Intramuscular hemangiomas of the forearm are a rare condition that should be evoked by orthopedic surgeons in front of pain and swelling of this region.
Amal Abayed, Orthopedics Kassab Institute, 2010 Ksar Said La Manouba, Tunis Faculty of Medicine, Manar University, Tunisia. E-mail: amal.abayed@gmail.com
Introduction: Hemangiomas are common benign vascular tumors. Intramuscular hemangioma is a very rare type of hemangioma occurring in the skeletal muscle. The lower limb muscles are more likely to be affected. The location within the muscles of the forearm is extremely rare.
Case Report: We present three cases of intramuscular hemangioma of the upper limb. Magnetic resonance imaging (MRI) revealed a vascular tumor within the pronator teres muscle in two cases and the extensor pollicis brevis muscle in the other. The tumors were surgically excised, and histopathologic examination confirmed the diagnosis of intramuscular cavernous hemangioma. The limb function was good and there was no recurrence at 12-month follow-up in the three cases.
Conclusion: Intramuscular hemangiomas of the forearm are a condition that should be evoked by orthopedic surgeons in front of pain and swelling of this region. MRI is the most effective imaging method to suspect the diagnosis.
Keywords: Cavernous hemangioma, muscles, upper limb, case report.
Intramuscular cavernous hemangioma is a benign vascular tumor located in skeletal muscles. It is a very rare tumor arising in <1% of diagnosed hemangiomas [1]. The lower limb muscles are more likely to be affected. Most cases are often asymptomatic, as the tumor is usually painless, lacks skin lesions, and grows slowly. It may pose a diagnostic challenge. When they are limited in size, wide local excision is a treatment of choice. We report hereby three cases of an intramuscular cavernous hemangioma of the forearm muscles.
Case 1
Patient information
An 18-year-old girl, without medical history, presented to our hospital with a painful mass of the anteromedial aspect of the left elbow (Fig. 1a). The pain worsened with exercise. The mass has been growing gradually over a year, without trauma history.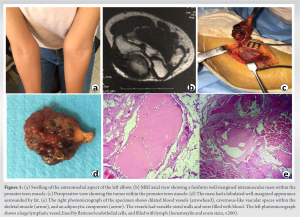
Clinical findings
Physical examination found a painful fixed soft mass in the anteromedial aspect of the elbow with a regular surface. The mass size was approximately 30 × 10 mm without clear boundaries. No changes in the covering skin or pulsion were observed. No palpable axillary lymph nodes were found. The joint range of motion and neurological examination were normal.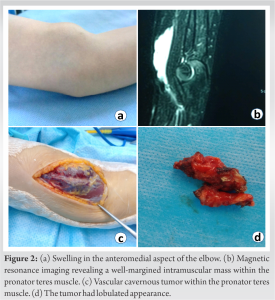
Timeline
Symptoms started 12 months before the first medical visit. X-ray was performed first, followed by ultrasonography and MRI. Once diagnosis was defined immediately surgery was performed within the following week. Histopathology results were released a few days later. The patient had regular follow-up visits. The latest follow-up was at 12-month postoperatively.
<H3>Diagnostic assessment
Plain radiograph of the left elbow revealed a small erosion of the medial cortex of the distal humerus. No calcification was found. Ultrasonography showed an ovalary well-margined hypoechoic intramuscular mass sized 26 × 21 × 10 mm. It was a heterogeneous low-flow vascular lesion including phlebolith calcification. MRI showed a fusiform well-margined intramuscular mass of 17 × 8 × 35 mm within the pronator teres muscle (Fig. 1b). The mass had an intermediated signal intensity with fat overgrowth on the T1-weighted and recovery images and high signal intensity on the T2-weighted images. T1-weighted gadolinium-enhanced axial and coronal MRI revealed heterogeneous signal intensity. MRI did not reveal any bone lesions. The bone erosion observed on the radiograph did not have any affiliation to the mass on MRI.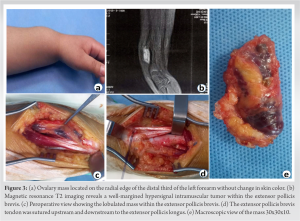
Therapeutic intervention
Benign vascular tumor was suspected and surgery was performed under general anesthesia. A pneumatic tourniquet was applied to the upper left arm. We used a 6 cm vertical incision centered on the pronator teres. The mass had a lobulated appearance surrounded by fat located within the humeral head of the pronator teres muscle (Fig. 1c). Tumor limits were clear. It was dissected carefully and excised totally. An afferent vessel was found and ligated. No adherence to adjacent structures and the profound fascia was found. No contact with the ulnar nerve was observed. The mass size was approximately 30x20x10mm with firm consistency (Fig. 1d). Histopathological examination of the excised mass revealed a proliferation of benign vascular channels within skeletal muscle, associated with a mature adipocytic component. The tumor is composed of mixed vessel types, including lymphatics, large thick-walled veins, and dilated vascular channels. Furthermore, there are cavernous-like spaces, an arteriovenous component, and some thick-walled veins in the tumor. Areas with the cavernous lymphatic component are predominant. These vascular spaces were filled with blood or lymphatic fluid. Some vessels display thrombosis, with occasional formation of phleboliths attested by the presence of calcification. There was no evidence of cytonuclear atypia or mitosis (Fig. 1e).
