Giant iliac osteochondroma is a rare but cosmetically disabling tumor and its timely diagnosis followed by en bloc excision warrants an immediate improvement in the quality of life.
Dr. Mohit J Jain, Department of Orthopedics, SBKS Medical Institute and Research Center at Sumandeep Vidyapeeth and Dhiraj Hospital, Waghodia, Vadodara, India. E-mail: dr.mits4u@gmail.com
Introduction: Osteochondroma is the most common benign bone tumor where a chondrogenic lesion is derived from aberrant cartilage from the perichondral ring. Although it commonly arises from the growing ends of long bones, less commonly, it may arise from the scapula, pelvis, or vertebra.
Case Report: We encountered a 16-year-old male patient with a painless left pelvic solid mass for 3 years, which was suggestive of osteochondroma on X-ray and magnetic resonance imaging findings. Besides cosmetic issues, the main indication for surgery was the constant discomfort in wearing pants/shorts/belts. He underwent en bloc excision followed by a biopsy of the surgical specimen by two independent histopathologists confirming the tumor to be osteochondroma. He was followed up for 2 years with no signs of post-operative complications or recurrence. This case represents one of the very few reported so affecting the iliac wing, where the excision was performed before skeletal maturation. We also performed a review of the current literature on iliac wing osteochondroma to understand the tumor better, identify gaps in current knowledge, and suggest areas for future research.
Conclusion: Since one of the differential diagnoses includes secondary chondrosarcoma, which could be a rare progression of osteochondroma, early recognition and comprehensive evaluation of such unusual cases needs to be dealt with a high index of suspicion to avoid misdiagnosis and to provide effective treatment.
Keywords: En bloc excision, ilium, osteochondroma.
Osteochondroma is the most common benign bone tumor accounting for 20 to 50% of all benign osseous tumors [1, 2]. However, the true incidence is difficult to predict as most cases are asymptomatic and do not seek medical attention due to painless mass. Osteochondromas may be solitary (85%) or multiple (15%). The multiple forms are an autosomal dominant syndrome referred to as hereditary multiple exostosis or familial osteochondromatosis. It usually grows on the metaphysis toward the rising end of the long bones (femur, tibia, humerus, etc.) but may develop in flat bones (scapula, feet, and pelvis) [3]. Patients typically present between the ages of 10 and 30 with a slight predilection for the male gender. Continuity of the cortex and medulla of the tumor, along with the underlying bone, is a pathognomonic feature in establishing the diagnosis [4]. Pelvic osteochondroma has been reported with an incidence of 5% of all osteochondromas [1]. The treatment of this tumor is en bloc excision for cosmetic deformity or pressure symptoms [5].
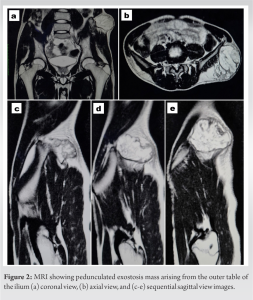
We encountered a 16-year-old male patient with a painless left pelvic solid mass for 3 years with a gradual increase in size during the subsequent period. It was suggestive of osteochondroma in radiology. We used magnetic resonance imaging (MRI) to characterize the lesion definitively. There were no associated medical comorbidities or positive family history for a similar problem. On physical examination, bony-hard, non-tender, and fixed but non-adherent mass from overlying skin measuring approximately 10 cm × 7 cm × 6 cm was noted over the anterolateral left iliac wing. Local examinations were negative for lymphadenopathy, dilated veins, or skin changes on or around the mass. Spine and left hip range of motions was full and free with normal distal neurovascularity of the lower extremity and normal gait. Pelvis with both hips (PBH) anteroposterior (A-P) view radiogram demonstrated a popcorn-like high-density mass with well-defined, clear boundaries on the left side of the outer cortex of the iliac wing (Fig. 1). 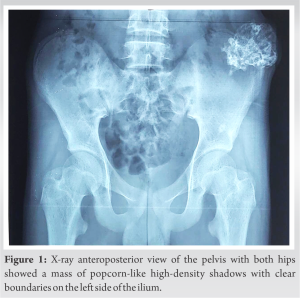
Surgical technique
The patient was planned for an en bloc excision biopsy of the tumor after all the necessary basic investigation, pre-anesthetic fitness, and consent. Spinal anesthesia was given and the patient was lying down in the right lateral position. Painting and drapping were done under aseptic precautions. The operating surgeon and assistant were both standing at the patient’s back/posterior side. Tumor boundaries were marked in circular manner by a sterile surface marker to determine the extent and direction of the incision (Fig. 3). A central curvilinear skin incision (11 cm) was made parallel to the long axis over the mass. Fascia-like covering of the tumor was removed until the solid cartilaginous part was exposed. Then, the muscles were separated by a periosteum elevator from the basal surface of the mass and the outer cortex of the iliac wing until the tumor pedicle was exposed (Fig. 4a).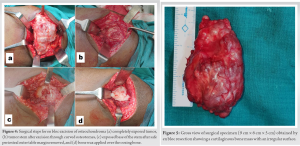

