Os Vesalinum pedis, though rare, should be kept as a differential diagnosis in the management of lateral foot pain.
Dr. Ashish Jacob Mathew, Department of Orthopaedics, Pushpagiri Institute of Medical Sciences and Research Center, Tiruvalla, Kerala, India. E-mail: ashishjacob96@gmail.com
Introduction: Os vesalianum pedis (OVP) is a rare accessory ossicle of the foot located proximal to the base of 5th metatarsal. It is usually asymptomatic but can mimic an avulsion fracture of proximal 5th metatarsal and is an infrequent cause of lateral foot pain. There have only been 11 cases of symptomatic OVP reported in the current literature.
Case Report: Our patient, a 62-year-old male presented with lateral foot pain following an inversion injury of his right foot, with no history of any previous trauma. What was initially mistaken as an avulsion fracture of the 5th metacarpal base was later revealed to be an OVP on contralateral X-ray.
Conclusion: Treatment is mostly conservative, but surgical excision can be done in cases following failed non-operative treatment. In the context of trauma, OVP must be differentiated from other causes of lateral foot pain such as Iselin’s disease and avulsion fractures of base of 5th metatarsal. Understanding the various etiologies of the condition and what those etiologies are usually related to can help prevent unnecessary treatment.
Keywords: Os vesalianum pedis, lateral foot pain, foot ossicles, 5th metatarsal avulsion fracture.
The foot and ankle are highly prone to anatomic variations. According to a recent study, the prevalence of accessory foot ossicles can be as high as 26%. It was Andreas Vesalius, anatomist and physician, who first described it in “de humani corporis fabrica” in 1543, and later on, this accessory ossicle was named “Os vesalianum pedis (OVP)” by Pfitzner in the memory of Andreas Vesalius [1]. With a radiological incidence that ranges between 0.1% and 0.4%, OVP is a rare, mostly bilateral, accessory ossicle of the foot [2, 3, 4, 5, 6]. The accessory bones of the foot are regarded as skeletal variants, and the most frequent accessory bones in adult feet are the accessory navicular (11.7%), os peroneum (4.7%), os trigonum (2.3%), os supranaviculare (1.6%), os supratalare (0.2%), and os intermetatarseum (0.2%). OVP is usually asymptomatic and only 11 cases of symptomatic OVP have been reported so far in the current literature and this is only the 4th case treated conservatively [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. We place a strong emphasis on thoroughly examining every patient with lateral foot pain in cases that are similar, to prevent the misdiagnosis of the condition and subsequent overtreatment. Undiagnosed lateral foot pain can be avoided by the awareness of various etiologies for the condition as well as what those etiologies are typically related to.
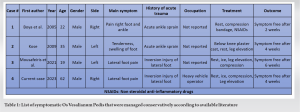
A healthy 62-year-old male was brought into our hospital’s emergency room complaining of lateral foot pain, edema, and restricted mobility in his right great toe. A few hours before being admitted to the emergency room, he indicated a history of trauma to his right foot, maybe including an inversion-type injury. The patient did not report any significant past history of trauma or previous lateral foot pain. He had initially consulted a local physician soon after the incident, who had taken radiographs of the right foot and diagnosed an avulsion fracture of the base of 5th metatarsal with an undisplaced fracture of distal phalanx of right big toe (Fig. 1). 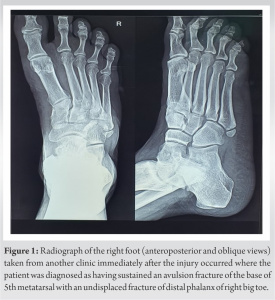
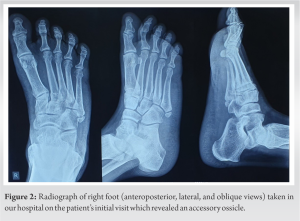

With an incidence rate of 0.1–5.9%, the OVP is an uncommon accessory ossicle of the foot [11, 12, 13]. We describe a rare instance of OVP that developed symptoms following a severe traumatic event. This is only the fourth instance of a symptomatic OVP that was treated conservatively that we are aware of. The applicable literature does contain cases that were handled conservatively [8, 9, 10] (Table 1), despite the fact that surgery was used to treat the majority of the reported cases [1, 7, 2, 3, 4, 5, 6, 13] Before suffering an inversion injury to the right foot, our patient was asymptomatic. We know of three instances of OVP that are comparable. They all mentioned young men who were brought into the emergency department with a severe ankle sprain and lateral foot pain. An accessory ossicle was detected through radiography. In the Kose case [9], the OVP was initially misdiagnosed as a fracture of the base of the fifth metatarsal, and a below-the-knee plaster was used to treat it. Ankle sprain care guidelines were used to treat the patient conservatively after the patient’s first radiographs were reevaluated to confirm the diagnosis of the OVP. In the instance discussed by Boya et al. [10], radiography of the contralateral (healthy) foot indicated the existence of the OVP bilaterally, which is similar to our situation. A CT scan confirmed the diagnosis, and the patient was once more given conservative treatment. The first radiographs in the case described by Mousafeiris et al. [8] were mistaken for an avulsion fracture of the base of the 5th metatarsal, but the contralateral foot’s radiography showed a similar pattern. The patient received conservative care. All patients received great follow-up reports. Although there are a few theories, nobody is quite sure about the exact origins of OVP. According to one view, the OVP is a persistent apophysis [8]. At