This article highlights the importance of a tailored surgical technique for treating a triple disruption of the superior shoulder suspensory complex and demonstrates that the combination of surgery and early active rehabilitation leads to good functional outcomes.
Dr. Matthieu Jaën, Department of Orthopaedic Surgery, CHUV, rue du Bugnon 21, 1011 Lausanne, Switzerland. E-mail: jaen.matthieu@gmail.com
Introduction: The shoulder girdle is composed of two arches, and these two arches are held together by the superior shoulder suspensory complex (SSSC), a ligamentous complex. Goss’s 1993 description of the SSSC as a ring includes the glenoid, coracoid process, coracoclavicular ligaments, distal clavicle, acromioclavicular joint, and acromion. Goss also noted in a 1996 study that a rupture of the SSSC in two places can result in an unstable lesion. This case report presents an unusual association of fractures involving the coracoid process, acromion, and distal clavicle, which has rarely been reported in the literature. Indeed, a triple lesion of the SSSC is very uncommon and the treatment is still debated. Therefore, we propose a surgical technique which we believe to have provide good results.
Case Report: A 54-year-old Caucasian male patient presented with Neer I distal third fracture of the clavicle, a displaced fracture of the acromion, and a fracture of the coracoid process following a left shoulder trauma after an epileptic crisis. The patient underwent surgery and has been followed for 1 year with good clinical and functional outcomes.
Conclusion: This case report highlights the complexity of lesions of the SSSC and the importance of determining proper surgical technique based on the type of lesion. It demonstrates that surgery combined with active rehabilitation can lead to good functional outcomes for patients with this type of injury. This report will be of interest to clinicians involved in the treatment of this type of lesion and should add a valuable treatment option for the treatment of triple disruption of the SSSC.
Keywords: Shoulder fractures, superior shoulder suspensory complex, surgical technique.
Acromial and coracoid fractures are very rare and represent 3–7% of scapular fractures, which themselves represent 1–3% of all fractures [1]. Acromial fractures represent 8–16% of scapular fractures and are found in 5–7% of cases in complications after reverse shoulder arthroplasty [2].
The shoulder girdle is formed by two arches:
- A superior arch: Composed of the acromioclavicular joint, the clavicle, the sternoclavicular joint, and the costoclavicular junction.
- An inferior arch: Composed of the glenoid cavity, the scapulothoracic space, and the scapula.
These two arches are attached together by a ligamentous complex called the superior shoulder suspensory complex (SSSC). The SSSC, described by Goss (1993), is a ring composed of the glenoid, the coracoid process, the coracoclavicular ligaments, the distal extremity of the clavicle, the acromioclavicular joint, and the acromion (Figs. 1 and 2) [3].
The patient is 54 years old and underwent a left shoulder trauma after an epileptic crisis.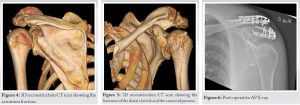
- A Neer I distal third fracture of the clavicle [5]
- A displaced fracture of the acromion
- A fracture of the coracoid process Ogawa type I [6].
Due to the damage in two places of the SSSC, a surgical indication is withheld.
Surgical technique
The patient is in beach chair position, 1.5 g of cefuroxime is introduced at induction, and he is under general anesthesia. We start by the acromial fracture with a posterior approach centered on the interspinous crest. Under radioscopic control, a 2.0-mm plate is laid on the superior part of the acromion and a second 2.8-mm plate is laid posteriorly on the interspinous crest. We then use a saber approach over the coracoid to reach the clavicle. Under radioscopic control, we apply a first 2.8-mm plate over the fracture. A second 2.8-mm plate is laid down after we notice that the clavicle is still mobile. These two plates are responsible for creating a stress zone, for which reason we introduce a third longer 2.8-mm plate superiorly on the clavicle to better distribute the stress zones. We complete the approach with a MIPO incision on the medial clavicle to apply the third plate. To neutralize the strengths applied on the coracoid, we complete the osteosynthesis by a transglenoid endobutton lacing. Finally, we deal with the coracoid fracture. Under radioscopic control, we pin the coracoid until the transglenoid level and insert a first 40-mm punched screw. We insert a second 2.8-mm cortical screw to complete the assembly (Fig. 6 and 7).