Post-operative protocol
The excision biopsy specimens were sent to laboratories in diluted formalin. Histopathologic examination was performed by two experienced independent oncohistopathologists (one was blinded about clinical and radiological findings, and the other was non-blinded) to confirm the osteochondroma. Mature hyaline cartilage with fibrous perichondrial covering over the mature bone without any malignancy confirmed a pedunculated osteochondroma (Fig. 8). 
Literature review
As far as our knowledge is concerned, our’s is the first study that performed a review solely on osteochondroma arising from the ilium. We performed literature search using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. We conducted the literature search through PubMed, EMBASE, Scopus, and Web of Science using the terms “osteochondroma,” “exostosis,” “pelvis,” “ilium,” and “solitary” with various spellings and Boolean logical operator. We reviewed 95 abstracts and included cases after reading the full text with a comprehensive description of the occurrence, symptoms, physical examination, radiologic characteristics, treatment, and follow-up results. We excluded duplicate articles, other language articles (where the English translation is unavailable), those discussing pelvic osteochondroma other than iliac wing (i.e., pubic and ischial region), cases of multiple exostosis, and osteosarcoma cases.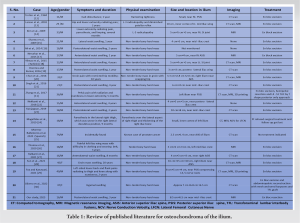
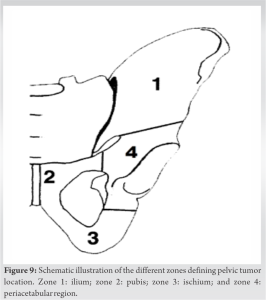
Osteochondroma is considered as an osteocartilaginous aberrant growth of normal physeal growth plates and, hence, believed to be a developmental lesion [6]. This theory is supported by the cases of osteochondroma reported following trauma or irradiation. However, recent research suggests that osteochondromas may truly be neoplasms as genetic mutations have been found in both MHE and solitary forms [7]. Despite the oldest article, we found about pelvic osteochondroma was by Ghormley et al., in 1946, there have been very few cases reported so far which suggest how rare is the pelvis for such a common tumor [8]. With their initial experience with 37 patients at the Mayo clinic between 1910 and 1943, they concluded that “chondromatosis of the pelvis must always be considered as serious surgical lesions.” The majority of osteochondroma arises from the ilium of the pelvis. However, ischium, pubis, and periacetabular region may rarely give rise to osteochondroma (Fig. 9). Our case was unusual in a number of ways. The patient’s age at presentation was younger than the typical age group. Besides, it is again very rare for it to let alone develop into such a huge tumor within few years of course as in our case. In our case, the tumor size was increasing, which began causing significant impairment with daily living. Pedunculated morphology as in our osteochondroma case is less likely to undergo shrinkage as compared to sessile ones [9]. Osteochondroma with continuous growth after skeletal maturity should raise the possibility of malignant chondrosarcoma. However, we decided not to wait due to constant discomfort in wearing pants or the lower extremity outfits and near total skeletal maturity. Besides, despite the rare location, pelvic osteochondroma has more chance of malignant transformation into secondary osteosarcoma than any other site and it also is associated with worse outcome [10]. Other serious complication in these regions can lead to fractures, hip joint mobility restriction, vascular impairment, neurological sequelae, hematuria, and sexual dysfunction. X-ray itself can be diagnostic in most cases. However, we recommend that CT scan or MRI as it allows anatomic delineation necessary for the surgical planning. Moreover, 3D printing is of immense value in case or osteochondroma causing nerve root compression [11]. Surgical en bloc excision is the treatment of choice for symptomatic osteochondroma. Our patient showed complete resolution of problems postoperatively with no post-operative recurrence. Similarly, all the cases we reviewed recovered fully after en bloc resection of tumor, and hence, it should be offered whenever indicated. Finally, there is no substitution for microscopic examination to prove that the chondrocytes grew actively and did not deteriorate. We do recommend two independent reporting to avoid any sampling or human error in definitive diagnosis.