the skeletal maturation age of 10 years for girls and 12 years for boys, an apophyseal line at the base of the fifth metatarsal is discernible in X-rays. This apophysis typically fuses 2 years later, starting at age 12 for girls and 14 for boys [14]. Another hypothesis proposes that the origin of the OVP is a fracture of the fifth metatarsal tuberosity [6]. One of most generally accepted hypotheses, which is reinforced by the fact that the OVP has articular cartilage, states that it is a true sesamoid bone [15]. OVPs are a rare source of discomfort of the lateral foot. Actually, the existence of OVP does not guarantee that it will be symptomatic and result in foot discomfort and incapacity [9]. In addition to the OVP, a number of other clinical entities, such as Iselin’s disease, an avulsion fracture of the base of fifth metatarsal, Jones fracture, metatarsal stress fracture, and os peroneum, are included in the differential diagnosis of lateral foot discomfort in a patient [8, 9, 14]. Nonunion of a tuberosity fracture, an ununited apophysis, or an ossifying apophysis of the base of fifth metatarsal are additional diagnoses on the differential list [8, 14]. Consider Iselin’s disease, which is a traction apophysitis of the base of fifth metatarsal, particularly if you have young children or adolescents [14]. Iselin’s disease is most likely caused by repetitive microtrauma brought on by the traction of the peroneus brevis tendon on the unfused apophysis; as a result, it is an overuse injury [8, 14]. The most frequent symptom, lateral foot discomfort, is made worse by activities, especially running. Its distinguishing feature is that the discomfort goes away when the apophysis fuses, which occurs around the ages of 12 and 14 for males and girls, respectively. In Iselin’s disease, radiographic imaging shows apophyseal fragmentation and irregularity. Early on in the disease’s progression, radiographs may come back negative. The early diagnosis of the disease is aided by magnetic resonance imaging (MRI) results since they appear before radiography epiphyseal fragmentation [8]. When comparing OVP to Iselin’s disease, age can be thought of as a good screening tool because Iselin’s illness typically manifests in young adults and gets worse with sports activities. On the other hand, the OVP persists past adulthood. The lateral foot discomfort associated with Iselin’s disease also has no history of trauma, in contrast to OVP, which typically develops symptoms following an ankle sprain or foot inversion injury [7, 8]. OVP can be misdiagnosed in the setting of trauma as a fifth metatarsal avulsion fracture, Jones fracture, or fifth metatarsal stress fracture [9]. If so, treatment for the patients can involve needless immobilization [7, 9]. OVP, however, possesses traits indicative of an accessory bone that aid in recognition and speedy diagnosis. It typically has an oblique synchondrosis line separating it from the base of fifth metatarsal. The ossicle is encircled by cortical bone and has a spherical form with smooth edges. The OVPs articulation with the cuboid bone, however, is its standout feature [10, 11, 12, 15]. Since the fracture line is acute and the bone fragment lacks cortication, the foregoing characteristics are not present in fractures of the fifth metatarsal base [9]. In addition, the direction of the fracture line and the apophyseal line is very different and nearly invariably perpendicular to one another in all types of fractures, including avulsion fractures, Jones fractures, and stress fractures. Avulsion fractures typically have a transverse direction, whereas the apophysis appears as a longitudinal line parallel to the long axis of the fifth metatarsal [8, 9]. A transverse fracture that does not extend distally to the fourth and fifth intra-metatarsal articulations is referred to as a Jones fracture on radiographs and occurs at the intersection of the diaphysis and metaphysis. The proximal pole of the fifth metatarsal is the site of avulsion fractures. Diaphyseal fracture at the proximal 1.5 cm of the shaft is known as a stress fracture of the proximal fifth metatarsal and is brought on by persistent, frequent trauma. In plain radiographs, stress fractures are located more distally and transversely [7, 8]. Os peroneum must be distinguished from OVP because it is a sesamoid bone with a bean-like form. The peroneus longus tendon’s distal end is typically where it is located. OVP and the Os peroneum both articulate with the cuboid bone, although the Os peroneum is smaller [8]. Imaging is crucial in the diagnosis of the OVP together with clinical suspicion. X-rays of both feet are crucial for the initial screening since OVP is typically bilateral. It is also possible to use an MRI; however, its results might not be conclusive [1]. The cause of OVP has also been further evaluated using bone scintigraphy [7]. Rest, specialized shoe insoles, stretching drills, analgesics NSAIDs, restricted weight-bearing, and/or casts should be the first line of treatment for symptomatic OVP [2, 4, 5, 6, 10]. Surgical options should be taken into account in situations where conservative treatment is ineffective. Excision of the problematic OVP without damaging the insertion of the peroneus brevis tendon is one surgical approach, as are osteosynthesis and bone grafting; both procedures have been shown to have positive functional outcomes [7, 8, 2, 4, 5, 6]. To prevent maltreatment, it is crucial to confirm if the OVP is to blame for the discomfort of the lateral foot.
