With good preoperative planning, iliofemoral arthrodesis can be employed as a reliable cost-effective reconstructive surgical management option for malignant of periacetabular tumors.
Dr. Sathish Muthu, Department of Orthopaedics, Government Medical College, Karur, Tamil Nadu, India. E-mail: drsathishmuthu@gmail.com
Introduction: Reconstructive options for surgical malignant of periacetabular tumors include endoprosthetic reconstructions, biologic reconstruction, hip transposition, hip rotationplasty, and iliofemoral arthrodesis. In this case series, we discuss the outcome of iliofemoral arthrodesis as a reconstruction option in the management of malignant periacetabular tumors.
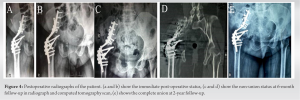
Case Report: A 45-year-old woman with complaints of right hip pain for 4-year duration was evaluated to have a well-defined radiolucent osteolytic lesion with calcifications localized around the right acetabulum diagnosed to be chondrosarcoma later on. Another 44-year-old woman with complaints of left hip pain for 2-year duration was evaluated to have fibrosarcoma of left gluteus maximus, piriformis, and gemelli extending to quadratus femoris. Wide resection was planned for both patients, and iliofemoral arthrodesis was performed. Both patients did not receive any adjuvant treatment. Both the patients demonstrated good functional outcomes at 2-years follow-up without any recurrence or distant metastasis.
Conclusion: Iliofemoral arthrodesis serves as a cost-effective reconstructive option in the management of malignant periacetabular tumors. Meticulous dissection and wide resection remain key to preventing recurrence or complications.
Keywords: Malignant tumor, arthrodesis, acetabulum, fibrosarcoma, chondrosarcoma.
Primary sarcomas of the pelvis are a relatively rare entity. Surgical management of these tumors necessitates the resection of bone and soft-tissue structures, resulting in significant morbidity to the patient [1, 2]. Enneking and Dunham classified the resection based on the region of pelvic bone being resected as shown in Fig. 1 [3, 4]. The periacetabular resection (PII) presents a unique surgical challenge where no reconstruction method has been proven to be superior to the other [5]. There is still an ongoing debate on the best reconstructive options in their management. The available surgical options include endoprosthetic reconstructions [6, 7, 8], hip transposition [9, 10], biologic reconstruction [11, 12], hip rotationplasty [13], and iliofemoral arthrodesis [14, 15]. These reconstructive procedures are associated with a higher rate of complications such as non-union, infections, implant breakage, problems associated with wound healing, and tumor recurrence [2, 16, 17]. The reported complication rate ranges from 15% to 65% [8]. The choice of the procedure should be weighed on its functional outcome against the risk of its associated complications. Limb salvage using iliofemoral arthrodesis is a rare entity and less often mentioned in literature [15]. The selection of an optimal procedure for these patients is a complex process involving factors such as the nature of the disease, residual host bone quality, patient demand, affordability, and risk of complications [5, 6]. The purpose of our study was to assess the clinical and functional outcome of iliofemoral arthrodesis as a reconstructive option in the management of malignant periacetabular tumors. We report our experience with iliofemoral arthrodesis for two cases of primary malignant periacetabular pelvic tumors.
Case 1
We present the case of a 45-year-old woman with complaints of chronic pain in her right hip for the past 4 years. She had no relevant history of trauma, infection, or other constitutional symptoms. On examination, there is a gross restriction of all ranges of movements involving the right hip. Radiological evaluation with radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) was performed to show a radiolucent osteolytic lesion in the periacetabular region with thin sclerotic rim and speckles of calcification, suggestive of low-grade chondrosarcoma as shown in Fig. 2.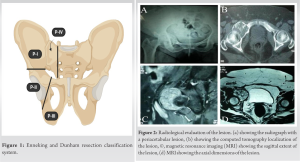

Case 2
We present the case of a 44-year-old woman with the complaints of chronic pain in the left hip for the past 2 years with associated swelling in the left gluteal region and stiffness of the hip joint. She had no relevant history of trauma, infection, or other constitutional symptoms. On examination, a swelling of size 7 × 5 cm was located in the gluteal region with gross restriction of all ranges of movement involving the left hip. Radiological evaluation with CT and MRI was performed to demonstrate a fibrosarcoma involving the left gluteus maximus, piriformis, and gemelli extending till quadratus femoris as shown in Fig. 5. Biopsy confirmed the diagnosis as shown in Fig. 6b and c. 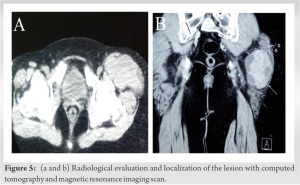

