With meticulous technique, one-stage excision of massive chronic non-infected infrapatellar bursae is safe and effective.
Dr. Mohamed Abdelghany, Department of Orthopaedics, Qena General Hospital, Qena, Egypt. E-mail: maghany06@gmail.com
Introduction: Superficial infrapatellar bursitis may be traumatic, inflammatory, or infectious. It rarely attains massive dimensions. Open excision can be performed as a one-stage or a two-stage procedure, and endoscopy can be an alternative. We report a chronic, unusually massive, hemorrhagic infrapatellar bursa which we resected totally in a single stage procedure with no significant complications.
Case Report: A 65-year-old male farmer presented with a chronic massive swelling in front of the right knee which first appeared 4 years earlier and had no effect on his general condition. The mass was excised in a one-stage procedure and it was found to be a hemorrhagic bursitis. The wound healed uneventfully and, on follow-up 7 weeks later, the patient was able to perform full flexion and extension of the knee.
Conclusion: Two-stage procedures for excision are effective, but one-stage procedures are equally effective in chronic cases, provided the dissection is performed meticulously and atraumatically.
Keywords: Infra-patellar bursitis, knee mass, hemorrhagic bursitis.
The superficial infrapatellar bursa (SIPB), sometimes called the pretibial bursa [1], is a synovial-lined sac located directly anterior or slightly superior to the tibial tuberosity [2, 3], between the anterior aspect of the distal end of the patellar tendon and the subcutaneous fat [4]. It functions to reduce friction between the tibial tuberosity and the overlying skin. Superficial infrapatellar bursitis may be caused by trauma (acute or repetitive), inflammation or infection. In superficial infrapatellar bursitis, a small swelling is usually noted; a massive growth is a rare presentation [5]. Open excision of bursae in front of the knee can be performed in a one-stage or a two-stage procedure, and the use of endoscopy is a viable alternative. We report an unusually massive hemorrhagic bursitis of the SIPB, which was totally resected in a one-stage open procedure.
A 65-year-old active and otherwise healthy Egyptian farmer presented to us with a massive swelling just below the right knee (Fig. 1).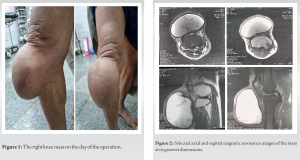
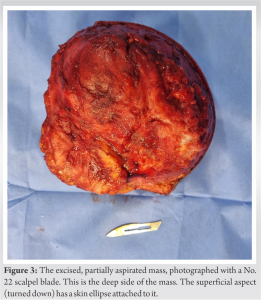


The SIPB is a synovial-lined sac located between the inferior aspect of the patellar tendon and the skin. It functions to reduce friction between the tibial tuberosity and the overlying skin. The average normal size of the SIPB is 19.5 × 21.2 × 2.2 mm [2]. Viegas et al. found the SIPB in only 55% of nine anatomic specimens (as opposed to the deep infrapatellar bursa which they detected in all their cadavres [2]. This is consistent with the figure reported about a century earlier by Churchman who described the presence of loose areolar tissue instead of the SIPB in about half of his cases [6]. When present and healthy, the SIPB, with its very minimal fluid content, is invisible on MR imaging [4, 7]. The huge collection within such a small bursa demonstrates the high stretchability of human tissues, which can sometimes reach extraordinary dimensions, even within a short time frame [5]. The SIPB is an uncommon site for bursitis [8, 9, 10], which can be either simple or hemorrhagic. Infrapatellar bursitis is more common in repetitive knee trauma, causing the best known type of superficial infrapatellar bursitis known as the “clergyman’s knee” caused by occupational kneeling. However, the etiology sometimes remains elusive [11]. Superficial infrapatellar bursitis may also be initiated by acute trauma, as in our patient, leading to hemorrhagic bursitis. With chronicity, the affected bursa may reach remarkable dimensions, producing a large mass with thick wall, loculation, and internal debris [3]. This was the case in our patient, whose hemorrhagic SIPB reached an extraordinary size. These remarkably enlarged bursae can even calcify and simulate soft-tissue tumors. Stahnke et al. reported on two octogenarian patients with calcific haemorrhagic bursitis anterior to the knee (one infrapatellar and one prepatellar) who were referred to their orthopedic oncology center for suspicion of soft-tissue sarcoma [12]. In most cases, radiological diagnosis of cystic lesions around the knee is straightforward. However, the more complex MRI appearance of chronic hemorrhagic bursitis, with atypical hemorrhagic contents and debris, differs significantly from the homogenous fluid signal seen in cases of simple bursitis [13, 14]. This may make the diagnosis of chronic hemorrhagic bursitis more challenging [15]. Skin compromise is a devastating complication following surgical excision of bursae over the anterior aspect of the knee [16], prompting the use of endoscopic [17], and two-stage open [18] procedures for these cases. Quayle and Robinson suggested excision of the posterior wall of the bursa only, leaving the anterior wall with its overlying skin undisturbed [19]. Senthilkumaran and Hamilton reported the use of the two-stage technique for the management of a large chronic prepatellar bursitis in a 62-year-old male patient [16]. However, Uçkay et al., studying cases of moderate to severe septic olecranon and prepatellar bursitis, asserted the safety, efficiency, and resource effectiveness of bursectomy with primary closure, reporting higher rates of wound dehiscence with the use of a two-stage technique for olecranon bursitis compared to the use of a one-stage technique [18]. Our patient’s wound healed uneventfully after a single-stage excision procedure.
