Distal humeral epiphyseal separation in a neonate can be diagnosed with the abnormal position of the olecranon and the articulation of the radius with the medial humeral condyle.
Dr. Nikolaos Laliotis, Department of Orthopaedics, Inter Balkan Medical Centre, Asklipiou 10, 570 01, Pylaia, Thessaloniki, Greece. E-mail:nicklaliotis@gmail.com
Introduction: Epiphyseal separation of the distal humeral epiphysis is an extremely rare injury. Both clinical and radiological examinations are unclear and delayed diagnosis is reported. The absence of the ossification center of the capitellum complicates the radiological diagnosis and often it is reported as elbow dislocation.
Case Report: We are reporting a case of a distal humeral epiphysis separation, diagnosed in the maternity hospital. The neonate had severe discomfort and reduced mobility of the affected arm. We confirmed the diagnosis with the conventional radiological examination, with the medial displacement of the olecranon and the articulation of the radius with the medial humeral condyle. We performed immediate reduction of the lesion and evaluated the restoration of the normal elbow anatomy with the correct articulation of the radius with the lateral humeral condyle. The neonate was followed for a year and there is normal development of the affected elbow.
Conclusion: Knowledge of this rare neonatal fracture is essential to diagnose properly the lesion. Plain radiographic evaluation enabled us to diagnose the epiphysiolesthesis. We have treated our neonate with no invasive procedures and the final result was the normal development of the elbow joint.
Keywords: Distal epiphyseal separation humerus, neonate, Salter-Harris epiphysiolesthesis, radiological diagnosis.
Traumatic lesion of the distal humeral epiphysis is an extremely rare injury in a neonate. There are only sporadic case reports of this lesion, which are often delayed in diagnoses [1, 2, 3]. The affected arm presents reduced mobility. Severe discomfort of the neonate during any change of clothing and swelling of the elbow is the main clinical signs. In case of an uncomplicated normal delivery, signs of irritability can alert the neonatologist who is trying to investigate the type of lesion of the neonate. Clinical examination reveals painful and reduced mobility of the elbow. Radiographic examination reveals alteration of the normal elbow anatomy, which is often missed or misdiagnosed as elbow dislocation [3, 4, 5]. Since the capitellum epiphysis is not ossified in a neonate, this complicates the diagnosis. Ultrasound examination is helpful and magnetic resonance imaging (MRI) examination is often required to establish the correct diagnosis [6, 7, 8]. The lesion affects the growth plate of the distal part of the humerus and adequate reduction is important for the normal development of the elbow in later life [2]. We present a clinical case of epiphysiolesthesis of the distal humerus diagnosed through plain radiological examination in a maternity hospital. Appropriate evaluation of the radiographs enabled us to perform an immediate reduction of the lesion and confirm the restoration of the normal joint anatomy. The elbow had a normal development.
A request for evaluation was sent to a pediatric orthopedic surgeon, regarding the examination of a female neonate, on the 3rd day of life, in a maternity hospital. She was the first child of the family, who was born through normal delivery at 35 weeks of gestation with birth weight of 3100 g without referred complications from the obstetrician. The neonate was experiencing continuous discomfort and was crying in the neonatal ward. Parents were alarmed because of the continuous irritability of the neonate. The neonatologist spotted reduced mobility of the left arm and suggested that it could be a case of partial brachial plexus palsy. On examination, the neonate was irritable and severe exaggeration of pain was noticed during the movements of the removal of her clothes. The left elbow was swollen. It was impossible to perform elbow movements as the neonate was crying. An AP X-ray of the upper affected arm was performed. This showed the distorted anatomy of the neonate’s elbow joint. The olecranon was medially shifted, and the radius head appeared to articulate with the medial humerus condyle. There were no ossification centers of the elbow joint. No fracture of the humerus shaft was apparent (Fig. 1).