The management of tumors in the periacetabular region is a rare entity and is less often discussed. Limb-sparing surgery for periacetabular tumors is one of the most challenging procedures for surgeons [5]. There are no standard procedures indicated in these cases. Usually, the management is individualized for each patient. When adequate bone remains after resection, the proximal femur could be fused to the remaining ilium to produce a good functional outcome [15]. In our study, the clinical and post-operative characteristics are reviewed. Avoiding post-operative complications is a major factor in the outcome of the patients. The surgical procedure should provide the adequate soft-tissue coverage and minimize non-biological materials. Most series show that failure in limb-saving surgeries is mainly due to inadequate soft-tissue cover, severe muscle loss, and dead space creation. Therefore, adequate soft-tissue coverage will reduce the dead space, decrease the chances of infection, and improve post-operative clinical outcome [6, 16]. After endoprosthetic replacement, most patients suffered major post-operative complications such as infection (36%) and dislocations (27%) [19]. Hip transposition had a lower incidence of infections, but severe limb length discrepancy requiring additional limb-lengthening surgeries [9]. Furthermore, most procedures described above require a good abductor function for restoring hip kinematics. In cases where the abductors cannot be preserved, iliofemoral arthrodesis gives good results with a stable painless hip [15]. Various studies mention the advantage of a durable pain-free stable hip with less length discrepancy with iliofemoral fusion. Fujiwara et al. [19] in their study compared the clinical outcomes of various surgical treatments for periacetabular tumors and found that the best results with iliofemoral arthrodesis, attributable to a good gait performance with a stiff hip. In their study, patients who had undergone pelvic reconstruction with endoprosthesis had poor functional results and higher post-operative complications. Patients who had undergone hip transposition surgeries had lower complications rate but had high limb length discrepancy rates [19]. Enneking [3] in their study recommend iliofemoral fusion as the reconstructive procedure of choice for periacetabular tumors. Similarly, Nagoya et al. [20] also had similar results with reconstructive hip arthrodesis with added vascularized fibular grafting. Angelini et al. [21] in their study recommend that pelvic resections should be followed by reconstructive techniques with the lowest complication rate and earliest functional recovery. Hence, we consider wide excision followed by reconstruction by iliofemoral arthrodesis an effective treatment in these patients. Patients in our series had no recurrence. In our study, we consider good pre-operative planning to assess the extent of the tumor-free resection margin following meticulous dissection, adequate osteoinductive bone grating to facilitate bone union and arthrodesis, and adequate post-operative immobilization for 6–12 weeks remain the key factors that determine a recurrence-free survival with good functional outcome post- periacetabular tumor resection surgery. The procedure is not without its own set of complications. In the immediate post-operative period, patients may present with infection, and implant failure and pseudo-arthrodesis, non-union later on. In the long term, the iliofemoral arthrodesis may result in low back pain, ipsilateral knee, and contralateral hip degeneration due to the altered biomechanics at play post-surgery [22]. Hence, this procedure cannot be considered in patients with degenerative changes in the lumbar spine, ipsilateral knee or contralateral hip degeneration, or contralateral total hip arthroplasty which increased its failure rate by 40% [19]. Further, pelvic sarcomas have overall 45% survival at 5-year post-surgery due to recurrence and other aforementioned complications [1, 23]. Total hip replacement or an endoprosthetic reconstruction could be considered a salvage option in such conditions depending on the extent of the lesion that needs to be excised during the revision scenario [24, 25, 26].
Iliofemoral arthrodesis serves as a cost-effective reconstructive option in the management of malignant periacetabular tumors. Meticulous dissection and wide resection remain key to preventing recurrence or complications.
- Appropriate selection of reconstructive procedures for individual patients considering the amount of bone remaining after tumor resection and the amount of viable soft tissue to support the reconstruction is important
- Selection of patients with proper history, physical examination, radiographs, computed tomograms, and MRI is mandatory, with due consideration to the stage of the malignant tumor
- Surgeons should be aware that these procedures are technically demanding and we recommend experienced orthopedic surgeons familiar with the normal and abnormal anatomy of the acetabulum
- Wide resection followed by iliofemoral fusion decreases the chance of recurrence and helps in cost-effectively achieving a stable hip with decreased risk of infection
- Avoiding the postoperative complication rate is a major deciding factor to ensure a good functional outcome in these patients, which can be achieved by adequate soft-tissue coverage and minimizing non-biological materials.
