The total scapular prosthesis in the treatment of scapular chondrosarcoma warrants the successful tumor treatment option as well as a satisfactory and favorable functional prognosis.
Dr. Nabile Himer, Oncologic Orthopaedic Surgery Unit and Upper Limb Surgery Unit, Strasbourg University Hospital, France. E-mail: nabile.himer@gmail.com
Introduction: Chondrosarcoma has the highest prevalence among the primary malignant bone tumors in adults over the age of 50, and the scapular region is the most affected anatomical site.
Case Report: We report the case of a 66-year-old female patient, with no previous medical history, who consulted for aggravating mixed, non-specific, and atraumatic pain in the right shoulder, evolving for a year. The radiological assessment, including a computed tomography (CT) scan, a magnetic resonance imaging, and a tumor CT-guided biopsy, confirmed the diagnosis of a Grade 2 chondrosarcoma. A curative surgical treatment was performed, by an extended tumor resection and simultaneous joint reconstruction by a reversed total shoulder prosthesis with a custom-made total scapular prosthesis. This option allows to maintain survival prognosis, associated with the preservation of upper limb function.
Conclusion: The results were conclusive at the curative level and very encouraging from the functional point of view with progressive and partial recovery of the articular amplitudes, allowing the preservation of patient’s autonomy and quality of life. No complications such as scapular dislocation or tumor recurrence were documented at 3-year postoperative follow-up.
Keywords: Chondrosarcoma, shoulder, total scapular prosthesis, shoulder prosthesis.
Chondrosarcomas usually develop between the fourth and sixth decades of life [1]. They account for approximately 20–25% of all bone sarcomas [2]. They most frequently affect flat bones, such as the scapula and pelvis [3]. They can present as primary or secondary tumors and also as malignant transformation of enchondromas or, more rarely, from the cartilaginous outer layer of osteochondromas [1, 3]. Their origin is not yet completely elucidated [1]. To date, it has been observed that the development of chondrosarcoma could be caused or favored by benign bone tumors such as chondromas or osteochondromas, bilateral retinoblastomas Paget’s disease, or Li-Fraumeni syndrome [4]. Conventional, clear cell, and mesenchymal and dedifferentiated chondrosarcomas are distinguished and are subdivided into three grades: I, II (the most frequent), and III, based on nuclear size, staining pattern (hyperchromasia), mitotic activity, and degree of cellularity [4]. Grade III chondrosarcoma often kills by metastasis, even if an appropriately radical operative procedure is performed with local control achieved [5]. The risk of recurrence increases with higher grades [5]. Nevertheless, surgery is the only curative treatment [4]. Several different surgical techniques have been developed for the treatment of this specific pathology. However, their main drawback is that they usually result in joint sacrifice with poor functional outcomes. The goal of this study was to report a rare case of curative surgical treatment of a scapular chondrosarcoma with reconstruction though a total scapular prosthesis.
Clinical Presentation
We report the case of a 66-year-old female patient who consulted for chronic mixed pain in the right shoulder progressively worsening during the last year. The clinical examination showed rather moderate and increased pain on mobilization, without movement limitation or palpable mass. Bony prominence palpation did not generate pain, and rotator cuff testing was negative.
Radiological Diagnosis
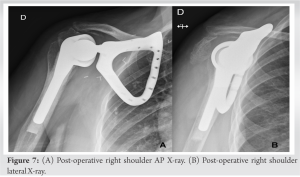
The radiological assessment included a CT scan (Fig. 1a) and a magnetic resonance imaging (MRI) (Fig. 1b and c), which showed an osteolytic lesion of the base of the neck of the scapula with a cartilaginous matrix.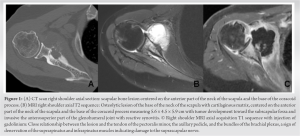
Histopathological Diagnosis
Primary bone tumor diffusely infiltrated the bone. As the pathological diagnosis required a tissue sampling, we performed a CT-guided bone biopsy which showed a Grade II chondrosarcoma.