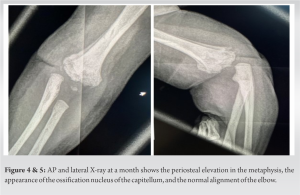
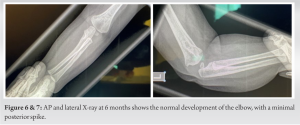
Neonatal transphyseal separation of the distal humerus epiphysis is a rare injury, with sporadic case reports presented in the literature. There is in total a small number of cases reported. Neonatal bone injuries are usually expected in urgent cesarean deliveries or in difficult vaginal labor, where types of violent maneuvers have been performed to complete the birth procedure [9, 10]. Increased birth weight is the most frequently identified risk factor. Moreover, an inverse association between fracture rate and level of experience and academic qualification has also been reported [11]. However, the etiology occasionally remains unclear, as reported in 227 of the 1174 neonates with fractures (19%), where no cause for the fracture could be found; obvious trauma during birth or congenital bone disease was excluded from the study [12]. In our patient, the obstetrician revealed that she has not encountered severe difficulties, and she considered the labor as an uncomplicated one. In the absence of clear violent maneuvers, we cannot confirm the accidental etiology of the lesion. Immediate diagnosis is rare and the clinical signs may be obscure in the initial presentation. Reduced mobility of the upper limb in a neonate is usually the result of brachial plexus palsy or neonatal fracture. Neonatal fractures in the absence of difficult labor may be considered in cases of neonatal bone fragility, like in osteogenesis imperfecta. Septic arthritis, which is usually affecting the shoulder, is a complication in premature neonates, who are intubated in ICU that appear after a period of hospitalization in the ICU. Diagnosis is difficult and it must be considered in all cases of reduced mobility of the limb. The case of battered child was excluded as the neonate was constantly under supervision in the maternity hospital [2, 8, 13]. The distal humeral epiphysis ossifies later than 6–8 weeks and the distal humeral epiphysis is not visible on X-ray [3]. However, appropriate evaluation of the medial displacement of the olecranon and the alignment of the radius with the medial humerus condyle are indicators of the distorted anatomy of the elbow. Lateral X-rays do not clearly indicate the lesion, in cases with mild displacement. Beckmann and Crawford reported a 2-day-old neonate with grossly displaced bones who had a suspicious image of an elbow dislocation but was instead a Salter-Harris lesion of the distal humeral epiphysis [4]. The relation of the capitellum with the radial head is the most important parameter inevaluating the elbow region in a neonate. The capitellum ossifies from 1 to 26 months [14]. Since congenital elbow dislocation has not been reported, we established the diagnosis of distal humeral epiphysiolesthesis. Radiological examination may be initially interpreted as normal, as reported by Gigante et al. in one of their cases [2]. Another premature neonate in the same cohort was diagnosed with elbow dislocation. The diagnosis was missed in four out of six children, in the series reported by Jacobsen, with a delayed diagnosis 9–30 days after discharge from the maternity hospital [5]. Radiological evaluation of transphyseal fractures of the distal humerus affecting toddlers was proposed based on the presence of ossification of the secondary ossification center of the capitellum [15, 16]. Three groups were recorded: Group A in the absence of ossification, occurring in patients <9 months; Group B with a small metaphyseal fragment; and Group C with a bigger fragment. Our neonate belongs to Group A. In a large retrospective study by Hariharan et al., the authors reported 79 patients, with transphyseal humeral separation, aged 0–46 months. They reported that plain radiographs were sufficient in making diagnosis in majority of the cases. They elaborated that the commonly used radiographic markers, such as the anterior humeral line and the radiocapitellar line, are not helpful in the absence of the capitellar ossification center [17]. Different results were reported from the series of Supakul et al., where the diagnosis of distal humeral epiphyseal separation was missed in nine of the 16 patients [3]. Ultrasonography is helpful, considering the difficulties encountered in diagnosis [3, 6]. The cartilaginous epiphysis can be detected in an abnormal position related to the metaphysis. The examination requires an experienced radiographer and cannot be easily interpreted with the surrounding edema. Inaccurate ultrasound diagnosis was reported [2]. The uncooperative neonate, who