High level of suspicion is needed in cases of chronic foot and ankle swelling to diagnose and treat fungal arthritis in the early stages for better functional outcome.
Dr. Shrihari L Kulkarni, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad, Karnataka, India. E-mail: shrihari1711@gmail.com
Introduction: Fungal infection of the musculoskeletal system is very rare. We present a rare case of fungal infection in the ankle joint. Skeletal phaeohyphomycosis (PHM) has been reported only once before in the literature.
Case Report: A 56-year-old man presented with pain and swelling in his right ankle for 2 years. There was a diffuse swelling over the medial and lateral aspect of the ankle with restricted movements. Arthroscopic biopsy was done from the ankle and histopathological examination showed pigmented fungi with few phagocytosed fungal hyphae within multinucleated giant cells indicating PHM. The patient was treated with itraconazole. At 1-year follow-up, the patient is pain free and can do his routine activities comfortably.
Conclusion: Fungal infection is a rare condition and must be kept in mind while dealing with chronic foot and ankle swelling. Early diagnosis and treatment will give good functional results.
Keywords: Ankle joint, fungal infection, phaeohyphomycotic, ankle arthroscopy.
Fungal arthritis also known as mycotic arthritis is the inflammation of the joint caused by fungus. The most common fungal infection of joints is caused by the Candida species, mainly, Candida albicans. Phaeohyphomycosis (PHM) is the group of mycoses caused by pigmented fungi. They are rare in occurrence and are mostly encountered in immunocompromised patients [1]. We present a case of fungal infection of the right ankle joint caused by PHM in a 56-year-old man.
A 56-years-old man presented to our outpatient department with pain and swelling over his right ankle joint for 2 years. There was no history of trauma. The local examination revealed diffuse swelling around the ankle with tenderness over the lateral and medial aspects. The range of movements was painful and restricted.  Radiographs revealed diffuse soft-tissue shadow around the ankle with posterior osteophytes in the ankle joint (Fig. 1 and 2).
Radiographs revealed diffuse soft-tissue shadow around the ankle with posterior osteophytes in the ankle joint (Fig. 1 and 2).  MRI showed marrow edema with enhancement in the distal tibia and talus and calcaneum with multiple subchondral cysts with diffuse cortical erosions adjacent to the articular surfaces (Fig. 3).
MRI showed marrow edema with enhancement in the distal tibia and talus and calcaneum with multiple subchondral cysts with diffuse cortical erosions adjacent to the articular surfaces (Fig. 3).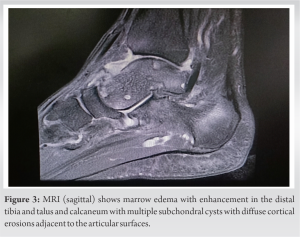 Ankle arthroscopy was performed and the synovial biopsy was done. Histopathological examination of the synovium showed hyperplastic synovium with well-formed granuloma comprising of epithelioid histocytes, Langhan`s type giant cells, and fibroblasts. Pigmented fungi were noted with phagocytosed fungal hyphae within multinucleated giant cells. All features were indicative of PHM (Fig. 4). The patient was immediately started with itraconazole 200 mg twice a day and physiotherapy. Anti-fungal therapy was given for 2 months, and the patient was relieved of pain and swelling by then. At 1-year follow-up, the patient is comfortable and carrying out his routine activities without any signs of any recurrences.