Follow-up and outcomes: A 3 monthly medical visit was carried out and consisted of a clinical examination. At 1-year follow-up, the patient reported no pain with excellent function of the elbow. Moreover, there was no recurrence.
Case 2
Patient information
A 6-year-old female, without medical history, presented with a mass of the proximal third of the left elbow (Fig. 2a). The mass has slowly grown over a year without pain.
Clinical findings
The mass size was approximately 50 × 20 mm without clear boundaries. No changes in the covering skin or pulsion were observed. Joint range of motion and neurological examination was normal.
Timeline
Symptoms started 12 months before the first medical visit. X-ray was performed first, followed by ultrasonography and MRI. Once diagnosis was defined immediately surgery was performed within the following week. Histopathology results were released a few days later. The patient had regular follow-up visits. The latest follow-up was at 12-month postoperatively.
Diagnostic assessment
Plain radiographs of the left elbow were normal. MRI showed a well-margined intramuscular mass of 30 mm within the pronator teres muscle (Fig. 2b).
Therapeutic intervention
The tumor was dissected carefully and excised using an 8 cm incision (Fig. 2c). Tumor limits were clear. No adherence to adjacent structures and the profound fascia was found. No contact with the ulnar nerve was observed. The mass size was approximately 30 × 30 × 10 mm with firm consistency (Fig. 2d). Histopathological examination found a cavernous hemangioma.
Follow-up and outcomes
A 3 monthly medical visit was carried out and consisted only of a clinical examination. At 1-year follow-up, the patient reported no pain with excellent function of the elbow. Moreover, there was no recurrence.
Case 3
Patient information
A 6-year-old girl, without medical history, presented with a mass of the distal third of the left forearm. The mass has slowly grown over a year without pain (Fig. 3a).
Clinical findings
Physical examination found a soft swelling ovalary sub-cutaneous mass. The mass was 5cmx3cm approximately with clear boundaries. The mass was located on the radial edge of the distal third of the left forearm, without pain or change in skin color. Joint mobility of the fingers, especially of the thumb, was normal.
Timeline
Symptoms started 12 months before the first medical visit. X-ray was performed first, followed by ultrasonography and MRI. Once diagnosis was defined immediately, surgery was performed within the following week. Histopathology results were released a few days later. The patient had regular follow-up visits. The latest follow-up was at 12-month postoperatively.
Diagnostic assessment
Plain radiograph of the left forearm did not show any abnormalities. Ultrasonography showed an ovalary hypoechoic mass of 50 × 30 mm. MRI T2 imaging revealed a hypersignal mass within the pollicis brevis muscle.
Therapeutic intervention
We used an 8 cm vertical incision on the posterior aspect of the distal forearm (Fig. 3b). The mass had a lobulated appearance surrounded by fat located within the extensor pollicis brevis muscle in its musculotendinous junction. Tumor limits were clear (Fig. 3c). The extensor pollicis brevis muscle was excised partially with its tendon. The remaining tendon was sutured upstream and downstream to the extensor pollicis longus (Fig. 3d). The thumb was immobilized using a thumb spica splint. Histopathological examination of the excised mass revealed a cavernous hemangioma.
Follow-up and outcomes
A 3 monthly medical visit was carried out and consisted of only a clinical examination. At 1-year follow-up, the patient reported no pain with excellent function of the thumb. Moreover, there was no recurrence.