is crying and agitated, further increases the difficulties [17]. MRI is the most accurate examination and can be performed with the appropriate splinting of the elbow, along with the cooperation of the parents. Sagittal and coronal planes are used to demonstrate the separation of the distal epiphysis [8]. We have previously described the use of MRI to detect the epiphysiolisthesis of the distal femoral epiphysis in a neonate. In our neonate, there was a clear diagnosis combining the clinical and radiological result [18]. With the increased anxiety of the family and the calmness of the neonate, considering the emergency of the condition, we performed an immediate gentle reduction without delay, because of the absence of MRI in the maternity hospital, and the neonate would have to be transferred to another hospital for the MRI examination. Delayed diagnosis has been reported. Supakul et al. report on two neonates, born by cesarean section without complications, who were brought back in 7 and 10 days after discharge, because of decreased movements of the arm. Another neonate born through an uncomplicated vaginal delivery was returned to the hospital in 2 weeks time. These neonates had been treated only with immobilization of the elbow and are reported as good clinical results with full range of motion [3]. Gentle reduction is the most common reported method of treatment, with immobilization in a cast. Reduction may require anesthesia, but in the recent cases, in the 1st days of injury, probably in the first 5–6 days, reduction is easily achieved [2, 5, 14]. On X-ray, there is reestablishment of the normal elbow anatomy with the radius pointing to the lateral humerus condyle and normal lateral x-ray without suspicion of the type of elbow dislocation. Immobilization in a simple bandage has been reported [19], but we feel that the cast provides better initial stability in the coronal plane, than a simple collar n cuff with 90o of elbow flexion. Unstable cases with delayed diagnosis have been reported to require stabilization with K wire [8]. Patil and Palled reported the use of K-wire in an unstable case in a 3-day-old neonate [6]. An arthrogram was performed intraoperatively, to assist in the diagnosis and confirm reduction [4]. Tan et al. reported a case of displacement of the epiphysis in the anterior subcutaneous tissue in the elbow, threw the brachialis muscle, like a buttonhole. They also used K wire to stabilize the lesion [20]. In general, epiphyseal injuries Salter-Harris Type 2, are stable when appropriately reduced and the use of K-wire must be used with caution in the neonatal period. For late diagnosed injuries, in toddlers, there are reports for an open reduction followed with K wire fixation [16, 17, 21]. There are reports that untreated cases of distal humeral epiphysiolesthesis have adequate remodeling, but development of cubitus varus has also been observed [5]. There is the possible danger of permanent damage of the distal physeal growth plate in cases of forceful reductions in late-diagnosed injuries. Open reduction is hardly justified in late cases, as reported by Gigante et al. in their series [2, 7]. Accurate radiological confirmation of the reduction can be recorded based on the anatomical reduction of the position of the radius with the lateral humerus condyle. We used this rule, and we had adequate reduction of the injury.
Epiphysiolisthesis of the distal humerus epiphysis is an extremely rare injury, so delay in diagnosis is not uncommon. Appropriate clinical evaluation is useful to localize the lesion in the elbow. Although radiological examination has similarities with elbow dislocation, this is not reported in neonates. Hence, the anatomical alteration of the alignment of the articulation of the radius with the lateral humeral condyle is very helpful. The use of ultrasound and MRI, in doubtful cases, further establishes the diagnosis. Reduction and immobilization for a period of 3 weeks have a very satisfying outcome. Intervention with the use of K-wire has been reported in unstable cases. Late-diagnosed cases are reported to have acceptable results due to the remodeling process.
Epiphysiolesthesis of the distal humeral epiphysis is a rare fracture in a neonate, presented with severe discomfort and reduced mobility of the affected arm. Plain radiographic evaluation with the medial displacement of the olecranon and the articulation of the radius with the medial humeral condyle, confirm the diagnosis. Immediate reduction and radiographic confirmation of the correct anatomical correlations are the appropriate treatment.