Ankle arthroscopy was performed and the synovial biopsy was done. Histopathological examination of the synovium showed hyperplastic synovium with well-formed granuloma comprising of epithelioid histocytes, Langhan`s type giant cells, and fibroblasts. Pigmented fungi were noted with phagocytosed fungal hyphae within multinucleated giant cells. All features were indicative of PHM (Fig. 4). The patient was immediately started with itraconazole 200 mg twice a day and physiotherapy. Anti-fungal therapy was given for 2 months, and the patient was relieved of pain and swelling by then. At 1-year follow-up, the patient is comfortable and carrying out his routine activities without any signs of any recurrences.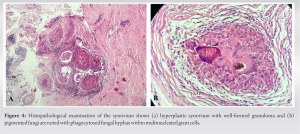
Fungal infection of the musculoskeletal system is rare but notorious for causing persistent, chronic, low-grade infection [2]. PHM is tissue infection caused by dematiaceous (pigmented) hyphae or yeasts. There are more than 150 species classified which are primarily soil and wood saprophytes causing opportunistic infections in humans. Skin and central nervous system are the most involved systems [3]. The following are the important risk factors for the fungal infection: immunosuppression by disease of medication (e.g., anti-tumor necrosis factor drugs), substance abuse, long-term presence of indwelling catheter, parenteral nutrition, diabetes mellitus, use of broad-spectrum antibiotics, HIV infection, organ transplantation [4]. Skin lesions following trauma mainly involve hands and feet. Subcutaneous granulomas are common in European countries. Lung and eye involvement is also common. Cerebral infections have maximum mortality rates. Skeletal system is rarely involved, and joint infections are either secondary to the direct spread following trauma or systemic spread through inhalation. The most important risk factors for PHM are history of trauma, diabetes mellitus, corticosteroid use, malnutrition, tumors, kidney transplantation, and chemotherapy. Systemic PHM is restricted to immunocompromised patients and is usually fatal [5,6]. Histopathology is diagnostic, due to large number of species cultures required to know the specific species of the organism and the antibiotic sensitivity. Histopathological features include granulomatous inflammation with necrosis and purulent debris with or without foreign material. Organisms appear as pigmented yeast in chains to hyphal forms in and around the granulomatous reaction. Molecular identification of fungi by polymerase chain reaction is rapid and specific in diagnosing PHM [7,8]. Itraconazole is drug of choice for the treatment of PHM. Alternatively, posaconazole can also be used. Solitary lesions can be managed with surgical excision and the disseminated lesions require systemic anti-fungal therapy. Only one such case of skeletal PHM has been reported in the literature before our report [9,10]. Our patient had no history of trauma or any wound around the joint, and infection by systemic spread is the most likely mode of infection. The diagnosis was confirmed by histopathological examination of the synovial tissue sent by arthroscopic biopsy and the patient was managed with oral itraconazole leading to full recovery.
Fungal arthritis is a rare condition and PHM is rarer. Diagnosis must be kept in mind while dealing with chronic foot and ankle swellings. Tissue biopsy and histopathological examination are gold standard for diagnosis. Early treatment with appropriate anti-fungal agent will give good functional results.
Histopathological examination after synovial biopsy is gold standard for the diagnosis of the fungal arthritis and early treatment with appropriate anti-fungal agents is pivotal for the good functional recovery of the patients.
References
- 1.Tucker A, Matthews S, Wilson A. Mycotic septic arthritis of the ankle joint. Am J Orthop (Belle Mead NJ) 2016;45:E478-80. [Google Scholar | PubMed]
- 2.Sealy PI. Fungal osteomyelitis. Eur Int J Sci Technol 2015;4:17-22. [Google Scholar | PubMed]
- 3.He Y, Zheng HL, Mei H, Lv GX, Liu WD, Li XF. Phaeohyphomycosis in China. Front Cell Infect Microbiol 2022;12:895329. [Google Scholar | PubMed]
- 4.Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda RA, Born CT. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg 2014;22:390-401. [Google Scholar | PubMed]
- 5.Gené J, Azón-Masoliver A, Guarro J, Ballester F, Pujol I, Llovera M. Cutaneous phaeohyphomycosis which was caused by Alternaria longipes in an immunosuppressed patient. J Clin Microbiol 1995;33:2774-6. [Google Scholar | PubMed]
- 6.Cardoso SV, Campolina SS, Guimarães AL, Faria PR, da C Costa EM, Gomez RS. Oral phaeohyphomycosis. J Clin Pathol 2007;60:204-5.n. [Google Scholar | PubMed]
- 7.Kumar YS, Kurian N, Lawrence M, Vimal K, Teerthanath S. A rare case of fungal osteoarthritis which was caused by phaeohyphomycosis. J Clin Diagn Res 2012;6:888-9. [Google Scholar | PubMed]
- 8.Halaby T, Boots H, Vermeulen A, van der Ven A, Beguin H, van Hooff H. Phaeohyphomycosis which was caused by Alternaria infectoria in a renal transplant recipient. J Clin Microbiol 2001;39:1952-5. [Google Scholar | PubMed]
- 9.Ben-Ami R, Lewis RE, Raad II, Kontoyiannis DP. Phaeohyphomycosis in a tertiary care cancer center. Clin Infect Dis 2009;48:1033-41. [Google Scholar | PubMed]
- 10.Shivaswamy KN, Pradhan P, Laxmisha C, Thappa DM, Jayanthi S. Disseminated phaeohyphomycosis. Int J Dermatol 2007;46:278-81. [Google Scholar | PubMed]