Practitioners should be mindful of the potential post-reduction complications with prompt consultation of vascular and orthopedic surgery services after prolonged vascular ischemia.
Dr. Zachary Donato, Department of Orthopaedic Surgery, University of Miami Miller School of Medicine, 1600 NW 10th Ave, Miami, Florida 33136, United States. E-mail: z.donato@med.miami.edu
Introduction: While commonly caused by traumatic injury and fracture, compartment syndrome can also result from reperfusion injury. Very few cases of prophylactic fasciotomy are mentioned when considering time to revascularization after prolonged vascular ischemia. We present a case of a patient who underwent multiple compartment prophylactic fasciotomies following reperfusion injury in the upper extremity.
Case Report: We report a 72-year-old male that suffered from an anterior shoulder dislocation after a ground-level fall. After reduction, pulses were not measurable, and angiography indicated an axillary artery occlusion. Immediately after operative reperfusion, compartments became tense. Orthopedic surgeons subsequently performed arm anterior, posterior, and forearm volar and mobile wad compartment fasciotomies, after 13 h of ischemia. The patient tolerated the procedure, and at the latest follow-up, was working to improve strength in the extremity.
Conclusion: Even when the circumstances of injury seem to be less traumatic as in this case of a ground-level fall, we document the importance of prompt recognition and intervention of suspected compartment syndrome following prolonged ischemia and revascularization of the upper extremity.
Keywords: Compartment syndrome, reperfusion injury, shoulder dislocation, axillary artery occlusion, fasciotomy.
Compartment syndrome is a surgical emergency that occurs when the pressure within a muscular compartment rises higher than the perfusion pressure. While commonly caused by traumatic injury and fracture, it can also result from reperfusion injury, which occurs secondary to inflammation that develops after blood supply is returned following prolonged ischemia [1]. His phenomenon is well documented in the lower extremity, with some indications for the consideration of prophylactic fasciotomy [2-4]. Very few cases of prophylactic fasciotomy are mentioned when considering the time to revascularization after prolonged ischemia due to arterial injury in the upper extremity [5-8]. This highlights the need for further evaluation of reperfusion injury and the indications for fasciotomy in the upper extremity. Herein, we present a case report on a patient who underwent multiple compartment fasciotomies following an axillary artery occlusion following shoulder dislocation and perform a review of the current literature on prophylactic fasciotomy for reperfusion injuries in the upper extremity.
A 72-year-old man with a past medical history of hypertension and morbid obesity presented to the emergency department immediately after sustaining a ground-level fall complaining of left shoulder pain and complete loss of sensation in his left hand. The patient had sluggish capillary refill of his left hand as well as palpable but weak radial pulse. His left shoulder and upper arm were edematous but soft with ecchymosis about the axilla. At this point, the patient was able to actively move his left arm at the elbow and wrist. Plain radiographs of the shoulder showed a left anterior shoulder dislocation with no fractures. Within 1 h of presentation, a left shoulder reduction was attempted by an emergency medicine physician under conscious sedation, but this was aborted when the patient became apneic. Immediately after this attempt, there were no palpable radial, ulnar, or brachial pulses. Both vascular surgery and orthopedic surgery were then consulted. The patient was immediately intubated and emergently taken to perform a computed tomography angiography (CTA) of the chest and left upper extremity and then to the operating room for a closed reduction. Exam under anesthesia demonstrated that the patient had full unrestricted passive shoulder range of motion, and the fluoroscopic view of the humeral head was stable to external rotation in both neutral and 90° abduction. Post-operatively, upon evaluation by vascular surgery, the left upper extremity was cool to touch and no brachial, radial, or ulnar pulses or signals could be obtained with Doppler ultrasound. The finalized interpretation of the CTA indicated left axillary and subclavian artery occlusion (Fig. 1).

Compartment syndrome is a surgical emergency that requires immediate recognition and repair with a decompressive fasciotomy. While diagnosis is clinically based, measurement of compartment pressures is a useful adjunct in equivocal cases or in those with a sedated patient. A delta pressure (diastolic-compartment pressure) <30 mmHg is highly specific for compartment syndrome. Arterial ischemia as a cause of compartment syndrome is well documented in the lower extremity; however, there are not many studies discussing its prevalence in the upper extremity. Numerous occluded arteries in the upper extremity have been documented as causes of reperfusion injury and subsequent compartment syndrome. Injury to the brachial artery specifically is a more common cause of compartment syndrome. Zellweger et al. studied 124 cases of surgically managed brachial artery injuries, and Ekim and Tuncer studied 49 patients also treated with surgical repair of brachial artery injuries [6, 7]. The rate of fasciotomy for impending or established compartment syndrome in these studies was about 12%. Other studies demonstrate ranges of compartment syndrome due to reperfusion injury in the upper extremity from 6.7% to 29.3% with multiple varying arteries occluded (Table 1) [6, 7, 9-13].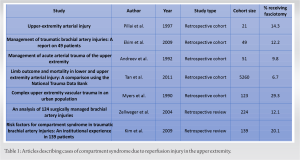
Compartment syndrome has many etiologies. It can occur after prolonged ischemia in the setting of attempted shoulder reduction with vascular compromise and delayed revascularization. A fasciotomy should be considered when there is a high index of suspicion of a reperfusion injury in the upper extremity.