Treatment-surgical Technique
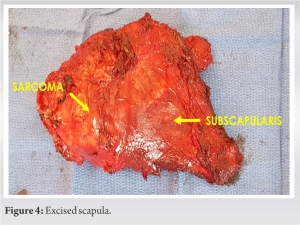
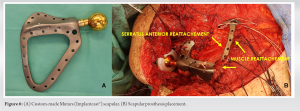
After discussion of patient’s file in a multidisciplinary meeting, the recommended therapeutic option was a total scapulectomy with extra-articular resection followed by reconstruction with custom-made scapular prosthesis and total reverse shoulder prosthesis, in a one-stage procedure. The patient was placed in left lateral decubitus, under general anesthesia (Fig. 2a). A Judet approach was performed, widened into the acromioclavicular joint (Fig. 2b). A diamond shape incision was made into the incision to completely excise the biopsy scar (Fig. 2c). Careful and progressive muscular disinsertion was performed plan by plan.


Follow-up
Shoulder was immobilized with an elbow splint for 6 weeks followed by progressive rehabilitation. At 3-year follow-up, there was a complete remission of the tumor, and the patient had a good shoulder function, allowing him independence for basic daily life activities (Fig. 8).
Chondrosarcomas are malignant bone tumors characterized by the production of neoplastic cartilage and are the second most common variety of matrix-producing malignant bone tumor [4]. They usually develop as intramedullary lesions, and they commonly affect the scapula as well as the pelvis [4]. The behavior of these tumors is inconstant, ranging from a slowly growing form with lower possibility of metastasis, to an aggressive sarcomatous form with a higher probability of metastatic transformation. They affect men and women equally and the fourth and sixth decades of life are the most common, as the patient we report [1]. Clinically, they are characterized by insidious, progressive, and long-lasting pain. Osteochondromas, which make part of the differential diagnosis, are usually asymptomatic, so patients are unaware of the existence of the lesion, so persistent and permanent pain may be the cause. A malignant transformation may occur in 5% of patients [6]. The diagnosis of scapular chondrosarcoma is radiological and histological. Several methods are used to detect these tumors, such as conventional radiography, computed tomography (CT), and MRI [7]. The radiographic appearance of chondrosarcomas, observed on CT, can help the final histopathological diagnosis, thanks to the individual characteristics of these lesions, such as their radiographically prominent endosteal nodular scalloping, the calcified matrix appears as foci of flocculent density, and mottled, “popped”, spotty or ring-like calcification of the cartilaginous matrix [2]. On the other hand, the PET scan does not have high sensitivity or specificity in the differential diagnosis of a benign and low-grade malignant chondrogenic lesion. Although, it is more efficient in identifying high-grade chondrosarcomas that show increased glucose metabolism [8, 9]. To define the best treatment for these tumors, it is important to classify them. Thus, after radiological and histological evaluation, the tumor needs to the classified into a localized and/or aggressive malignant tumor [4]. Hence, localized lesions rather are low histological grade, with little possibility of metastases. Their treatment consists of a wide resection, preserving the adjacent bone to the tumor [10]. On the other hand, aggressive cases with histological intermediate-to high-grade tumors are treated by a segmental amputation, if possible. Complete resection can heal classic lesions, avoiding the need for adjuvant radiation therapy [9]. In the present case, the malignant tumor was localized at the scapular level. Although it did not present metastasis, there was a soft-tissue invasion. To avoid a limb amputation, it was therefore decided to perform a curative surgical treatment by total resection of the tumor with a total prosthetic scapular and humeral reconstruction. Other types of surgical procedures, such as amputation and especially isolated scapulectomy and acromio-humeral arthrodesis, were excluded, due to their poor functional results. Nevertheless, it should also be noted that the role salvage surgery is yet to be clear, especially for tumor around the shoulder with often massive invasion of the proximal part of the upper limb. In this situation, the vast majority of surgeons tend to choose tumorectomy and limb amputation. However, in our case, the size and location of the tumor in the scapula, where surgical margins could be achieved and surrounding neurovascular structures remained intact. Such situation offers the possibility of tumor resection followed by reconstruction and limb salvage, using custom-made scapular and total reverse shoulder prosthesis, ensures the patient to keep the upper limb function. At 3-years post-surgery, there was no tumor recurrence or appearance of metastatic lesion. The upper limb function was satisfactory, allowing the patient to maintain her autonomy. Nevertheless, such a short follow-up does not allow us to affirm with certainty that this therapeutic approach is the best. Considered questionable by some authors, this therapeutic option can, in many cases, be the best choice in the management of these tumors and promote a favorable evolution with significant impact on the patient’s quality of life.
