Non-classical Celiac disease is an underdiagnosed condition with many non-specific symptoms and known cutaneous manifestations, and it should be considered in the work-up of refractory post-operative skin complications.
Dr. Vikranth Mirle, Midwest Orthopedics at Rush, Rush University Medical Center, Chicago, Illinois, USA. E-mail: vikranthmirle@uchicagomedicine.org
Introduction: Non-classical Celiac disease is a previously undescribed cause of debilitating post-operative cutaneous complications following an orthopedic procedure. Non-specific symptoms and rarity of the disease pose a diagnostic challenge; however, given underdiagnosis and significant morbidity, after ruling out of acute pathology, Celiac disease should be included in differential diagnosis for refractory cutaneous complications following an operative procedure.
Case Report: A 34-year-old woman who underwent patellofemoral arthroplasty and medial patellofemoral ligament reconstruction experienced over 5 months of post-operative knee swelling, erythema, and pain unresponsive to antihistamines and negative infectious, vascular, and implant allergy testing workups. After careful dietary monitoring by an allergy specialist, she was tested and confirmed to have Celiac disease. Following cessation of her oral contraceptive pill and dietary gluten, her knee swelling, erythema, and debilitating pain resolved.
Conclusion: Skin erythema, swelling, and pain are known complications after any operative treatment, but after ruling out of acute infectious and thromboembolic processes, diagnosis and management of refractory complications pose a challenging scenario. In this rare phenomenon, previously undescribed, a patient presented with months of post-operative knee erythema, swelling, stiffness, and extreme pain on activity along with non-specific symptoms of headache and fatigue before diagnosis with Celiac disease. On cessation of her birth control and dietary gluten, her symptoms and knee function improved dramatically.
Keywords: Knee arthroplasty complication, celiac disease, medial patellofemoral reconstruction, patellofemoral arthroplasty, autoimmune disease.
Patellofemoral arthroplasty (PFA) has emerged as a viable tool in the surgical management of isolated patellofemoral arthritic conditions. Refinement in patient selection and advancements in implant design and surgical technique have resulted in improved implant performance and patient satisfaction [1, 2, 3]. However, post-operative stiffness and swelling is an uncommon, but frustrating complication following knee surgery, including PFA. The differential diagnosis for post-surgical swelling is broad. While extended post-operative pain, erythema, stiffness, and swelling are most concerning for an infectious etiology, a multitude of other etiologies, including thromboembolism and allergy-related complications, may be considered once an infection has been excluded from the study [4, 5]. Even more rare, genetic causes include mastocytosis and hereditary angioedema. Celiac disease is an autoimmune enteropathic disorder that classically affects the small intestine in response to dietary gluten sensitivity. With an estimated prevalence of 1% in the population, Celiac disease has garnered significant public attention over the last few decades [6]. However, non-classical Celiac disease is an underdiagnosed disorder with numerous cutaneous manifestations, including dermatitis herpetiformis, erythema nodosum, urticaria, and atopic dermatitis [7]. To the best of our knowledge, a cutaneous manifestation of non-classical Celiac disease following an orthopedic surgical procedure has not been reported previously. We report the case of a patient who developed refractory right knee swelling, pain, and erythema following combined PFA and medial patellofemoral ligament reconstruction (MPFLR) reconstruction. The patient’s symptoms were determined ultimately to be secondary to a non-classical form of Celiac disease, and her symptoms resolved expeditiously following discontinuation of gluten intake. The patient was informed that data concerning her case would be submitted for publication, and she provided consent.