References
- 1.Han I, Lee YM, Cho HS, Oh JH, Lee SH, Kim HS. Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg 2010;2:160-6. [Google Scholar]
- 2.Hoffmann C, Gosheger G, Gebert C, Jürgens H, Winkelmann W. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am 2006;88:575-82. [Google Scholar]
- 3.Enneking WF. Local resection of malignant lesions of the hip and pelvis. 1966. Clin Orthop Relat Res 2002;397:3-11. [Google Scholar]
- 4.Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am 1978;60:731-46. [Google Scholar]
- 5.Hugate R Jr., Sim FH. Pelvic reconstruction techniques. Orthop Clin North Am 2006;37:85-97. [Google Scholar]
- 6.Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after the excision of malignant tumours. Complications and functional outcome of prostheses. J Bone Joint Surg Br 1997;79:773-9. [Google Scholar]
- 7.Jaiswal PK, Aston WJ, Grimer RJ, Abudu A, Carter S, Blunn G, et al. Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum. J Bone Joint Surg Br 2008;90:1222-7. [Google Scholar]
- 8.Ueda T, Kakunaga S, Takenaka S, Araki N, Yoshikawa H. Constrained total hip megaprosthesis for primary periacetabular tumors. Clin Orthop Relat Res 2013;471:741-9. [Google Scholar]
- 9.Gebert C, Gosheger G, Winkelmann W. Hip transposition as a universal surgical procedure for periacetabular tumors of the pelvis. J Surg Oncol 2009;99:169-72. [Google Scholar]
- 10.Gebert C, Wessling M, Hoffmann C, Roedl R, Winkelmann W, Gosheger G, et al. Hip transposition as a limb salvage procedure following the resection of periacetabular tumors. J Surg Oncol 2011;103:269-75. [Google Scholar]
- 11.Laffosse JM, Pourcel A, Reina N, Tricoire JL, Bonnevialle P, Chiron P, et al. Primary tumor of the periacetabular region: Resection and reconstruction using a segmental ipsilateral femur autograft. Orthop Traumatol Surg Res 2012;98:309-18. [Google Scholar]
- 12.Campanacci D, Chacon S, Mondanelli N, Beltrami G, Scoccianti G, Caff G, et al. Pelvic massive allograft reconstruction after bone tumour resection. Int Orthop 2012;36:2529-36. [Google Scholar]
- 13.Winkelmann WW. Hip rotationplasty for malignant tumors of the proximal part of the femur. J Bone Joint Surg Am 1986;68:362-9. [Google Scholar]
- 14.Carmody Soni EE, Miller BJ, Scarborough MT, Parker Gibbs C. Functional outcomes and gait analysis of patients after periacetabular sarcoma resection with and without ischiofemoral arthrodesis. J Surg Oncol 2012;106:844-9. [Google Scholar]
- 15.Fuchs B, O’Connor MI, Kaufman KR, Padgett DJ, Sim FH. Iliofemoral arthrodesis and pseudarthrosis: A long-term functional outcome evaluation. Clin Orthop Relat Res 2002;397:29-35. [Google Scholar]
- 16.Hillmann A, Hoffmann C, Gosheger G, Rödl R, Winkelmann W, Ozaki T. Tumors of the pelvis: Complications after reconstruction. Arch Orthop Trauma Surg 2003;123:340-4. [Google Scholar]
- 17.Ozaki T, Hillmann A, Bettin D, Wuisman P, Winkelmann W. High complication rates with pelvic allografts. Experience of 22 sarcoma resections. Acta Orthop Scand 1996;67:333-8. [Google Scholar]
- 18.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;286:241-6. [Google Scholar]
- 19.Fujiwara T, Ogura K, Kobayashi E, Tanzawa Y, Nakatani F, Chuman H, et al. Clinical outcomes of surgical treatments for primary malignant bone tumors arising in the acetabulum. Sarcoma 2015;2015:430576. [Google Scholar]
- 20.Nagoya S, Wada T, Kawaguchi S, Kaya M, Takebayashi T, Yamashita T. Functional results of reconstructive hip arthrodesis for periacetabular malignant tumor. Eur Orthop Traumatol 2012;3:121-5. [Google Scholar]
- 21.Angelini A, Drago G, Trovarelli G, Calabrò T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: An analysis of 270 patients from one institution. Clin Orthop Relat Res 2014;472:349-59. [Google Scholar]
- 22.Karol LA, Halliday SE, Gourineni P. Gait and function after intra-articular arthrodesis of the hip in adolescents. J Bone Joint Surg Am 2000;82:561-9. [Google Scholar]
- 23.Puchner SE, Funovics PT, Böhler C, Kaider A, Stihsen C, Hobusch GM, et al. Oncological and surgical outcome after treatment of pelvic sarcomas. PLoS One 2017;12:e0172203. [Google Scholar]
- 24.Aderinto J, Lulu OB, Backstein DJ, Safir O, Gross AE. Functional results and complications following conversion of hip fusion to total hip replacement. J Bone Joint Surg Br 2012;94:36-41. [Google Scholar]
- 25.Çalbıyık M. Total hip arthroplasty following arthrodesis: A single-center experience of 17 patients. Ther Clin Risk Manag 2018;14:659-64. [Google Scholar]
- 26.Kitagawa Y, Ek ET, Choong PF. Pelvic reconstruction using saddle prosthesis following limb salvage operation for periacetabular tumour. J Orthop Surg (Hong Kong) 2006;14:155-62. [Google Scholar]