To prevent overtreatment, it is critical to be mindful that OVP could be present as an uncommon cause of lateral foot discomfort. OVP can be interpreted as a potential fifth metatarsal base avulsion fracture, and the proper diagnosis requires a high index of suspicion, especially in cases where you see sclerotic edges without a previous history of trauma. Apart from fractures of the fifth metatarsal (avulsion fracture, Jones fracture, and stress fracture), differential diagnosis also includes Iselin’s disease and various accessory ossicles. The most effective way to show accessory ossicles with their articulations is using a lateral oblique radiograph with contralateral radiographs of opposite foot. Surgery is only indicated in refractory patients after the initial course of conservative treatment has failed.
OVP is a rare condition which can be a causative factor for lateral foot pain. This can be frequently mistreated and misinterpreted as a fracture of the base of the fifth metatarsal. Although rare it should be evaluated cautiously and considered as a differential diagnosis in cases with lateral foot pain
References
- 1.Aykanat F, Vincenten C, Cankus MC, Kose O, Sindel M. Lateral foot pain due to os vesalianum pedis in a young football player; A case report and review of the current literature. Skeletal Radiol 2019;48:1821-8. [Google Scholar]
- 2.Beil FT, Burghardt RD, Strahl A, Ruether W, Niemeier A. Symptomatic os vesalianum: A case report and review of the literature. J Am Podiatr Med Assoc 2017;107:162-5. [Google Scholar]
- 3.Smith AD, Carter JR, Marcus RE. The os vesalianum: An unusual cause of lateral foot pain a case report and review of the literature. Orthopedics 1984;7:86-9. [Google Scholar]
- 4.Inoue T, Yoshimura I, Ogata K, Emoto G. Os vesalianum as a cause of lateral foot pain: A familial case and its treatment. J Pediatr Orthop B 1999;8:56-8. [Google Scholar]
- 5.Wilson TC, Wilson RC, Ouzounov KG. The symptomatic os vesalianum as an uncommon cause of lateral foot pain: A case report. J Am Podiatr Med Assoc 2011;101:356-9. [Google Scholar]
- 6.Petrera M, Dwyer T, Ogilvie-Harris DJ. A rare cause of foot pain with golf swing: Symptomatic os vesalianum pedis-a case report. Sports Health 2013;5:357-9. [Google Scholar]
- 7.Dorrestijn O, Brouwer RW. Bilateral symptomatic os vesalianum pedis: A case report. J Foot Ankle Surg 2011;50:473-5. [Google Scholar]
- 8.Mousafeiris VK, Papaioannou I, Kalyva N, Arachoviti C, Repantis T. Os vesalianum pedis in a young adult: A case report and literature review. Cureus 2021;13:e14896. [Google Scholar]
- 9.Kose O. Os vesalianum pedis misdiagnosed as fifth metatarsal avulsion fracture. Emerg Med Australas 2009;21:426. [Google Scholar]
- 10.Boya H, Ozcan O, Tandoğan R, Günal I, Araç S. Os vesalianum pedis. J Am Podiatr Med Assoc 2005;95:583-5. [Google Scholar]
- 11.Tsuruta T, Shiokawa Y, Kato A, Matsumoto T, Yamazoe Y, Oike T, et al. Radiological study of the accessory skeletal elements in the foot and ankle (author’s transl). Nihon Seikeigeka Gakkai Zasshi 1981;55:357-70. [Google Scholar]
- 12.Cilli F, Akçaoğlu M. The incidence of accessory bones of the foot and their clinical significance. Acta Orthop Traumatol Turc 2005;39:243-6. [Google Scholar]
- 13.Miswan M, Hussin A, Thangaraju S. Misdiagnosed os vesalianum as fifth metatarsal avulsion fracture: A case report. Int J Sci Res 2013;4:1874-1875 [Google Scholar]
- 14.Canale ST, Williams KD. Iselin’s disease. J Pediatr Orthop 1992;12:90-3. [Google Scholar]
- 15.Coskun N, Yuksel M, Cevener M, Arican RY, Ozdemir H, Bircan O, et al. Incidence of accessory ossicles and sesamoid bones in the feet: A radiographic study of the Turkish subjects. Surg Radiol Anat 2009;31:19-24. [Google Scholar]