Apophyseal avulsion fractures of the olecranon may not be pathognomonic of Osteogenesis Imperfecta.
Dr. Fernando Macedo, Department of Orthopaedic Surgery, Hospital Senhora da Oliveira, Guimarães, Portugal. E-mail: fe.rm@live.com.pt
Introduction: While elbow fractures are frequently observed in children, isolated apophyseal detachments of the olecranon are rare, accounting for just 1.7% of all elbow fractures in healthy children. These fractures have been found to have a large positive likelihood ratio for osteogenesis imperfecta (OI). Within the population of patients with OI, the incidence is 13.5%, with 6% sustaining bilateral fractures. There are, however, very few reports of synchronous bilateral fractures.
Case Report: A 15-year-old boy sustained a bilateral olecranon apophyse fracture, AO/OTA 21u-M/7 (displaced on the right side and minimal displacement on the left) after a low-energy fall. The patient was submitted on the same day to surgical treatment (open reduction and internal fixation with AO tension band wiring technique) on the right elbow and nonoperative treatment with a cast on the left side. Exome sequencing excluded mutations related to OI.
Conclusion: Apophyseal avulsion fractures of the olecranon may not be pathognomonic of OI, However, orthopedists should exercise caution and remain alert to the potential occurrence in patients who experience displaced, isolated olecranon fractures due to low-energy mechanisms, particularly if they have a history of previous fractures. The clinical genetic evaluation was recommended because of clinical suspicion of OI and because patient management can be significantly influenced by genetic testing, particularly when a genetic syndrome is identified.
Keywords: Olecranon apophyseal fracture, osteogenesis imperfecta, bilateral synchronous fracture.
While elbow fractures are frequently observed in children, isolated apophyseal detachments of the olecranon are rare, accounting for just 1.7% of all elbow fractures in healthy children [1]. Olecranon fractures in children are typically divided into two primary categories: Purely apophyseal fractures, commonly seen in younger children, and metaphyseal fractures, which occur in older children and involve a sizable metaphyseal fragment that is connected to the epiphysis [1]. According to Wilkins, the location of the triceps expansive insertion on the ulnar metaphysis, distal to the apophysis, probably accounts for the rarity of fracture along the apophyseal line [2]. Olecranon apophyseal fracture has been regarded as essentially pathognomonic of Osteogenesis imperfecta (OI) [3]. In children with OI, purely apophyseal fractures have been described more frequently and are characterized by an indirect mechanism of injury and an avulsion fracture, wherein the tip of the olecranon becomes detached due to a sudden contraction of the triceps brachii muscle [4,5]. Since OI affects not only bones but also ligaments and tendons [6], Zionts proposed that the vulnerability of the olecranon apophysis to avulsion in children with OI may be attributed to a combination of factors. These factors include the weakness of the subchondral bone near the growth plate of the proximal olecranon and increased laxity of the triceps expansion [7]. Zionts and Moon [7], in a retrospective review published in 2002, treated 10 children with OI who sustained olecranon apophysis fracture. One patient, who had previously suffered from asynchronous bilateral olecranon fracture, later had simultaneous refracture of both elbows while doing a pushup. Mudgal [8] in 1992 published a case report in Belgium that described a 13-year-old girl who had a proven case of OI that fell with both arms outstretched while pushing a supermarket trolley, resulting in bilateral olecranon fracture. Schweitzer [5] described a case of bilateral avulsion fracture of olecranon apophyses in a 13-year-old boy, but the author was unable to determine whether the fractures occurred simultaneously or on separate occasions. As far as the authors can tell, these were the only cases of synchronous bilateral fractures of apophyseal avulsion fractures of the olecranon described. We describe a clinical case of a 15-year-old patient with synchronous bilateral fractures, in which exome sequencing was unable to find any known mutation related to OI.
