Symptomatic presentation of Tarlov cyst though rare should be considered in the differential diagnosis and managed appropriately if identified as the source of symptoms.
Dr. Sathish Muthu, Department of Orthopaedics, Government Medical College, Dindigul, Tamil Nadu, India. E-mail: drsathishmuthu@gmail.com
Introduction: Tarlov cysts are rare perineural cysts noted as an incidental finding in approximately 1% of lumbar magnetic resonance imaging (MRI) arising from extradural components near the dorsal root ganglion. Due to its localization, it may cause sensory symptoms in some cases. However, most of these cysts are asymptomatic.
Case Report: We present the case of a 55-year-old woman with complaints of severe pain localized to the inner aspect of the thigh and gluteal region for the past 6 months, which has not been relieved by conservative management. On examination, there was a loss of sensation around the S2 and S3 dermatome with preserved motor functions. MRI showed a cystic lesion occupying the spinal canal with a size of about 1.3 × 0.7 cm with remodeling changes around the S2 vertebra. The cyst appears hypointense on T1 and hyperintense T2-weighted images. The diagnosis of the symptomatic Tarlov cyst was made and was managed with an epidural steroid injection. The patient was relieved of symptoms and remained asymptomatic till the latest follow-up at 1 year.
Conclusion: Symptomatic presentation of Tarlov cyst though rare should be considered and managed appropriately if identified as the source of symptoms. Conservative management with epidural steroids is a successful method in the management of smaller cysts without motor symptoms.
Keywords: Tarlov cyst, sacrum, spine, decompression.
In 1938, Tarlov first described a cystic finding in his autopsy studies of filum terminale as an incidental finding [1]. Tarlov cysts are rare perineural cysts noted as an incidental finding in approximately 1% of lumbar magnetic resonance imaging (MRI) [2]. “Perineural cyst” and “Nerve root cyst” are various synonyms for this condition arising from extradural components near the dorsal root ganglion. Due to its localization, it may cause sensory symptoms in some cases. However, most of these cysts are asymptomatic. Only a few cases have been reported so far in the literature on this lesion being symptomatic and its effective management strategies are debated [3, 4, 5, 6, 7]. We present a case of symptomatic Tarlov cyst presenting in the sacral root and discuss the strategies involved in their management.
We present the case of a 55-year-old woman with complaints of severe pain localized to the inner aspect of the thigh and gluteal region for the past 6 months. Our patient did have any history of urinary incontinence, constipation, or sexual dysfunction. The patient had a history of hysterectomy done 5 years ago which was uneventful. The patient was put on conservative management elsewhere with pain medications and physiotherapy which did not relieve her symptoms. On examination, the pain was corresponding to S2 and S3 sacral dermatomal levels with loss of sensation and preserved motor functions without any neurological deficit elsewhere. MRI showed a cystic lesion occupying the spinal canal with the size of about 1.3 × 0.7 cm around the S2 vertebra, as shown in Fig. 1.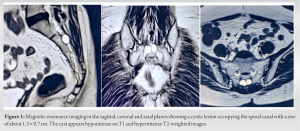
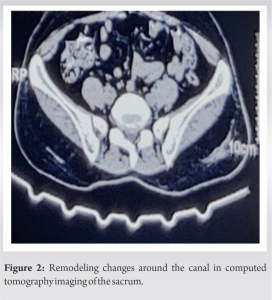
Tarlov postulated that these cysts occur due to the breakage of perineural venous drainage after any trauma [8]. Fortuna et al. [9] have considered these as congenital proliferation of the arachnoid membrane along the path of the exiting sacral nerve roots. The increase in the size of the cyst with time is due to the ball valve effect whereby cerebrospinal fluid enters during systole but fails to escape during diastole [7]. The spinal meningeal cysts have been classified by et al. [5] into three types where type 1 represents the extradural cyst not containing the spinal root fibers, while type 2 comprises the extradural cyst containing the spinal root fibers (Tarlov cyst classified as type 2) and type 3 intradural cyst. A recent survey by the Tarlov Cyst support group [10] noted that majority of the respondents were female (86.6%) and male population with this condition limited (13.4%). Similarly, the common age group of the respondents was between 31 and 60 years. Our patient also fits into this demographic profile. Apart from the cyst in the meninges, 33% respondents reported the presence of cysts in other regions of the body of which the common locations were abdomen, hand, and wrists. On analyzing the clinical presentation of the respondents, only 3% were without pain while 4.2% suffered from very mild pain; 7.6% mild pain; 31.5% moderate; 38.6% severe; and 15.1% suffered very severe pain due to the condition. The clinical features are sciatica, urinary incontinence, headache, constipation, sexual dysfunction, and loss of sensation, though the majority are asymptomatic. It may produce symptoms if it increases in size and compresses ventral roots which may produce motor deficits. MRI is usually diagnostic but delayed myelogram and CT myelogram are used to assess communication of the cyst with subarachnoid space. In our case report, this patient had prolonged symptoms that were not relieved by any medications or physiotherapy. During the MRI study, we identified a Tarlov cyst at the level of the S2 vertebra which corresponds to her pain distribution. Moreover, we did not find any other cause to explain her symptoms which made us diagnose the case as a symptomatic Tarlov cyst rather than an incidental finding. There is no clear indication for Tarlov cyst management. Some authors recommend cysts larger than 1.5 cm and or with bony destruction need to be managed with surgical decompression [11]. There are various treatment options such as percutaneous drainage, fenestration, and imbrication partial or total excision lumbar-peritoneal shunt, but everything has a controversial discussion in areas of failure, recurrences, and complications. Mostly, these surgical decompressive measures are only needed in large cysts with significant nerve root compression [3, 11, 12, 13, 14, 15]. There has been a successful report of cases managed with non-surgical measures such as oral steroids and epidural steroid injections [16, 17]. Hence, we decided to manage our case initially with an epidural steroid injection since the cyst was <1.5 cm, and depending on her response, we further planned for surgical decompression if deemed necessary. Fortunately, our patient showed a greater response to her symptoms with an epidural steroid injection. Voyadzis et al. [18] suggested larger cyst >1.5 cm in diameter greatly responded to motor symptoms of patients after excision and our patient presented only with sensory symptoms so we did not put her through further surgical decompression measures. In our case, the degenerative changes in the lumbar levels did not attribute to the cause of the pain based on her symptomatology but could not be exclusively ruled out, and hence, the successful result from epidural steroid might have an alternate hypothesis other than Tarlov cyst which might also be addressed with its usage.
