Aseptic-looking non-union in long bones can be misdiagnosed and turn out to be septic non-union due to a chronic subclinical infection, making it essential to have multiple surgical options on table for such cases.
Dr. Aniket Wagh, Department of Orthopaedics, Employees’ State Insurance Hospital, Kandivali, Mumbai, Maharashtra, India. E-mail: ani4u8725@gmail.com
Introduction: The usual cause of a distal tibial fracture is a high-energy trauma. Although multiple options are available for their treatment such as intramedullary nailing, open plating, and external fixator, each of these options might result in a non-union. Knowing the type of non-union not only allows us to guess the cause but also directs us toward the best possible treatment. Despite this, we might still get surprises on the operating table due to pre-operative misdiagnosis.
Case Report: Reporting a case of a 42-year-old male with a 15-month-old left distal tibia non-union. The index injury was a grade 1 distal third tibia fibula fracture which was fixed with a plate and screws 15 months back. All the clinical and biochemical signs hinted toward the diagnosis of an aseptic non-union and the treatment was planned accordingly. However, intraoperative findings were much different due to which the surgeons had to improvise and change the intervention to an antibiotic-coated nail.
Conclusion: Although each variety of non-union has its set of signs and symptoms, they can be misleading. Different etiologies can coexist making it difficult to give a perfect pre-operative diagnosis and management. Non-unions, especially in the tibia, thus need meticulous understanding of the underlying disease process and extensive treatment strategies.
Keywords: Aseptic, non-union, septic, distal tibia, antibiotic-coated nail, subclinical infection.
According to the Food and Drug Administration, non-union is said to have occurred when the fracture is at least 9 months old and has shown no clinical and radiological signs of healing for three consecutive months [1]. Fracture union requires good interplay between reduction technique, surgical stabilization as well as host biology. Calori and Giannoudis described the diamond concept which tells the importance of the biological environment, factoring in osteogenic cells, osteoconductive scaffolds, and growth factors; as well as mechanical stability [1, 2]. Fracture healing would be endangered if any one of these factors is inadequate [3]. Tibia is the most commonly injured long bone [4]. The rate of tibia non-union is around 1.1% if treated nonoperatively and nearly 5% if treated operatively [1, 2, 5]. These numbers increase significantly in cases of open fractures [1]. Non-unions are especially more common in the distal third tibia due to its subcutaneous location, inadequate soft-tissue cover, and paucity of blood supply. Apart from having an inimical effect on the patient’s quality of life, non-unions also have an impact on the health care cost, probably double the cost of fractures that heal normally [6, 7]. In fact, Kreder, in 2013 had commented that tibial non-union is worse than having a myocardial infarction [8]. Non-unions are broadly classified as septic (infected) and aseptic non-unions with aseptic subclassified as hypertrophic, oligotrophic, atrophic, and finally pseudoarthrosis. Diagnosing the type of non-union is vital as it gives us a clue as to what might be the possible cause of its occurrence, and guides us toward the best possible treatment. However, non-unions with low-grade or subclinical infections are difficult to identify as they might not show any clinical or laboratory signs of infection [9]. Due to the low grade of infection, these cases may be misdiagnosed leading to a completely mismatched treatment strategy.
A 42-year-old male came to us with a history of a grade 1 distal third tibia fracture sustained 15 months back which was fixed with plate and screws the next day of injury. At presentation, he complained of persistent pain at the fracture site and antalgic gait. X-rays showed frank non-union with an interfragmentary screw and a 10-hole medial distal tibia locking plate in situ with 1 locking screw backed out (Fig. 1). There was adequate callus at the fracture site of tibia as well as fibula. There was no clinical, biochemical, or radiological signs of infection. A diagnosis of hypertrophic non-union was made as evidenced by improper reduction, inadequate fixation, and presence of callus. The surgical plan consisted of implant removal, fibulectomy, and replating with good reduction. However, after removing the plate and screws, we encountered pus coming out of one of the screw holes (Fig. 2).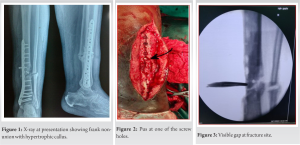

Follow-up
The patient was followed up at monthly intervals. No complications were encountered during the follow-up visits. At 3 months, the patient was walking full weight bearing without support with full knee and ankle range of movements (Fig. 6). No signs of infection. X-rays at 3 months showed complete radiological union (Fig. 7).