The ability of living human tissues to expand and stretch over time is well-known and well-documented. The use of a one-stage procedure for resection of massive chronic bursae in front of the knee is safe and effective, provided the dissection is performed meticulously and atraumatically.
Living human tissues have a great ability to expand over an extended period of time. Two-stage procedures for excision are effective, but one-stage procedures are equally effective in chronic cases, provided the dissection is performed meticulously and atraumatically.
References
- 1.Bolog NV, Andreisek G, Ulbrich E. Synovium and capsule. In: MRI of the Knee: A Guide to Evaluation and Reporting. Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 2.Viegas FC, Aguiar RO, Gasparetto E, Marchiori E, Trudell DJ, Haghighi P, et al. Deep and superficial infrapatellar bursae: Cadaveric investigation of regional anatomy using magnetic resonance after ultrasound-guided bursography. Skeletal Radiol 2007;36:41-6. [Google Scholar]
- 3.Flores DV, Gómez CM, Pathria MN. Layered approach to the anterior knee: Normal anatomy and disorders associated with anterior knee pain. Radiographics 2018;38:2069-101. [Google Scholar]
- 4.Morrison JL, Kaplan PA. Water on the knee: Cysts, bursae and recesses. Magn Reson Imaging Clin N Am 2000;8:349-70. [Google Scholar]
- 5.Dharmshaktu GS, Pangtey T. How much can a small bursa stretch? A curious case of massive superficial infrapatellar bursitis in the emergency department. J Emerg Pract Trauma 2021;7:146-8. [Google Scholar]
- 6.Churchman JW. Leutic bursopathy of verneuil. Am J Med Sci 1909;138:371-96. [Google Scholar]
- 7.McCarthy EM, Murphy CL, Doran MF, Cunnane G. Infrapatellar bursitis: An occupational legacy. J Clin Rheumatol 2011;17:49-50. [Google Scholar]
- 8.Beaman FD, Peterson JJ. MR imaging of cysts, ganglia, and bursae about the knee. Magn Reson Imaging Clin N Am 2007;15:39-52. [Google Scholar]
- 9.Marra MD, Crema MD, Chung M, Roemer FW, Hunter DJ, Zaim S, et al. MRI features of cystic lesions around the knee. Knee 2008;15:423-38. [Google Scholar]
- 10.Perdikakis E, Skiadas V. MRI characteristics of cysts and “cyst-like” lesions in and around the knee: What the radiologist needs to know. Insights Imaging 2013;4:257-72. [Google Scholar]
- 11.Jain M, Nayak M, Ansari S, Patro BP. Infrapatellar bursitis presenting as a lump. BMJ Case Rep 2021;14:e243581 [Google Scholar]
- 12.Stahnke M, Mangham DC, Davies AM. Calcific haemorrhagic bursitis anterior to the knee mimicking a soft tissue sarcoma: report of two cases. Skeletal Radiol 2004;33:363-6. [Google Scholar]
- 13.Donahue F, Turkel D, Mnaymneh W, Ghandur-Mnaymneh L. Hemorrhagic prepatellar bursitis. Skeletal Radiol 1996;25:298-301. [Google Scholar]
- 14.Steinbach LS, Stevens KJ. Imaging of cysts and bursae about the knee. Radiol Clin N Am 2013;51:433-54. [Google Scholar]
- 15.Naranje S, Mittal R, Kumar A, Nataraj AR. Hemorrhagic prepatellar bursitis: A rare case report and review. Eur J Orthop Surg Traumatol 2009;19:281-4. [Google Scholar]
- 16.Senthilkumaran S, Hamilton SW. Surgical management of a large chronic prepatellar bursitis: 2-stage technique. Case Rep Orthop 2020;2020:3204014. [Google Scholar]
- 17.Huang YC, Yeh WL. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011;35:355-8. [Google Scholar]
- 18.Uçkay I, von Dach E, Perez C, Agostinho A, Garnerin P, Lipsky BA, et al. One- vs 2-stage bursectomy for septic olecranon and prepatellar bursitis. Mayo Clin Proc 2017;92:1061-9. [Google Scholar]
- 19.Quayle JB, Robinson MP. An operation for chronic prepatellar bursitis. J Bone Joint Surg Br 1976;58-B:504-6. [Google Scholar]