Symptomatic presentation of Tarlov cyst though rare should be considered and managed appropriately if identified as the source of symptoms. Conservative management with epidural steroids is a successful method in the management of smaller cysts without motor symptoms. Further, reporting and analysis of similar cases are needed to know about the exact mechanism of these cyst formations and to establish various aspects of its effective treatment measures.
- Tarlov cysts are rare perineural cysts noted as an incidental finding in approximately 1% of lumbar MRI.
- The clinical features include sciatica, urinary incontinence, headache, constipation, sexual dysfunction, and loss of sensation, though the majority are asymptomatic.
- Symptomatic Tarlov cyst though rare should be kept in mind if found at an appropriate level without any other identifiable cause of patient symptomatology.
- Conservative management with epidural steroids is a successful method in the management of smaller cysts without motor symptoms.
References
- 1.Tarlov IM. Perineural cysts of the spinal nerve roots. Arch Neurol Psychiatry 1938;40:1067-74. [Google Scholar]
- 2.Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol 1994;15:293-7. [Google Scholar]
- 3.Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Tex Med 1987;83:55-6. [Google Scholar]
- 4.Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery 2000;47:74-8. [Google Scholar]
- 5.Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 1988;68:366-77. [Google Scholar]
- 6.Schreiber F, Haddad B. Lumbar and sacral cysts causing pain. J Neurosurg 1951;8:504-9. [Google Scholar]
- 7.Seaman WB, Furlow LT. The myelographic appearance of sacral cysts. J Neurosurg 1956;13:88-94. [Google Scholar]
- 8.Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry 1970;33:833-43. [Google Scholar]
- 9.Fortuna A, La Torre E, Ciappetta P. Arachnoid diverticula: A unitary approach to spinal cysts communicating with the subarachnoid space. Acta Neurochir (Wien) 1977;39:259-68. [Google Scholar]
- 10.Tarlov Cyst Support Group. Tarlov Cysts: What are they and How can they be Treated?. Available from: https://www.aans.org/. [Last accessed on 2022 Dec 24]. [Google Scholar]
- 11.Medani K, Lawandy S, Schrot R, Binongo JN, Kim KD, Panchal RR. Surgical management of symptomatic Tarlov cysts: Cyst fenestration and nerve root imbrication-a single institutional experience. J Spine Surg 2019;5:496-503. [Google Scholar]
- 12.Bartels RH, van Overbeeke JJ. Lumbar cerebrospinal fluid drainage for symptomatic sacral nerve root cysts: An adjuvant diagnostic procedure and/or alternative treatment? Technical case report. Neurosurgery 1997;40:861-4. [Google Scholar]
- 13.Patel MR, Louie W, Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am J Roentgenol 1997;168:367-70. [Google Scholar]
- 14.Morio Y, Nanjo Y, Nagashima H, Minamizaki T, Teshima R. Sacral cyst managed with cyst-subarachnoid shunt: A technical case report. Spine (Phila Pa 1976) 2001;26:451-3. [Google Scholar]
- 15.Caspar W, Papavero L, Nabhan A, Loew C, Ahlhelm F. Microsurgical excision of symptomatic sacral perineurial cysts: A study of 15 cases. Surg Neurol 2003;59:101-5. [Google Scholar]
- 16.Mitra R, Kirpalani D, Wedemeyer M. Conservative management of perineural cysts. Spine (Phila Pa 1976) 2008;33:E565-8. [Google Scholar]
- 17.Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech 2005;18:29-33. [Google Scholar]
- 18.Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: A study of 10 cases with review of the literature. J Neurosurg 2001;95:25-32. [Google Scholar]








