Operative treatment of femur fractures on a fracture table with concomitant use of traction pose a risk of genito-perineal soft tissue injuries and pudendal nerve palsy. To reduce the risk of injury, it is crucial to ensure that the post is adequately padded and to evaluate the patient's perineal skin before the procedure. Furthermore, after the treatment, it is essential to assess the patient for any sensory issues or perineal soft tissue insult, as these injuries are more common than previously thought and should not be overlooked.
Dr. Sitansu Sekhar Samantaray, Junior Resident, Department of Orthopaedics Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai Maharashtra, India. Email: situ749@gmail.com
Introduction: A fracture table with a perineal post for counter traction is frequently used in the surgical treatment of lower limb fractures. Nevertheless, persistent use of the perineal post has been linked to serious side effects. We discuss our experience treating genitoperineal wounds due to traction table.
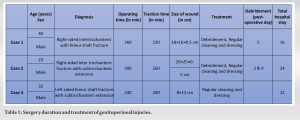
Methods: During a month, our facility treated 3 patients who had genitoperineal injuries related to the usage of a traction table. We assessed the clinical appearance of these perineal injuries, the length of the operation, the treatment strategy, the clinical results, and the length of the hospital stay.
Results: After surgery, partial thickness necrosis in the region including the scrotum and perineum developed in all patients. Two patients who had necrotic tissue infections received surgical debridement. In all cases, the wound healed fully with secondary intention by continued cleaning, dressing, and appropriate antibiotics.
Conclusion: Genitoperineal skin necrosis caused by a perineal traction post necessitates surgical debridement and prolongs hospitalization. Orthopaedicsurgeons should utilize several techniques such as proper perineal post diameter, length of surgery, positioning of the limb during surgery, etc. to lower the likelihood of this problem.
Keywords: Traction table, perineal post, necrosis, perineum, debridement, secondary intention healing.
The orthopaedic fracture table is widely used in conjunction with the perineal post for successful traction, counter traction, and immobilization in the surgical care of lower extremities and pelvic fractures [1]. For almost all diaphyseal fractures of the lower extremities, interlocking intramedullary nailing has emerged as the preferred technique [2]. The coaxial alignment and intramedullary nail insertion are made easier by the perineal post, an efficient counter-traction device [3]. Estimating the magnitude of the traction applied is done indirectly by noting distraction at the fracture site and determining the soft-tissue tension at the knee posteriorly by attempting knee flexion. However, a fracture table with a perineal post for traction and counter traction is associated with significant complications such as perineal pressure sore, pudendal nerve injury causing erectile dysfunction, and urethral injuries if not used properly.
We present a series of 3 patients who were operated at our institution in December 2022. All were operated with closed reduction and proximal femoral nailing to achieve osteosynthesis. All three patients had complex femoral fractures, resulting in difficult reduction and longer operative time. Post operatively these patients developed genitoperineal pressure sore due to counter traction at the perineal post. We involved plastic surgeons for soft-tissue management and the wound healed completely by secondary intention with regular cleaning and dressing with appropriate antibiotics (Table).
Case 1
A 40-year male suffered significant trauma to his right thigh by slip and fall resulting in displaced reverse inter-trochanteric femur fracture with the ipsilateral shaft of femur fracture (Fig. 1). Skin traction followed by closed reduction and proximal femoral nailing was done on post-trauma day 7 with the patient in the supine position using traction and counter traction by the perineal post.
Case 2
A 23-year male suffered significant trauma by fall from a height resulting in right-sided inter trochanteric fracture with subtrochanteric extension (Fig. 4). Skin traction followed by closed reduction and proximal femoral nailing was done on post-trauma day 11 with the patient in the supine position using counter traction at the perineal post. Operative time was 300 min and the patient was on traction for 260 min. Following surgery perineal skin peeling was noted 120 min post operatively; following which an ulcer developed and then a slough appeared. No erectile dysfunction or voiding issues were reported. Surgical debridement was done on post-operative day 3 (ulcer size 20 × 25 × 0.5 [Fig. 5]) and 9 and culture sensitivity was sent and antibiotics were started as per sensitivity. With regular cleaning and dressing healthy granulation appeared and the ulcer healed (Fig. 6). Patient was discharged and followed up regularly for wound cleaning and dressing.
Case 3
A 32-year male sustained trivial trauma by slip and fall while running resulting in a femur shaft fracture with subtrochanteric extension (Fig. 7). Skin traction with closed reduction and proximal femoral nailing was done. Operative time was 240 min and the patient was on traction for 200 min. In the immediate post-operative period perineal erythema and edema (Fig. 8) appeared followed by a superficial skin ulcer of size 8 × 12 cm (Fig. 9) on the scrotum on post-operative day 2. Regular cleaning and dressing were done as advised. The patient was discharged on post-operative day 12 after suture removal and followed up regularly for 1 week for cleaning and dressing. Complete healing was demonstrated by the 18th day post operatively.