Hemangiomas are common benign proliferations of blood vessels accounting for 7% of all soft-tissue tumors [2]. Hemangiomas are distinguished from vascular malformations clinically by the rapid growth of the tumor volume during childhood and histologically by endothelial hyperplasia with the formation of a basement membrane laminated under the endothelium [3]. The majority of hemangiomas are cutaneous, subcutaneous, and mucosal. They are intramuscular, arising in skeletal muscle, only in 0.8% of diagnosed cases [2,4]. In 1843, Liston reported the first case by describing a hemangioma that had developed in the semimembranosus muscle [5]. Since then, intramuscular hemangiomas have been reported regularly in literature often by case reports in different muscles. Up to 1983, only 527 cases of hemangioma originating in the skeletal musculature have been recorded in the literature [6]. The lower limbs are the most frequent localization (45%), followed by the upper limbs (27%). Only 14% are located in the head-and-neck region and 14% in the trunk [6]. The most commonly affected muscle is the quadriceps. Localization in muscles of the upper limb, particularly in the elbow, is very rare [7]. These tumors are usually diagnosed at young adulthood, under 30 in 80 to 90 % of cases with no sex preference [8]. In our case, it showed up at the age of 6 and 18. Their etiology is unclear and they are considered congenital in origin. Histologically, they are thought to be hamartoma or neoplasm [2]. According to Scott [9], hemangiomas are arising in abnormal embryonic sequestrations and evolve slowly over the years until causing clinical symptoms. Minor trauma or excessive muscle contraction is believed to play a role in the growth of the mass by stimulating blood flow in the preexisting tumor. In 1972, Allen and Enzinger [2] classified hemangiomas of skeletal muscles in three types based on the tumor vessels size: Small-vessel type, large-vessel type, and mixed type. Cavernous hemangiomas are part of the large-vessel type. They represent the most common type of intramuscular hemangiomas. Hemangiomas are also classified based on the predominant type of vascular channel in four types [10]: Capillary hemangiomas are composed of numerous capillaries with small lumens with no connective tissue separating the capillaries; they are the most common hemangiomas. Cavernous hemangiomas are composed of caverns that are lined by a single layer of endothelial cells filled with large blood spaces and separated by fibrous tissue. Arteriovenous hemangiomas are composed of fetal capillaries with abnormal communication between arteries and veins. Venous hemangiomas are composed of dilated veins with walls of varying thickness within a loose fatty-fibrous stroma. In the first case, cavernous hemangioma was identified through histological findings of mixed cavernous vascular structures including lymphatics, large thick-walled veins, and dilated vascular channels filled with blood or lymphatic fluid. Moreover, occasional phleboliths were revealed in some vascular spaces. Phleboliths are commonly seen in cavernous hemangiomas as a result of dystrophic calcification within organizing thrombi [11]. Approximately 50% of these tumors remain undetected until the clinical symptoms are revealed [2]. As in many other soft-tissue tumors, pain and palpable mass represent the most common initial symptoms. In particular locations, these tumors can be the cause of specific clinical signs. The location in the medial region of the elbow is described to cause neurological symptoms by encapsulating or invading the ulnar nerve [12]. The ulnar nerve was not having contact with the tumor and caused no symptoms in the two cases. Due to their low prevalence, non-specific clinical presentation, deep location, and lack of objective clinical findings (e.g., skin discoloration, compressibility, thrills, or pulsation), the pre-operative diagnosis of intramuscular hemangioma is difficult and only 8% of all cases of intramuscular hemangiomas are diagnosed preoperatively. Therefore, imaging methods are essential for the proper diagnosis and distinction from other soft-tissue tumors [13]. However, pathologic confirmation is mandatory for final diagnosis. The plain radiograph showed phleboliths which are pathognomonic of cavernous angiomas and present in 25–30% of cases [12]. CT scan and ultrasound examination were used as imaging pre-operative studies but MRI remains the method of choice in defining the vascular nature of the tumor and delineating its anatomic extent. On T1-weighted imaging, hemangiomas are isointense or hypointense to muscle. On T2 imaging, the lesions are hyperintense on account of the volume of stagnant blood, clearly differentiated from the normal muscle and fibro-fatty septa. MRI may also help to differentiate between types of hemangiomas. Lesions with large cystic spaces are cavernous, whereas arteriovenous hemangiomas show more prominent fast-flow serpentine vessels. Venous hemangiomas show slow-flow serpentine vessels. This particular type of hemangioma does not undergo spontaneous regression and may be locally destructive with time due to pressure exerted on neighboring structures [14]. Complete surgical resection is the most efficient technique and complete local excision is therefore advised whenever feasible. Otherwise, the rate of recurrence is important [15]. Allen and Enzinger [2] reviewed 89 cases and found 18% of recurrences, 7% more than once. In some recurrent or invasive hemangiomas, embolization or radiation therapy can be considered as secondary therapeutic options [13].