Even though the majority of osteochondromas arise from the metaphysis of long bones, case reports have shown that osteochondromas presenting in atypical locations such as the pelvis do occur. Iliac osteochondroma can greatly impair the quality of life of the patients even after being asymptomatic clinically. Better recognition and more comprehensive evaluation of these rare cases should be highlighted to avoid misdiagnosis during clinical practice. All providers, particularly those in primary care, should be aware of these conditions as patients with asymptomatic iliac mass lesions will most likely initially present to them.
We suggest a high index of suspicion for pelvic osteochondroma in skeletally immature patients and its en bloc excision is indicated whenever the atypical location of the tumor compromises the quality of life.
References
- 1.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: Variants and complications with radiologic-pathologic correlation. Radiographics 2000;20:1407-34. [Google Scholar]
- 2.Garcia RA, Inwards CY, Unni KK. Benign bone tumors--recent developments. Semin Diagn Pathol 2011;28:73-85. [Google Scholar]
- 3.Motamedi K, Seeger LL. Benign bone tumors. Radiol Clin North Am 2011;49:1115-34, v. [Google Scholar]
- 4.Baig MN, O’Malley S, Fenelon C, Kaar K. Osteochondroma of acromioclavicular joint. BMJ Case Rep 2019;12:e230246. [Google Scholar]
- 5.Herode P, Shroff A, Patel P, Aggarwal P, Mandlewala V. A rare case of pubic ramus osteochondroma. J Orthop Case Rep 2015;5:51-3. [Google Scholar]
- 6.Clarke DO, Crichlow A, Christmas M, Vaughan K, Mullings S, Neil I, et al. The unusual osteochondroma: A case of snapping scapula syndrome and review of the literature. Orthop Traumatol Surg Res 2017;103:1295-8. [Google Scholar]
- 7.Pacifici M. The pathogenic roles of heparan sulfate deficiency in hereditary multiple exostoses. Matrix Biol 2018;71-72:28-39. [Google Scholar]
- 8.Ghormley RK, Meyerding HW. Osteochondromata of the pelvic bones. J Bone Joint Surg Am 1946;28:40-8. [Google Scholar]
- 9.Aiba H, Yamada S, Yamamoto N, Hayashi K, Miwa S, Tsuchiya H, et al. Spontaneous shrinkage of solitary osteochondromas. Skeletal Radiol 2018;47:61-8. [Google Scholar]
- 10.Tsuda Y, Gregory JJ, Fujiwara T, Abudu S. Secondary chondrosarcoma arising from osteochondroma: Outcomes and prognostic factors. Bone Joint J 2019;101-B:1313-20. [Google Scholar]
- 11.Zhang Y, Wen L, Zhang J, Yan G, Zhou Y, Huang B. Three-dimensional printing and computer navigation assisted hemipelvectomy for en bloc resection of osteochondroma: A case report. Medicine (Baltimore) 2017;96:e6414. [Google Scholar]
- 12.Trotter D, Zindrick M, Ibrahim K. An unusual presentation of an osteochondroma. Report of a case. J Bone Joint Surg Am 1984;66:299-301. [Google Scholar]
- 13.Larson J, O’Malley JE, Cohen TI. Case report: Solitary pelvic osteochondroma presenting with L3 nerve root compression. Alaska Med 2002;44:35-7. [Google Scholar]