We describe a clinical case of a 15-year-old male, 174 cm tall, 62 kg, body mass index 20.5, recreational football player who was admitted to the emergency room with bilateral elbow pain after a fall back while playing football, hitting the ground with both elbows flexed simultaneously. He had no past medical history and no previous fractures. At physical examination, he presented with tenderness over the olecranon bilaterally and was unable to extend both elbows. The radiographs (X-ray) (Fig. 1) revealed bilateral olecranon apophyseal fracture AO/OTA 21u-M/7, with apophysis avulsion and displacement on the right side (Fig. 1a) with minimal displacement on the left side (Fig. 1b). The fractures occurred through the metaphyseal bone adjacent to the olecranon physis. The patient had normal teeth and sclerae. There was no known family history of OI or frequent or atypical childhood fractures.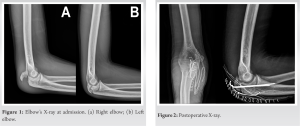
Treatment
The patient was submitted to open reduction and internal fixation with 2 K-wire and AO (Arbeitsgemeinschaft für Osteosynthesefragen) tension band wiring technique at the right side (Fig. 2) and closed treatment with immobilization in a long arm cast at 90° of flexion for 6 weeks at the left side. He was instructed to initiate a range of motion movement on the right elbow on the 1st day after surgery.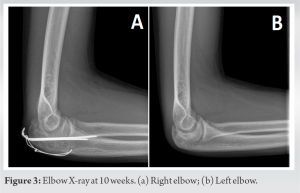
Clinical outcomes
A clinical and radiological reassessment was made weekly to allow prompt recognition of any displacement. At 6 weeks, the cast was removed on the left side, and the patient was instructed to initiate active movements toward resumption of range of motion of elbow and forearm. At 10 weeks after surgery, he had no pain or limitation of function, with full range of motion on both elbows and a DASH score of 2.5 (Fig. 3). At the 4-month follow-up, the tension band was removed due to hardware prominence. The clinical genetic evaluation was conducted because of clinical suspicion of OI and because genetic testing can often inform clinical management, especially if a genetic syndrome is identified. Exome sequencing was unable to find any known mutation related to OI. However, it showed a variant of uncertain significance (VOUS) on the STAG1 gene. The effect on protein synthesis and quaternary structure is not predictable in silico analysis (Table 1).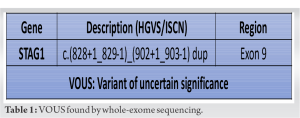
Since olecranon apophyseal fracture has been considered fundamentally pathognomonic of OI [3,9] and given it was a case of bilateral synchronous fractures with a relatively low energy trauma, we were expecting genetic analysis to confirm the diagnosis of OI. However, the only anomaly found was a VOUS in the STAG1 gene. Variants of this gene are usually associated with intellectual impairment. This specific variant had never been reported in gnomAD and ExAC (benign variation), nor in ClinVar (known pathological variation) before, and there is no literature regarding predisposition to fractures with any other variants in this gene. Displaced isolated fractures of the olecranon apophysis are very uncommon in healthy children [1,2,5,7]. These fractures have been found to have a large positive likelihood ratio for OI [10]. Tayne and Smith, in a retrospective review of 358 children with the diagnosis of OI, reported an incidence of olecranon fracture of 8.1%. Within the population of patients with OI type I, the incidence was 13.5%, with 6% sustaining bilateral fractures [9]. There are, however, very few reports of synchronous bilateral fractures. Recently, VanEenenaam et al. reviewed 403 patients with olecranon fractures in a pediatric population, in which only 14 (3.5%) had a confirmed diagnosis of OI, and suggested that isolated olecranon fractures may not be pathognomonic for OI [11]. OI is characterized by distinctive orthopedic and trauma manifestations, which include vertebral fractures, scoliosis, kyphosis, deformities of the long bones, bone fractures resulting from low-energy traumas, and spontaneous avulsions occurring at the tendon insertions [1]. We were not able to find any personal or family history of these conditions. The majority of patients clinically diagnosed with OI have a mutation in either the COL1A1 or COL1A2 genes, which encode the α chains of collagen type 1 [12]. However, there are also other less common known mutations associated with different types of OI. Furthermore, it is highly probable that there are additional genes related to this condition that have not yet been identified or reported. There is no standard method of treatment for fractures of the apophysis because few such fractures have been described. According to Rath, good long-term outcomes are achieved after nonoperative management with up to 2 mm of displacement [13]. Several studies have provided varying recommendations regarding the acceptable displacement threshold that would require open reduction, ranging between 3 and 5 mm [7]. According to Wilkins, surgical treatment is recommended when closed methods fail to achieve acceptable alignment, when there is a displacement >4 mm or if the intra-articular surface is incongruent [2]. Tension band constructs are widely recognized as the primary treatment choice for olecranon avulsion [14]. Gortzak et al. described a technique of open reduction using percutaneously placed K-wires and absorbable sutures instead of wires for the tension band [15]. However, suture tension bands have inferior failure loads and result in reduced compression at the fracture site [16]. In this case, since there was a bilateral fracture and we went for nonoperative treatment on the left side, we wanted for the patient to be able to move the right arm immediately after surgery for his comfort, so we opted for wires instead of sutures for maximum compression at the fracture site and thus avoided immobilization of both arms. The physis located at the proximal end of the ulna accounts for only 20% of the longitudinal bone growth. Given that the patient is 15 years old, arm shortening is not expected.