The most frequent side effects of the perineal post-traction are erectile dysfunction and pudendal nerve palsy. The occurrence is yet unknown; however, it’s thought to be between 1.9% and 15% [4, 5, 6, 7]. Just four studies on perineal skin necrosis caused by a traction table have been documented in the English literature [1, 6, 8, 9]. These patients experienced various degrees of skin necrosis, from superficial, partial-thickness perineal necrosis in a few localized locations to severe, deep cutaneous necrosis. Several surgical debridements, dressing changes, and broad-spectrum antibiotics were used to treat skin wounds. Operating times were lengthy and prolonged for these 3 patients (260, 300, and 240 min) resulting in prolonged traction against the perineal post. Kosia et al. acknowledged that the most significant factors contributing to the onset of pressure-induced tissue necrosis are elevated pressures and extended exposure to these high pressures [10]. Prior research by Topliss et al. demonstrated that microscopic tissue damage occurs when tissue pressures of 70 mm Hg are applied for 2 h [10, 11]. The average operative time of <120 min is safe to avoid perineal injuries. The use of intermittent traction is also another option to adopt in a prolonged surgery to avoid such complications. Many studies have examined the use of various padding kinds, perineal post diameters, and limb placements to measure pressure on the perineum due to the traction post [11, 12, 13]. Kruger et al. and Toolan et al. discovered that 10° of leg adduction in the afflicted leg and 45° of leg abduction in the opposite leg greatly increased and practically doubled the perineal counter traction force. Nevertheless, with no difference in the location of the perineal post in the ipsilateral and contralateral sides, 20° of abduction of the injured leg reduced the counter-traction force by half. The contralateral leg’s flexion, abduction, and external rotation were used to apply the least amount of pressure on the perineum while the post was positioned near the contralateral limb. When the perineal post was positioned ipsilateral to the injured limb, this pressure decrease was not seen with this procedure [12, 13]. Experiments by Topliss et al. also showed that, although the padding material was unimportant, lower pressures were attained using large-diameter paddings (10 cm) [11].
The preventive measures to avoid such complications are:
- Use perineal post of 10 cm and more in diameter [4, 11]
- Adduction of the injured limb is to be avoided [12, 13]
- Position the patient with the post positioned contralateral to the injured leg and the affected leg abducted 20°, or with the contralateral limb flexed, abducted, and externally rotated [12, 13]
- Full relaxation during anesthesia [4, 8, 9]
- Use of pre-operative traction to maintain length and to ease intra-operative reduction [4]
- Surgical planning beforehand to reduce the operative time [9]
- Intermittent traction release in prolonged procedures requiring high traction forces [8]
- Use of AO fracture distractors as an alternative to regular traction and counter traction at the perineal post [14]
- Use of manual traction [15].
- Use of alternate positioning technique to avoid the use of perineal post
- Use of pressure sensing perineal post
- Less time to be taken for cleaning and drapping
- Use of flexible reamer
The use of fracture table and traction-counter traction at the perineal post is common place in the majority of the orthopedics procedures of the lower limb. A better understanding of the basics of perineal post application, placement, padding, and traction periods can prevent ghastly complications such as perineal sore, pudendal nerve palsy, and urethral injuries. We report a case series of 3 patients with genitoperineal sores, the least common complication of perineal post usage, which went on heal completely with surgical debridement, regular cleaning and dressing at an average of 35 days post operatively.
Perineal sore as a complication of the use of a fracture table is not common but increases morbidity and mortality. Genito-perineal injuries subject the patient to increased hospital stays and expose the patient to an increased risk of hospital-acquired infections. It also results in delayed ambulation, further amplifying the risk of deep vein thrombosis complications like pulmonary thromboembolism. These pressure sores can cause cross-infection of the surgical site adding to the morbidity, mortality and hospital stay in these patients. It is necessary to know how to avoid such complications.
References
- 1.Hammit MD, Cole PA, Kregor PJ. Massive perineal wound slough after treatment of complex pelvic and acetabular fractures using a traction table. J Orthop Trauma 2002;16:601-5. [Google Scholar]
- 2.Winquist RA, Hansen ST Jr., Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am 1984;66:529-39. [Google Scholar]
- 3.Coelho RF, Gomes CM, Sakaki MH, Montag E, Guglielmetti GB, de Barros Filho TE, et al. Genitoperineal injuries associated with the use of an orthopedic table with a perineal posttraction. J Trauma 2008;65:820-3. [Google Scholar]
- 4.France MP, Aurori BF. Pudendal nerve palsy following fracture table traction. Clin Orthop Relat Res 1992;276:272-6. [Google Scholar]
- 5.Burgess AR. Intramedullary Fixation of Subtrochanteric Fractures. In: Paper Presented at: East Coast Resident Program, Baltimore, Maryland; 1999. [Google Scholar]
- 6.Kao JT, Burton D, Comstock C, McClellan RT, Carragee E. Pudendal nerve palsy after femoral intramedullary nailing. J Orthop Trauma 1993;7:58-63. [Google Scholar]
- 7.Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am 1992;74:1450-5. [Google Scholar]
- 8.Callanan I, Choudhry V, Smith H. Perineal sloughing as a result of pressure necrosis from the traction post during prolonged bilateral femoral nailing. Injury 1994;25:472. [Google Scholar]
- 9.Peterson NE. Genitoperineal injury induced by orthopedic fracture table. J Urol 1985;134:760-1. [Google Scholar]
- 10.Topliss CJ, Webb JM. Interface pressure produced by the traction post on a standard orthopaedic table. Injury 2001;32:689-91. [Google Scholar]
- 11.Kruger DM, Kayner DC, Hankin FM, Falahee MH, Kaufer H, Matthews LS, et al. Traction force profiles associated with the use of a fracture table: A preliminary report. J Orthop Trauma 1990;4:283-6. [Google Scholar]
- 12.Toolan BC, Koval KJ, Kummer FJ, Goldsmith ME, Zuckerman JD. Effects of supine positioning and fracture post placement on the perineal countertraction force in awake volunteers. J Orthop Trauma 1995;9:164-70. [Google Scholar]
- 13.Baumgaertel F, Dahlen C, Stiletto R, Gotzen L. Technique of using the AO-femoral distractor for femoral intramedullary nailing. J Orthop Trauma 1994;8:315-21. [Google Scholar]
- 14.Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am 1992;74:1450-5. [Google Scholar]
- 15.Karpos PA, McFerran MA, Johnson KD. Intramedullary nailing of acute femoral shaft fractures using manual traction without a fracture table. J Orthop Trauma 1995;9:57-62. [Google Scholar]