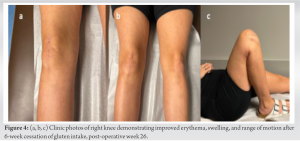
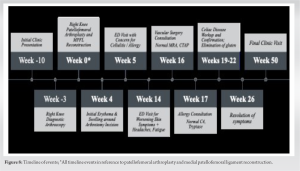
A 34-year-old female presented to clinic with an extensive history of right knee pain and patellar instability. The patient experienced three patellar dislocations as a high school student, all of which were treated nonoperatively. She endorsed intermittent anterior knee pain subsequently, which became progressive approximately 5 years before presentation. At the time of initial presentation in our clinic, her numeric rating pain scale ranged from 5 to 10/10. Physical examination was significant for a trace intra-articular effusion, a positive J sign, positive Clarke’s test, and positive patellar apprehension with passive lateral translation. Magnetic resonance imaging (MRI) demonstrated a laterally subluxated patella and significant patellofemoral osteoarthritis. Given the patient’s persistent knee pain and patellar instability, the patient was indicated for an initial diagnostic knee arthroscopy. During initial diagnostic knee arthroscopy, evaluation of the patellofemoral compartment confirmed lateral patellar subluxation and Outerbridge Grade 4 chondrosis of the medial and lateral patella facets. Based on these findings, the patient was indicated for a subsequent right knee patellofemoral resurfacing with concomitant MPFLR. On return to the operating room 7 weeks later, the patient was placed supine on the operating table, and a standard PFA was performed. Briefly, a 12 cm longitudinal midline incision was made on the anterior aspect of the right knee. Following a medial peripatellar arthrotomy, the patient’s trochlea was sized, prepared, and a 5 × 8.5 25 mm trochlear prosthesis and a 25 mm patellar button were implanted (PF Wave Implant System, Anika, Bedford, MA). After standard closure of the patellar arthrotomy, attention was turned to MPFLR. A 2.5 cm incision at the junction of the proximal one-third and distal two-thirds of the medial border of the patella was made for the MPFLR. A guidepin was placed at Shottle’s point under lateral radiography. The tibialis anterior allograft was then implanted on the femoral side with a 6.25 mm × 15 mm PEEK tenodesis screw and on the patellar side with two 2.4 PEEK suturetaks and four #4 FiberWire sutures. Following imbrication utilizing 0-Vicryl suture, the subcutaneous tissue and skin were closed in a layered fashion. At 4-week postoperatively, the patient noted an erythematous rash encompassing the arthrotomy incision. During this same period, she noticed increased knee stiffness, warmth, and swelling. On examination, her right knee had a trace effusion with range of motion (ROM) limited to 0–30°. The skin surrounding the knee was erythematous with mild urticaria, warm, blanchable, non-tender, and without edema. An outline of the redness was marked on her leg for comparison, and she was instructed to return to clinic in 2 days for repeat examination. In addition, the patient was started on a 7-day course of Bactrim with concern for a skin and soft-tissue infection. On return to clinic, the patient endorsed increasing pain and no change in erythema. She denied any systemic symptoms including fevers or chills. The patient’s vital signs remained stable, and examination was significant for newfound tenderness to palpation along the medial and lateral aspect of the joint line. The skin remained erythematous within previous boundary. The skin was warm and blanchable with no palpable edema. Mild intra-articular effusion remained. Neurovascular examination was intact, and the incision sites were well-healed and benign. Given persistent urticaria and erythema, the patient was referred to the emergency department (ED) for possible cellulitis or allergic reaction. In the ED, the patient was started on intravenous diphenhydramine and vancomycin before admission. During her admission, inflammatory markers and MRI were negative for infection with subjective improvement of erythema, urticaria, and swelling. The patient was discharged after 2 days with oral diphenhydramine and topical clabetasol with follow-up in clinic. Over post-operative week 7 through week 21, the patient continued to experience worsening of symptoms during activity including warmth and swelling around her knee, a reticular rash across the limb, and throbbing pain rated 10/10 (Fig. 1-3). 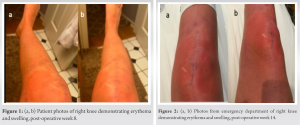

Refractory post-operative skin changes, swelling, and pain without other systemic signs are a challenging entity and have a wide differential diagnosis once acute infection and allergic reaction have been ruled out. 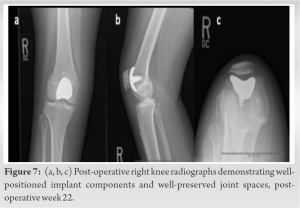
Skin erythema, swelling, and pain are known complications after any operative treatment, but after ruling out of acute infectious and thromboembolic processes, diagnosis and management of refractory complications pose a challenging scenario. In this rare phenomenon, previously undescribed, a patient presented with months of post-operative knee erythema, swelling, stiffness, and extreme pain on activity along with non-specific symptoms of headache and fatigue before diagnosis with Celiac disease. On cessation of her birth control and dietary gluten, her symptoms and knee function improved dramatically.