Follow-up
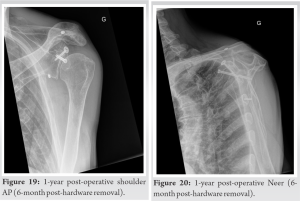
The patient had a 1-year post-operative follow-up with checkups at 6 weeks, 3, 6, 9 months, and 1 year. He benefited from physiotherapy with a free mobilization with no strength during the first 12 weeks, followed by progressive muscle strengthening. At 6 weeks, the patient does not complain of pain and has acquired excellent mobility. His active mobilization was of the following on the right and left side, in flexion 150–140°, abduction 130–120°, external rotation 50–45°, and internal rotation at L2-L3. The shoulder and clavicle X-rays show good joint ratio and no secondary displacement of the material nor of the fractures. At 3 months, the active mobilization on the right and left side is in flexion 150–150°, abduction 135–120°, external rotation 50–50°, and internal rotation at L2-L3. The X-rays start to show signs of consolidation. At 6 months, the patient is bothered by the orthopedic material and has discomfort on shoulder abduction and pain with adduction and palpation of the AC joint. The active mobilization of the left shoulder is in flexion 150°, abduction at 150°, external rotation at 50°, and internal rotation at L2. A scanner is planned to evaluate the rotator cuff and verify the fracture consolidation in sight of material removal. The scanner shows a good consolidation of the acromial and clavicle fractures but shows a pseudarthrosis of the coracoid fracture without secondary displacement and severe arthrosis of the AC joint. The removal of material is planned with a secondary osteosynthesis of the coracoid. The incision is made using the previous scars and all the material is removed without difficulty. The 4.0 cannulated screw is changed for a 5.0 screw to improve the coracoid stability, and another 4.0 cannulated screw is inserted at the location of the pseudarthrosis to reinforce the coracoglenoid osteosynthesis. We also reset by 5 mm the distal extremity of the clavicle because of an advanced symptomatic acromioclavicular arthrosis, making sure to preserve the posterior ligament (Fig. 8).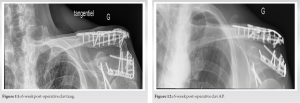
Fractures associated to the coracoid process, the acromion, and the distal clavicle are very rare, there are few cases described in the literature, and so there is little documentation of the treatment options. A careful pre-operative planning is required to assure an optimal result, leading to a good functional outcome and a reduced morbidity associated to this complex wound. Goss reports two similar cases [3]. In the first case, the acromial fracture was simply stabilized with a guidewire, while the distal clavicle and acromial fractures were not treated surgically. The latter fractures reduced spontaneously. In the second case, the non-displaced acromial fracture was fixed with a plate, and the distal clavicle fracture was stabilized with a guidewire and the coracoid fracture with a Kirschner pin. The bones healed in both places. Goss recommended later on the use of a cannulated screw instead of the Kirschner pin in the coracoid fractures. Goss assessed that the distal Neer I clavicle fracture associated to a coracoid apophysis fracture was functionally equivalent to the instability of a Neer II distal clavicle fracture and that they should be treated as such [4]. Eyres et al. (1995) reported the case of a displaced clavicle fracture associated to a coracoid apophysis fracture that extended to the superior edge of the scapula and the glenoid. They fixed the coracoid apophysis fracture with a unique 3.5-mm lag screw and inserted through the base of the coracoid in the scapular body. The clavicle was fixed with a six-hole plate. However, Eyres et al. did not describe the surgical sequence [7]. Lecoq et al. (2001) described a triple rupture of the SSSC implicating the distal third of the clavicle, the acromion, and the coracoid process. They attempted an open reduction and osteosynthesis of the coracoid process with screws while the two latter fractures were treated conservatively [1]. Jung et al. (2011) described a triple rupture of the SSSC including a displaced fracture of the distal clavicle, a coracoid apophysis fracture, and a non-displaced acromial fracture. The coracoid apophysis fracture was treated with a screw, and the clavicle and acromial fractures were treated with two Kirschner pins [8]. Mariño et al. (2013) presented the case of a triple lesion of the SSSC in a 26-year-old patient, with a type II Neer fracture of the clavicle associated with an acromial and a coracoid process fracture treated by osteosynthesis of the clavicle by two Kirschner pins, two cannulated screws in the acromion and a conservative treatment of the coracoid process [9]. The final results seem to show that surgery is a reliable treatment for these multiple lesions of the SSSC. Combined with active rehabilitation, the surgery improves the recovery of the shoulder function [10]. For this case report, the patient required the removal of the material and a secondary osteosynthesis of the coracoid process but he recovered a good shoulder function and does not complain of pain at 3 months after the second operation.
Lesions of the SSSC are very variable and complex. It is important while deciding the treatment to determine properly the surgical technic considering the biomechanical concepts of the SSSC. The different cases described in the literature seem to show that surgery offers good results. The decision to restore the integrity or simply stabilize part of the structures must be taken case by case according to the type of lesion the patient presents.
The surgical technique that we propose seems to give good clinical results and could be useful in the management of these rare and complex lesions.
References
- 1.Lecoq C, Marck G, Curvale G, Groulier P. Triple fracture of the superior shoulder suspensory complex. Acta Orthop Belg 2001;67:68-72. [Google Scholar]
- 2.Hill BW, Anavian J, Jacobson AR, Cole PA. Surgical management of isolated acromion fractures: Technical tricks and clinical experience. J Orthop Trauma 2014;28:e107-13. [Google Scholar]
- 3.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma 1993;7:99-106. [Google Scholar]
- 4.Goss TP. The scapula: Coracoid, acromial, and avulsion fractures. Am J Orthop (Belle Mead NJ) 1996;25:106-15. [Google Scholar]
- 5.Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res 1968;58:43-50. [Google Scholar]
- 6.Ogawa K, Yoshida A, Takahashi M, Ui M. Fractures of the coracoid process. J Bone Joint Surg Br 1997;79:17-9. [Google Scholar]
- 7.Eyres KS, Brooks A, Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br 1995;77:425-8. [Google Scholar]
- 8.Jung CY, Eun IS, Kim JW, Ko YC, Kim YJ, Kim CK. Treatment of triple fracture of the superior shoulder suspensory complex. J Korean Orthop Assoc 2011;46:68. [Google Scholar]
- 9.Tamimi Mariño I, Martin Rodríguez I, Mora Villadeamigo J. Triple fracture of the shoulder suspensory complex. Rev Esp Cir Ortop Traumatol 2013;57:371-4. [Google Scholar]
- 10.Yao X, Wu L, Li J, Huang W, Duan X, Gu Z, et al. Open reduction and internal fixation for multiple injuries of superior shoulder suspensory complex with coracoid process fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2020;34:347-51. [Google Scholar]