Compartment syndrome must be considered in the case of prolonged vascular compromise after shoulder reduction.
References
- 1.McNally MM, Univers J. Acute limb ischemia. Surg Clin North Am 2018;98:1081-96. [Google Scholar]
- 2.Wesslen C, Wahlgren CM. Contemporary management and outcome after lower extremity fasciotomy in non-trauma-related vascular surgery. Vasc Endovascular Surg 2018;52:493-7. [Google Scholar]
- 3.Kronja G, Misovic S, Tomic A. Indications and results of fasciotomy in vascular injuries of the lower extremities. Vojnosanit Pregl 2000;57:271-6. [Google Scholar]
- 4.Hofmeister EP, Shin AY. The role of prophylactic fasciotomy and medical treatment in limb ischemia and revascularization. Hand Clin 1998;14:457-65, x. [Google Scholar]
- 5.Sayar U, Ozer T, Mataraci I. Forearm compartment syndrome caused by reperfusion injury. Case Rep Vasc Med 2014;2014:931410. [Google Scholar]
- 6.Zellweger R, Hess F, Nicol A, Omoshoro-Jones J, Kahn D, Navsaria P. An analysis of 124 surgically managed brachial artery injuries. Am J Surg 2004;188:240-5. [Google Scholar]
- 7.Ekim H, Tuncer M. Management of traumatic brachial artery injuries: A report on 49 patients. Ann Saudi Med 2009;29:105-9. [Google Scholar]
- 8.Dragas M, Davidovic L, Kostic D, Markovic M, Pejkic S, Ille T, et al. Upper extremity arterial injuries: Factors influencing treatment outcome. Injury 2009;40:815-9. [Google Scholar]
- 9.Pillai L, Luchette FA, Romano KS, Ricotta JJ. Upper-extremity arterial injury. Am Surg 1997;63:224-7. [Google Scholar]
- 10.Andreev A, Kavrakov T, Karakolev J, Penkov P. Management of acute arterial trauma of the upper extremity. Eur J Vasc Surg 1992;6:593-8. [Google Scholar]
- 11.Tan TW, Joglar FL, Hamburg NM, Eberhardt RT, Shaw PM, Rybin D, et al. Limb outcome and mortality in lower and upper extremity arterial injury: A comparison using the National Trauma Data Bank. Vasc Endovascular Surg 2011;45:592-7. [Google Scholar]
- 12.Myers SI, Harward TR, Maher DP, Melissinos EG, Lowry PA. Complex upper extremity vascular trauma in an urban population. J Vasc Surg 1990;12:305-9. [Google Scholar]
- 13.Kim JY, Buck DW 2nd, Forte AJ, Subramanian VS, Birman MV, Schierle CF, et al. Risk factors for compartment syndrome in traumatic brachial artery injuries: An institutional experience in 139 patients. J Trauma 2009;67:1339-44. [Google Scholar]
- 14.Magister S, Bridgforth A, Yarboro S. Axillary artery injury following closed reduction of an age-indeterminate anterior glenohumeral dislocation. J Orthop Case Rep 2018;8:53-6. [Google Scholar]
- 15.Bekmez S, Beken S, Mermerkaya MU, Ozkan M, Okumus N. Acute forearm compartment syndrome in a newborn caused by reperfusion after spontaneous axillary artery thrombosis. J Pediatr Orthop B 2015;24:552-5. [Google Scholar]
- 16.Ben Hammamia M, Ben Mrad M, Mleyhi S, Ziadi J, Ghedira F, Ben Omrane S, et al. Revascularization delay and complications in acute upper limb ischemia. J Med Vasc 2019;44:194-8. [Google Scholar]
- 17.Rothenberg KA, George EL, Trickey AW, Chandra V, Stern JR. Delayed fasciotomy is associated with higher risk of major amputation in patients with acute limb ischemia. Ann Vasc Surg 2019;59:195-201. [Google Scholar]