Post-operative skin erythema, swelling, and pain pose a challenging diagnostic scenario after ruling out of acute pathology including infectious, vascular, and acute allergy. In this case report, we demonstrate a previously undescribed phenomenon of non-classical Celiac disease as a cause of debilitating post-operative complications following a patellofemoral arthroplasty and medial patellofemoral reconstruction. Given the underdiagnosis and significant morbidity of celiac disease and autoimmune diseases in general, they are important to be included in the differential diagnosis of refractory post-operative complications after ruling out acute etiologies.
References
- 1.Familiari F, Madonna V, Mercurio M, Cinque ME, Gasparini G, Galasso O, et al. Outcomes and complications of inlay versus onlay patellofemoral arthroplasty: A systematic review. Knee 2023;41:124-36. [Google Scholar]
- 2.Strickland SM, Bird ML, Christ AB. Advances in patellofemoral arthroplasty. Curr Rev Musculoskelet Med 2018;11:221-30. [Google Scholar]
- 3.Li C, Li Z, Shi L, Gao F, Sun W. The short-term effectiveness and safety of second-generation patellofemoral arthroplasty and total knee arthroplasty on isolated patellofemoral osteoarthritis: A systematic review and meta-analysis. J Orthop Surg Res 2021;16:358. [Google Scholar]
- 4.Bohensky MA, deSteiger R, Kondogiannis C, Sundararajan V, Andrianopoulos N, Bucknill A, et al. Adverse outcomes associated with elective knee arthroscopy: A population-based cohort study. Arthroscopy 2013;29:716-25. [Google Scholar]
- 5.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 2012;40:1916-23. [Google Scholar]
- 6.Catassi C, Verdu EF, Bai JC, Lionetti E. Coeliac disease. Lancet 2022;399:2413-26. [Google Scholar]
- 7.Rodrigo L, Beteta-Gorriti V, Alvarez N, Gómez de Castro C, de Dios A, Palacios L, et al. Cutaneous and mucosal manifestations associated with celiac disease. Nutrients 2018;10:800. [Google Scholar]
- 8.Walsh JM, Huddleston HP, Alzein MM, Wong SE, Forsythe B, Verma NN, et al. The minimal clinically important difference, substantial clinical benefit, and patient-acceptable symptomatic state after medial patellofemoral ligament reconstruction. Arthrosc Sports Med Rehabil 2022;4:e661-78. [Google Scholar]
- 9.Pacheco KA. Allergy to surgical implants. Clin Rev Allergy Immunol 2019;56:72-85. [Google Scholar]
- 10.Granchi D, Cenni E, Trisolino G, Giunti A, Baldini N. Sensitivity to implant materials in patients undergoing total hip replacement. J Biomed Mater Res B Appl Biomater 2006;77:257-64. [Google Scholar]
- 11.Research C for DE and. Medications and Gluten. FDA. Published online; 09 February, 2019. Available from: https://www.fda.gov/drugs/ensuring-safe-use-medicine/medications-and-gluten. [Last accessed on 2023 Feb 07]. [Google Scholar]
- 12.Elwenspoek MM, Thom H, Sheppard AL, Keeney E, O'Donnell R, Jackson J, et al. Defining the optimum strategy for identifying adults and children with coeliac disease: Systematic review and economic modelling. Health Technol Assess 2022;26:1-310. [Google Scholar]
- 13.Cole MW, Ross BJ, Collins LK, Imonugo O, Sherman WF. The impact of celiac disease on complication rates after total joint arthroplasty: A matched cohort study. Arthroplast Today 2022;17:205-10.e3. [Google Scholar]
- 14.Gatti S, Lionetti E, Balanzoni L, Verma AK, Galeazzi T, Gesuita R, et al. Increased prevalence of celiac disease in school-age children in Italy. Clin Gastroenterol Hepatol 2020;18:596-603. [Google Scholar]