Apophyseal avulsion fractures of the olecranon may not be pathognomonic of OI. Nevertheless, orthopedists should remain vigilant about the possibility of OI in patients who experience displaced, isolated olecranon fractures due to low-energy mechanisms, particularly if they have a history of previous fractures. Clinical genetic evaluation was recommended because of clinical suspicion of OI and because patient management can be significantly influenced by genetic testing, particularly when a genetic syndrome is identified. With whole-exome sequencing being increasingly used, we may identify candidate genes or other novel gene variants associated with fragility fractures.
Apophyseal avulsion fractures of the olecranon may not be pathognomonic of OI, however orthopedists should remain cautious of the potential association and always refer to clinical genetic evaluation.
References
- 1.Persiani P, Ranaldi FM, Graci J, De Cristo C, Zambrano A, D’Eufemia P, et al. Isolated olecranon fractures in children affected by osteogenesis imperfecta Type I treated with single screw or tension band wiring system: Outcomes and pitfalls in relation to bone mineral density. Medicine (Baltimore) 2017;96:e6766. [Google Scholar]
- 2.Waters PM, Skaggs DL, Flynn JM. Rockwood and Wilkins’ Fractures in Children. United States: Lippincott Williams and Wilkins; 2019. [Google Scholar]
- 3.Butler BA, Lawton CD, Grayhack JJ. Olecranon fractures: Apophysis osteogenesis imperfecta. In: Pediatric Orthopedic Trauma Case Atlas. Germany: Springer; 2019. p. 1-4. [Google Scholar]
- 4.Caterini R, Farsetti P, D’Arrigo C, Ippolito E. Fractures of the olecranon in children. Long-term follow-up of 39 cases. J Pediatr Orthop B 2002;11:320-8. [Google Scholar]
- 5.Schweitzer G. Bilateral avulsion fractures of olecranon apophyses. Arch Orthop Trauma Surg (1978) 1988;107:181-2. [Google Scholar]
- 6.Kocher MS, Shapiro F. Osteogenesis Imperfecta. J Am Acad Orthop Surg 1998;6:225-36. [Google Scholar]
- 7.Zionts LE, Moon CN. Olecranon apophysis fractures in children with osteogenesis imperfecta revisited. J Pediatr Orthop 2002;22:745-50. [Google Scholar]
- 8.Mudgal CS. Olecranon fractures in osteogenesis imperfecta: A case report. Acta Orthop Belg 1992;58:453-6. [Google Scholar]
- 9.Tayne S, Smith PA. Olecranon fractures in pediatric patients with osteogenesis imperfecta. J Pediatr Orthop 2019;39:e558-62. [Google Scholar]
- 10.Peddada KV, Sullivan BT, Margalit A, Sponseller PD. Fracture patterns differ between osteogenesis imperfecta and routine pediatric fractures. J Pediatr Orthop 2018;38:e207-12. [Google Scholar]
- 11.VanEenenaam DP Jr., Houlihan N, Heyer JH, Flynn JM, Mitchell SL. When is an isolated olecranon fracture pathognomonic for osteogenesis imperfecta? J Pediatr Orthop 2022;42:e515-9. [Google Scholar]
- 12.Frank R, Glorieux FH. Osteogenesis imperfecta. Lancet 2004;363:1377-85. [Google Scholar]
- 13.Rath NK, Carpenter EC, Ortho F, homas DP. Traumatic pediatric olecranon injury: A report of suture fixation and review of the literature. Pediatr Emerg Care 2011;27:1167-9. [Google Scholar]
- 14.Karlsson MK, Hasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon during growth : A 15-25-year follow-up. J Pediatr Orthop B 2002;11:251-5. [Google Scholar]
- 15.Gortzak Y, Mercado E, Atar D, Weisel Y. Pediatric olecranon fractures: Open reduction and internal fixation with removable Kirschner wires and absorbable sutures. J Pediatr Orthop 2006;26:39-42. [Google Scholar]
- 16.Parent S, Wedemeyer M, Mahar AT, Anderson M, Faro F, Steinman S, et al. Displaced olecranon fractures in children: A biomechanical analysis of fixation methods. J Pediatr Orthop 2008;28:147-51. [Google Scholar]











