Mangled extremity leads to devastating consequences for the patient with subsequent possibility of loss of limb. Early salvage of the limb with multidisciplinary approach with Ilizarov fixation and meticulous observation can provide an excellent and satisfying outcome.
Dr. Amir Ratna Shakya, Department of Orthopaedics, Shree Birendra Hospital, Chhauni, P76R+GG6, Kathmandu 44600, Nepal. E-mail: anmishakya@hotmail.com
Introduction: Mangled is the evocative term for a grievance caused by crushing, resulting in a limb confiscation. Motor vehicle crashes and industrial/farm accidents are the leading causes of such occurrences. The verdict to reconstruct or to amputate still commonly lies with the surgical skills and experience of the treating surgeon.
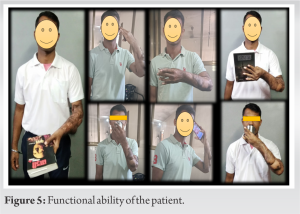
Case Report: We present a case of 33-year-old male military personnel involved in a road traffic accident who presented to our center with a mangled forearm with segmental fracture radius and fracture shaft of ulna with vascular injury. He was immediately taken up for early debridement, intramedullary fixation, vascular repair, and temporizing skin graft. After definitive soft-tissue flap coverage and a period of convalescence, the patient underwent Ilizarov external fixator application with successful rehabilitation. The patient achieved pain-free limb with functional range of motions of both elbow and wrist with functional capabilities of basic needs and activities of daily living.
Conclusion: The combination of osseous, vascular, soft-tissue, and nerve injury after severe trauma to an extremity is a great challenge in the mangled extremity. However, in young patients without significant systemic involvement and borderline injury scores, limb salvage should be attempted.
Keywords: Mangled forearm, Ilizarov, mangled extremity, vascular injury, crush injury forearm, circular fixator, multidisciplinary approach.
The modern era is witnessing a rise in road traffic accidents (RTAs) and as a result the injuries as well. As most of these injuries are caused by high-energy trauma, the incidence of mangled extremity has also increased exponentially. Historically mangled extremities were generally treated with a primary amputation. However, as a consequence of the advancement of surgical repair and reconstruction techniques, they can now be salvaged by multidisciplinary approach. Due to the absence of widely acceptable protocols, the decision to salvage or to amputate still commonly lies within the surgical judgment and experience of the treating surgeon.
A 33-year-old male, right-hand dominant soldier, was airlifted to our center with a Grade IIIC Gustilo Anderson injury of left forearm with extensive degloving injury following RTA after initial first aid at another center within a time span of 3 h. On evaluation, the patient was found to be hypotensive with ongoing blood loss from injury site. Immediate crystalloid resuscitation was initiated and cross-matched blood was requisitioned while the patient was promptly shifted to the operation theater. Mangled extremity severity score (MESS) was calculated to be 8 points (age – 1, moderate ischemia – 2, transient hypotension – 1, and skeletal and soft-tissue injury – 4). Radiograph of forearm revealed peri-implant fracture shaft radius and ulna at the proximal ends of the plates with a distal radius fracture (Fig. 1).
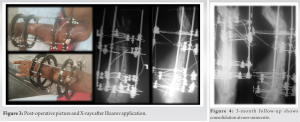
Destruction or severe damage caused by tearing or crushing of tissues in different ways leading to a complex injured limb subsequently becoming unrecognizable is described as Mangled. et al. defined a mangled extremity as an injury which usually results from major trauma and often combines significant injuries to various tissue [1]. With the advancement of trauma resuscitation, microvascular tissue transfer, and fracture fixation, there is increase in attempt to salvage these injuries, which were earlier not attempted; however, there still remains an ambiguity on the decision [2]. In cases where preserving a mangled limb however is a technical possibility, it often requires multidisciplinary approach with multiple surgeries, prolonged rehabilitation, patient compliance, and huge financial costs. Nevertheless, in some instances despite every effort, there are likely chances of morbidity and delayed amputation or mortality. Multiple scoring systems help to guide the management of complex extremity trauma but there is much debate over the criteria that can help in predicting limb salvage or better off with early amputation. Many of these predictive indices are criticized for being too subjective, complex, and difficult to apply universally. Mostly, these indices were retrospectively derived with a small patient series and no functional outcome validation [3]. The MESS was introduced by Johansen et al. in 1990 [4]. Four different factors, skeletal and soft-tissue injury, ischemia, shock, and patient age, were scored with a maximum score of 15 and a score of <7 was shown to be predictive of salvage. The proposed advantages of this predictive index were that the information required for scoring is readily available upon presentation, its relative simplicity, and reproducibility, which lead it to be the most utilized indices [5]. Rush et al. showed that small group of a combat