.
A 30-year-old male presented to us with complaints of trauma to his right knee and instability during walking. Patient gave history of poliomyelitis in childhood of same leg, for which adequate physiotherapy and treatment was taken. Patient had an equinovarus deformity of the foot (Fig. 1).
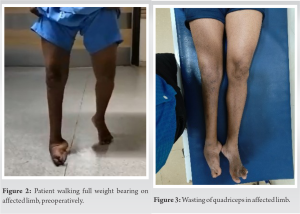
To the best of our knowledge, there has been no reported literature on ACL reconstruction in a polio affected limb. Polio afflicted limbs typically have osteoporosis, hyperextended knees, lax cruciate, capsular, and collateral ligaments, valgus alignment, and patellar baja [17]. Valgus or varus laxity is one of many causes of hyperextension abnormalities. Patients with polio commonly have reduced quadriceps strength [18]. Loss of motor neurons, which can result in flaccid paralysis, muscle atrophy, and hyporeflexia, is a hallmark of poliomyelitis [19]. In order to compensate for the loss of movement, the injured nerve fibres grow new nerve-end terminals (dendrites), which they attach to neighbouring muscle fibres. The result is functional movement recovery [20]. This procedure illustrates neuroplasticity, or the nervous system’s capacity to heal by creating nerve buds that strengthen the polio-affected nerve fibres and muscles. ACL reconstruction in polio patients can present several challenges due to the weakness or paralysis of the affected limb. Some of the challenges in ACL reconstruction in poliotic limbs include:
- Pre-operative planning: analysing all deformities, grading of muscle power, radiographs to assess bone quality and expectations and demands of the patient should be considered while planning the treatment
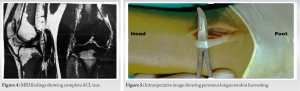
- Graft selection: in this case we decided to expend the peroneus longus tendon due to chronic varus deformity at the foot and avoid postoperative flexion deformity at the knee commonly seen with hamstrings graft and also the fact that there was mild quadriceps weakness
- Difficulty in assessing joint stability: Assessing joint stability can be challenging in polio patients due to the weakness or paralysis of the affected limb. Adequate radiographic investigations should be done prior to surgery. A diagnostic arthroscopy should always be performed prior to co relate the clinical and radiological findings
- Rehabilitation: Rehabilitation and physical therapy after surgery may need to be modified to accommodate the patient’s unique needs. The therapist may need to work with the patient to develop a specialized rehabilitation plan that takes into account the patient’s weakened or paralyzed limb
- Risk of complications: Polio patients may be at increased risk of complications following ACL reconstruction surgery owing to osteoporotic bones and weak muscles.
Young age of our patient, demand for a stable knee and pre-injury activity levels of the patient were factors on which we decided to reconstruct the ACL with a peroneus longus graft.
ACL injury in a poliotic limb can be challenging to manage due to neuromuscular weakness. However with proper preoperative planning, proper intraoperative execution and correct postoperative therapy, it can be managed with a good outcome.
References
- 1.John TJ, Vashishtha VM. Eradicating poliomyelitis: India’s journey from hyperendemic to polio-free status. Indian J Med Res 2013;137:881-94. [Google Scholar]
- 2.Vashishtha VM, Kumar P. 50 years of immunization in India: Progress and future. Indian Pediatr 2013;50:111-8. [Google Scholar]
- 3.Aylward B, Tangermann R. The global polio eradication initiative: Lessons learned and prospects for success. Vaccine 2011;29 Suppl 4:D80-5. [Google Scholar]
- 4.John TJ, Vashishtha VM. Path to polio eradication in India: A major milestone. Indian Pediatr 2012;49:95-8. [Google Scholar]
- 5.Ren R, Racaniello VR. Poliovirus spreads from muscle to the central nervous system by neural pathways. J Infect Dis 1992;166:747-52. [Google Scholar]
- 6.Clinical Manifestations of Infection with Poliomyelitis Virus. JAMA Network. Available from: https://www.jamanetwork.com/journals/jama/article-abstract/302243 [Last accessed on 2023 April 16]. [Google Scholar]
- 7.Available from: https://www.unignet.com.br/wp-content/uploads/2021_poliomielite-sindrome.pdf [Last accessed on 2023 April 16]. [Google Scholar]
- 8.López D, Peña N, Benítez E, Samudio S, Vecino P, Benvenutto E, et al. Clinical gait analysis in patient with poliomyelitis sequelae and total knee arthroplasty. Enferm Cuidados Humanizados 2021;10:75-88. [Google Scholar]
- 9.Chan CX, Wong KL, Toh SJ, Krishna L. Epidemiology of patients with anterior cruciate ligament injuries undergoing reconstruction surgery in a multi-ethnic Asian population. Res Sports Med 2021;29:12-24. [Google Scholar]
- 10.Kochhal N, Thakur R, Gawande V. Incidence of anterior cruciate ligament injury in a rural tertiary care hospital. J Family Med Prim Care 2019;8:4032-5. [Google Scholar]
- 11.Ligamentous Restraints to Anterior-Posterior Drawer in the h JBJS. Available from: https://www.journals.lww.com/jbjsjournal/citation/1980/62020/ligamentous_restraints_to_anterior_posterior.13.aspx [Last accessed on 2023 April 16]. [Google Scholar]
- 12.Quatman CE, Kiapour AM, Demetropoulos CK, Kiapour A, Wordeman SC, Levine JW, et al. Preferential loading of the ACL compared with the MCL during landing: A novel in sim approach yields the multiplanar mechanism of dynamic valgus during ACL injuries. Am J Sports Med 2014;42:177-86. [Google Scholar]
- 13.Paternostro-Sluga T, Grim-Stieger M, Posch M, Schuhfried O, Vacariu G, Mittermaier C, et al. Reliability and validity of the medical research council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med 2008;40:665-71. [Google Scholar]
- 14.Rhatomy S, Asikin AI, Wardani AE, Rukmoyo T, Lumban-Gaol I, Budhiparama NC. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27:3552-9. [Google Scholar]
- 15.Rhatomy S, Hartoko L, Setyawan R, Soekarno NR, Zainal Asikin AI, Pridianto D, et al. Single bundle ACL reconstruction with peroneus longus tendon graft: 2-years follow-up. J Clin Orthop Trauma 2020;11 Suppl 3:S332-6. [Google Scholar]
- 16.He J, Tang Q, Ernst S, Linde MA, Smolinski P, Wu S, et al. Peroneus longus tendon autograft has functional outcomes comparable to hamstring tendon autograft for anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2021;29:2869-79. [Google Scholar]
- 17.Hosalkar HS, Fuller DA, Rendon N, Esquenazi A, Keenan MA. Outcomes of total joint arthroplasties in adults with post-polio syndrome: Results from a tertiary neuro-orthopaedic center. Curr Orthop Pract 2010;21:273. [Google Scholar]
- 18.Beelen A, Nollet F, de Visser M, de Jong BA, Lankhorst GJ, Sargeant AJ. Quadriceps muscle strength and voluntary activation after polio. Muscle Nerve 2003;28:218-26. [Google Scholar]
- 19.Patterson BM, Insall JN. Surgical management of gonarthrosis in patients with poliomyelitis. J Arthroplasty 1992;7 Suppl:419-26 [Google Scholar]
- 20.Post-Polio Syndrome. Reeve Foundation. Available from: https://www.christopherreeve.org/living-with-paralysis/health/causes-of-paralysis/post-polio-syndrome-poliomyelitis [Last accessed on 2023 April 16]. [Google Scholar]