References
- 1.Mane PP, Challawar NS, Shah H. Late presented case of distal humerus epiphyseal separation in a newborn. BMJ Case Rep 2016;2016:bcr2016215296. [Google Scholar]
- 2.Gigante C, Kini SG, Origo C, Volpin A. Transphyseal separation of the distal humerus in newborns. Chin J Traumatol 2017;20:183-6. [Google Scholar]
- 3.Supakul N, Hicks RA, Caltoum CB, Karmazyn B. Distal humeral epiphyseal separation in young children: An often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR Am J Roentgenol 2015;204:W192-8. [Google Scholar]
- 4.Beckmann NM, Crawford L. Salter-Harris I fracture of the distal humerus in a neonate: Imaging appearance of radiographs, ultrasound, and arthrography. Radiol Case Rep 2017;12:571-6. [Google Scholar]
- 5.Jacobsen S, Hansson G, Nathorst-Westfelt J. Traumatic separation of the distal epiphysis of the humerus sustained at birth. J Bone Joint Surg Br 2009;91:797-802. [Google Scholar]
- 6.Patil MN, Palled E. Epihyseal separation of lower end humerus in a neonate-diagnostic and management difficulty. J Orthop Case Rep 2015;5:7-9. [Google Scholar]
- 7.Varghese J, Teng M, Huang M, Balsam D. Birth injuries to growth plates: A sheep in wolves’ clothing. J Clin Ultrasound 2017;45:511-4. [Google Scholar]
- 8.Kay M, Simpkins C, Shipman P, Whitewood C. Diagnosing neonatal transphyseal fractures of the distal humerus. J Med Imaging Radiat Oncol 2017;61:494-9. [Google Scholar]
- 9.Von Heideken J, Thiblin I, Högberg U. The epidemiology of infant shaft fractures of femur or humerus by incidence, birth, accidents, and other causes. BMC Musculoskelet Disord 2020;21:840. [Google Scholar]
- 10.Högberg U, Fellman V, Thiblin I, Karlsson R, Wester K. Difficult birth is the main contributor to birth-related fracture and accidents to other neonatal fractures. Acta Paediatr 2020;109:2040-8. [Google Scholar]
- 11.Rehm A, Promod P, Ogilvy-Stuart A. Neonatal birth fractures: A retrospective tertiary maternity hospital review. J Obstet Gynaecol 2020;40:485-90. [Google Scholar]
- 12.Groenendaal F, Hukkelhoven C. Fractures in full-term neonates. Ned Tijdschr Geneeskd 2007;151:424. [Google Scholar]
- 13.Malik S, Khopkar SR, Korday CS, Jadhav SS, Bhaskar AR. Transphyseal injury of distal humerus: A commonly missed diagnosis in neonates. J Clin Diagn Res 2015;9:SD01-2. [Google Scholar]
- 14.Ratti C, Guindani N, Riva G, Callegari L, Grassi FA, Murena L. Transphyseal elbow fracture in newborn: Review of literature. Musculoskelet Surg 2015;99 Suppl 1:S99-105. [Google Scholar]
- 15.DeLee JC, Wilkins KE, Rogers LF, Rockwood CA. Fracture-separation of the distal humeral epiphysis. J Bone Joint Surg Am 1980;62:46-51. [Google Scholar]
- 16.Zhou W, Canavese F, Zhang L, Li L. Functional outcome of the elbow in toddlers with transphyseal fracture of the distal humerus treated surgically. J Child Orthop 2019;13:47-56. [Google Scholar]
- 17.Hariharan AR, Ho C, Bauer A, Mehlman CT, Sponseller PD, O’Hara N, et al. Transphyseal humeral separations: What can we learn? A retrospective, multicenter review of surgically treated patients over a 25-year period. J Pediatr Orthop 2020;40:e424-9. [Google Scholar]
- 18.Laliotis N, Kapetanakis S, Gkasdaris G, Konstantinidis P, Karoutsou R, Chourmouzi D, et al. Salter-Harris Type II fracture of the distal femur in a newborn: Acute anatomic imaging alterations after labor dystocia. Clin Case Rep 2019;7:1450-1. [Google Scholar]
- 19.Catena N, Sénès FM. Obstetrical chondro-epiphyseal separation of the distal humerus: A case report and review of literature. J Perinat Med 2009;37:418-9. [Google Scholar]
- 20.Tan W, Wang FH, Yao JH, Wu WP, Li YB, Ji YL, et al. Percutaneous fixation of neonatal humeral physeal fracture: A case report and review of the literature. World J Clin Cases 2020;8:4535-43. [Google Scholar]
- 21.Anari JB, Arkader A, Spiegel DA, Baldwin KD. Approaching unusual pediatric distal humerus fracture patterns. J Am Acad Orthop Surg 2019;27:301-11. [Google Scholar]