setting the MESS was a sensitive predictor for amputation [6]. In contrast, a larger study by Brown et al. in British military patients with mangled extremity ballistic injuries found that the MESS score between 7 and 9 did not help to decide for amputation [7, 8]. In another study using the MESS system in upper-limb injuries, some cases with MESS scores >7 were successfully salvaged as published by Prichayudh et al. [9] In our case, we applied MESS score of 8, keeping in mind, that upper-limb crush injuries differ from lower limbs in terms of more muscle coverage leading to longer tolerance for ischemia and that upper limbs are responsible for a variety of complex functions that cannot be replaced by artificial limbs, the verdict for limb salvage was taken in view of young age, short duration since injury, absence of any other injury or systemic comorbidity, and the availability of specialist trauma team with orthopedic surgeon, plastic surgeon, anesthetist, and intensivist. The fact that we were dealing with a limb which had a history of previously operated both bone fractures with peri-implant fractures in a setting of ulnar artery transection made the job more complex. Early temporary fixation was based on principles of damage control orthopedics (DCO) which is a staged approach for the management of multiple injured patients presenting in an unstable state. The choice of initial intramedullary fixation and subsequent Ilizarov fixation at a later setting was also based on the fact that the patient had plate fixation on both bones earlier and peri-implant fractures were in turn due to stress riser effect of the same. The other option of primary bridge plating with longer plate was rejected as it would lead to increased soft-tissue damage, chances of infection, more weakening of bone, and increase in operative time. Similarly, soft-tissue coverage was also done by debridement and split skin graft to reduce operative time. Ilizarov fixator application was used in this case to achieve stable fixation in the presence of infection and to cause minimal damage to the already compromised soft-tissue envelope. Favorable result of the surgery in this case was achieved due to (i) prevention of systemic complications by dedicated team, (ii) Early debridement and temporary fixation and soft-tissue coverage as per DCO with the availability of well-trained trauma team, (iii) well-planned and minimal number of surgical interventions, (iv) dedicated and untiring physiotherapy, and (v) deliberate and time-to-time counseling of the patient and his family. The limitations of the treatment were the long duration of the treatment period and inability to correct the distal radius malunion completely.
Multiple tissue injuries after severe trauma to an extremity are a great challenge for any trauma center. Keeping in mind the anatomical, physiological, and functional differences between mangled injuries of upper and lower extremities, a simple scoring system that will allow a clear cut-off point for amputation versus salvage is needed. Management decisions in such cases should be patient-centric and multidisciplinary approach with additional involvement of vascular and plastic surgeon with effective planning with good post-operative rehabilitation with physiotherapy shall result in favorable and optimal outcome.
Although the literature favors amputation in severely crush extremity with MESS score of >7, an attempt to salvage the limb using multidisciplinary approach should be considered. Ilizarov circular fixator is an effective tool that can be game changing for the revival of both the soft-tissue component and bony structure.
References
- 1.Ring D, Jupiter JB. Mangling upper limb injuries in industry. Injury 1999;30:B5-13. [Google Scholar]
- 2.Prasarn ML, Helfet DL, Kloen P. Management of the mangled extremity. Strategies Trauma Limb Reconstr 2012;7:57-66. [Google Scholar]
- 3.Schirò GR, Sessa S, Piccioli A, Maccauro G. Primary amputation vs limb salvage in mangled extremity: A systematic review of the current scoring system. BMC Musculoskelet Disord 2015;16:372. [Google Scholar]
- 4.Johansen K, Daines M, Howey T, Helfet D, Hansen ST Jr. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma 1990;30:568-72, discussion 572-3. [Google Scholar]
- 5.Togawa S, Yamami N, Nakayama H, Mano Y, Ikegami K, Ozeki S. The validity of the mangled extremity severity score in the assessment of upper limb injuries. J Bone Joint Surg Br 2005;87:1516-9. [Google Scholar]
- 6.Rush RM Jr., Kjorstad R, Starnes BW, Arrington E, Devine JD, Andersen CA. Application of the mangled extremity severity score in a combat setting. Mil Med 2007;172:777-81. [Google Scholar]
- 7.Brown KV, Ramasamy A, McLeod J, Stapley S, Clasper JC. Predicting the need for early amputation in ballistic mangled extremity injuries. J Trauma 2009;66:S93-8, discussion S97-8. [Google Scholar]
- 8.Loja MN, Sammann A, DuBose J, Li CS, Liu Y, Savage S, et al. The mangled extremity score and amputation: Time for a revision. J Trauma Acute Care Surg 2017;82:518-23. [Google Scholar]
- 9.Prichayudh S, Verananvattna A, Sriussadaporn S, Sriussadaporn S, Kritayakirana K, Pak-art R, et al. Management of upper extremity vascular injury: Outcome related to the mangled extremity severity score. World J Surg 2009;33:857-63. [Google Scholar]