- 14.Kim WJ, Kim KJ, Lee SK, Choy WS. Solitary pelvic osteochondroma causing L5 nerve root compression. Orthopedics 2009;32:922. [Google Scholar]
- 15.Sharma S, Kalsotra N, Gupta P, Wani I, Singh M, Singh D. Solitary osteochondroma of the ilium: A case report. Internet J Orthop Surg 2009;16(2);20-23. [Google Scholar]
- 16.Ali N, Bhat A, Bangroo FA, Dhanda MS, Maqsood M, Sharma SC. Isolated osteochondroma of the ilium: Case report with review of the literature. Scholars J Appl Med Sci 2014;2:1573-6. [Google Scholar]
- 17.Nerurkar AA, Parikh MS, Chavan V, Gujarathi GA. A rare case of a solitary osteochondroma of the anterior superior iliac spine: A case report. Int J Orthop Sci 2015;1:31-3. [Google Scholar]
- 18.Yilmaz S, Demirtaş Y, Gülçek M, Deveci A, Yildirim AO, Öken OF, et al. Solitary osteochondroma of the Ilium: A case report. J Kartal TR 2015;26:89-93. [Google Scholar]
- 19.Doomra T, Kumar A. A rare case of a solitary osteochondroma of the iliac wing: Case report. J Evol Med Dent Sci 2016;5:732-5. [Google Scholar]
- 20.Chun YS, Rhyu KH, Cho KY, Cho YJ, Lee CS, Han CS. Osteochondroma arising from anterior inferior iliac spine as a cause of snapping hip. Clin Orthop Surg 2016;8:123-6. [Google Scholar]
- 21.Singh A, Sharma, A, Kumar M, Mathur AK. Solitary osteochondroma of the ilium: A rare case report. Int J Sci Res 2016;5:622-624. [Google Scholar]
- 22.Nekkanti S, Savsani S, Reddy YC, Meka A, Mahtani A. A rare sessile variant of osteochondroma presenting at an unusual site of the iliac wing in a 15-year-old boy. J Orthop Allied Sci 2018;6:93-5. [Google Scholar]
- 23.Kunjappan SK. A rare case of osteochondroma in iliac crest-a case report. Univ J Surg Surg Spec 2019;5(4):61-64. [Google Scholar]
- 24.Magalhães LV, Massardi FR, Pereira SA. Pelvic osteochondroma causing meralgia paresthetica. Neurol India 2019;67:928-9. [Google Scholar]
- 25.Moreno-Ballesteros A, Calvo-Morón MC, García-Gómez FJ, Castro-Montaño J. Incidental finding of pelvic osteochondroma. Reumatol Clin (Engl Ed) 2020;16:183-4. [Google Scholar]
- 26.Thomas C, Sanderson B, Horvath DG, Mouselli M, Hobbs J. An unusual case of solitary osteochondroma of the iliac wing. Case Rep Orthop 2020;2020:8831806. [Google Scholar]
- 27.Kulkarni SL, Mannual S, Daragad MS, Girirajaiah SH. Iliac wing osteochondroma in a 16-year-old boy: A case report. Int J Res Orthop 2021;7:171-4. [Google Scholar]
- 28.Sun J, Wang ZP, Zhang Q, Zhou ZY, Liu F, Yao C, et al. Giant osteochondroma of ilium: A case report and literature review. Int J Clin Exp Pathol 2021;14:538-44. [Google Scholar]
- 29.Fox O, Kanawati A. 3D printed composite model of pelvic osteochondroma and nerve roots. 3D Print Med 2021;7:31. [Google Scholar]
- 30.Olivero AA, Laxague F, Jorge FD, Sadava EE. Reconstruction of the abdominal wall after radical resection of pelvic osteochondroma. Cir Esp (Engl Ed) 2022;100:30 [Google Scholar]