Even though they are rare, intramuscular hemangiomas of the forearm are a condition that should be evoked by orthopedic surgeons in front of pain and swelling of this region. MRI is the most effective imaging method to suspect the diagnosis. Reference treatment is complete surgical resection. Otherwise, the rate of recurrences rises. We present three cases of intramuscular hemangioma of the upper limb. All cases contained a detailed description and illustration of the clinical, diagnostic testing, and outcomes of the surgical treatment.
Intramuscular hemangiomas of the forearm are a condition that should be evoked by clinicians. The surgical treatment consisting in tumor resection followed by histopathology confirms the diagnosis.
References
- 1.Canavese F, Soo BC, Chia SK, Krajbich JI. Surgical outcome in patients treated for hemangioma during infancy, childhood, and adolescence: A retrospective review of 44 consecutive patients. J Pediatr Orthop 2008;28:381-6. [Google Scholar | PubMed]
- 2.Allen PW, Enzinger FM. Hemangioma of skeletal muscle. An analysis of 89 cases. Cancer 1972;29:8-22. [Google Scholar | PubMed]
- 3.Fernández-Pineda I. Intramuscular cavernous hemangioma. Am J Surg 2009;198:300-1. [Google Scholar | PubMed]
- 4.Watson WL, McCarthy WD. Blood and lymph vessel tumors. A report of 1056 cases. Surg Gynecol Obstet 1940;71:569-88. [Google Scholar | PubMed]
- 5.Ferri E, Pavon I, Armato E. Intramuscular cavernous hemangioma of the sternocleidomastoid muscle: An unusual neck mass. Otolaryngol Head Neck Surg 2007;137:682-3. [Google Scholar | PubMed]
- 6.Cohen AJ, Youkey JR, Clagett GP, Huggins M, Nadalo L, d’Avis JC. Intramuscular hemangioma. JAMA 1983;249:2680-2. [Google Scholar | PubMed]
- 7.Dammak N, Rouhou HC, Khalifa I, Haddad I, Zitoun Y, Abid F. Intramuscular cavernous haemangioma of the triceps. Pan Afr Med J 2020;36:139. [Google Scholar | PubMed]
- 8.Enzinger FM, Weiss SW. Soft Tissue Tumors. St Louis: CV Mosby; 1988. p. 512-4. [Google Scholar | PubMed]
- 9.Scott JE. Haemangiomata in skeletal muscle. Br J Surg 1957;44:496-501. [Google Scholar | PubMed]
- 10.Fletcher CD, Bridge JA, Hogendoorn PC, Mertens F, editors. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon: IARC Press; 2013. [Google Scholar | PubMed]
- 11.Pattamapaspong N, Peh WC, Shek TW. Imaging of intramuscular haemangiomas of the extremities. Singapore Med J 2020;61:122-8. [Google Scholar | PubMed]
- 12.Fnini S, Messoudi A, Benjeddi Y, Elandaloussi Y, Hassoun J, Garche A, et al. Intramuscular hemangioma of the forearm: Seven cases. Ann Chir Plast Esthet 2013;58:243-7. [Google Scholar | PubMed]
- 13.Eryilmaz MA, Varsak YK, Gül Z, Uğur A. Intramuscular cavernous hemangioma of the temporalis muscle. J Craniofac Surg 2014;25:1400-1. [Google Scholar | PubMed]
- 14.Melman L, Johnson FE. Intramuscular cavernous hemangioma. Am J Surg 2008;195:816-7. [Google Scholar | PubMed]
- 15.Bella GP, Manivel JC, Thompson RC Jr., Clohisy DR, Cheng EY. Intramuscular hemangioma: Recurrence risk related to surgical margins. Clin Orthop Relat Res 2007;459:186-91. [Google Scholar | PubMed]