Chondrosarcoma is the second primary malignant bone tumor after osteosarcoma and should be thought of when located in the scapula. Chemotherapy and radiotherapy have already been used without success. The gold standard curative treatment remains surgery. The challenge in this context lies both in ensuring a complete tumor resection for the survival prognosis and a prosthetic reconstruction of the osteoarticular components for the functional prognosis. The utilized technique in the treatment of our patient warrants the successful tumor treatment as well as a satisfactory and favorable functional prognosis.
Our differential diagnostic approach regarding scapular located pain, should include the possibility of a malignant pathology. A thorough imaging and histopathological assessment will allow for the most appropriate application of treatment modality. Our surgical technique warrants limb salvage and satisfactory functional results.
References
- 1.Patel S, Benjamin R. Sarcomas ósseos e das partes moles e metástases ósseas. In: Braunwald E, Kasper DL, Fauci AS, Jameson JL, Longo DL, Hauser S, editors Harrison Medicina Interna. 17a ed. Rio de Janeiro: Mcgraw-Hill Interamericana do Brasil;2008:610-3. [Google Scholar]
- 2.de Moraes FB, Linhares ND, de Souza Domingues PM, Warzocha VN, Soares JM. Calcaneal chondrosarcoma: A case report. Rev Bras Ortop 2014;49:409-13. [Google Scholar]
- 3.Kilgore WB, Parrish WM. Calcaneal tumors and tumor-like conditions. Foot Ankle Clin 2005;10:541-65. [Google Scholar]
- 4.Board WC of TE. Soft tissue and bone tumours. In: WHO Classification of Tumours. 5th ed. France: IARC Press; 2020. [Google Scholar]
- 5.Evans H, Ayala A, Romsdahl M. Prognostic factors in chondrosarcoma of bone: A clinicopathologic analysis with emphasis on histologic grading. Cancer 1977;40:818-31. [Google Scholar]
- 6.Gomes A, Silveira C, Paiva R, Aragão A Jr., Castro J Jr. Condrossarcoma em paciente com osteocondromatose múltipla: Relato de caso e revisão da literatura. Radiol Bras 2006;39(6):449–451. [Google Scholar]
- 7.Tossato P, Pereira A, Cavalcanti M. Osteossarcoma e condrossarcoma: Diferenciação radiográfica por meio da tomografia computadorizada. Pesq Odontol Bras 2002;16:69-76. [Google Scholar]
- 8.Qiang S, Ma XN, Wang HW, Lv SC. Scapula chondrosarcoma. Medicine (Baltimore) 2019;98:e15388. [Google Scholar]
- 9.Lee FY, Yu J, Chang SS, Fawwaz R, Parisien MV. Diagnostic value and limitations of fluorine-18 fluorodeoxyglucose positron emission tomography for cartilaginous tumors of bone. J Bone Joint Surg Ame 2004;86:2677-85. [Google Scholar]
- 10.Miura K, Kondo R, Kurai M, Isobe K, Ishii K. Recurrence of juxtacortical chondrosarcoma arising on the rib. Gen Thorac Cardiovasc Surg 2016;64:170-3. [Google Scholar]