Established non-unions are difficult to treat [9-11]. They have a devastating effect on the well-being of the patient in terms of financial and emotional compromise [12, 13]. At the same time, it demands meticulous strategies and prolonged treatment from the treating surgeon [13, 14]. Hypertrophic non-unions are perceived as easier to treat since they are caused due to lack of fracture stability producing excess mobility at the fracture site and forming a hypertrophic callus. Thus, it can be typically solved by providing a more stable fixation [3, 15]. This was thought to be the case in our situation. However, in clinical practice, we often encounter non-unions with several concomitant causal factors. This poses a challenge to clinically diagnose septic versus aseptic non-unions, especially if it is associated with low-grade or chronic infection [9, 16]. Although an open fracture is a known cause of septic non-union, this cannot be an absolute dictum. In fact, a study by Kohlprath et al. in 2011 showed a 23% rate of aseptic non-unions in open fractures of the tibia in adults [17]. Septic non-union may be suspected pre-operatively on certain parameters namely, radiographs showing lysis, sequestering, etc., raised acute phase reactants such as erythrocyte sedimentation rate C-reactive protein [18], raised white blood count, and clinical/local signs of infection. However, all of these might be normal in subclinical infections as were in our case. Magnetic resonance imaging is sensitive but it has its restrictions in metal implanted bones. Positron emission tomography–computed tomography (PET/CT) and single-photon emission computed tomography scan has a good sensitivity of 79%, and specificity of 97% [19-21]. However, these are expensive and have availability issues. It thus becomes difficult to give a definitive diagnosis of septic non-union preoperatively in cases of subclinical infections. Thus, a malleable surgical plan needs to be devised in such cases with all the appropriate implants and trained staff [22]. Microbiological examination of the intraoperatively sampled tissue is needed to establish a final diagnosis. Local high-dose antibiotic delivery can be definitely considered in doubtful diagnosis [22]. Septic non-unions need two important factors- eradication of infection and stability to promote bony union. Conventionally, these were achieved by 2 separate procedures. However, a single-stage antibiotic nail fixation has been known to be equally effective [23] and it would reduce the complications and morbidities of 2-stage procedure. Antibiotic coated nail is especially useful, where the infection is purely intramedullary and the soft-tissue envelope around the fracture is in good condition. Another advantage of a nail is early mobilization and weight bearing. There have been many documentations of the effective use of antibiotic cement-coated intramedullary nailing for infected non-union of tibia [23, 24]. It is useful more so in refractory subclinical infections as it is known to elute antibiotics locally for as long as 36 weeks [25]. Primary bone grafting in infected non-unions is being undertaken successfully by a lot of surgeons, however, its indications are very precise [26]. Newer artificial grafts that claim to be infection resistant have limited studies and would require radical primary debridement [26].
We conclude from this case that aseptic-looking non-union in long bones can very well turn out to be a septic non-union due to subclinical infection. Pre-operative clinical, radiological, and even biochemical markers can misdiagnose such cases. Only microbiological studies of intraoperative tissue samples can give a definitive diagnosis. Pre-operative PET-CT and intraoperative frozen section is promising but not available in most centers. Thus, surgeons need to be prepared with multiple surgical options in the operating room. They should have several implants ready in their armamentarium including and not limited to plates, nails, external fixators, cement, thermostable antibiotics, etc., before operating these cases. The treatment of a potential low-grade infection should be a consideration in all non-union cases.
- Never rule out infection in a long bone non-union preoperatively. It is wise to consider a non-union as a septic one unless proven otherwise.
- Intraoperative tissue sampling for culture should be a dictum in such cases.
- Be prepared with all kinds of implants and accessories before taking on a non-union case.
- Interlocking nail coated with antibiotic cement is an effective single stage intervention which is easy to perform and economical for the management of septic non-union of tibia.
References
- 1.Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: The role of the biological chamber. Injury 2011;42:1191-3. [Google Scholar]
- 2.Calori GM, Albisetti W, Agus A, Iori S, Tagliabue L. Risk factors contributing to fracture non-unions. Injury 2007;38(Suppl 2):S11-8. [Google Scholar]
- 3.Rodriguez-Merchan EC, Forriol F. Nonunion: General principles and experimental data. Clin Orthop Relat Res 2004;419:4-12. [Google Scholar]
- 4.Fong K, Truong V, Foote CJ, Petrisor B, Williams D, Ristevski B, et al. Predictors of nonunion and reoperation in patients with fractures of the tibia: An observational study. BMC Musculoskelet Disord 2013;14:103. [Google Scholar]
- 5.Akhtar A, Shami A, Sarfraz M. Functional outcome of tibial nonunion treatment by Ilizarov fixator. Ann Pak Inst Med Sci 2012;8:188-91. [Google Scholar]
- 6.O’Halloran K, Coale M, Costales T, Zerhusen T, Castillo RC, Nascone JW, et al. Will my tibial fracture heal? Predicting nonunion at the time of definitive fixation based on commonly available variables. Clin Orthop Relat Res 2016;474:1385-95. [Google Scholar]
- 7.Brinker MR, Hanus BD, Sen M, O’Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am 2013;95:2170-6. [Google Scholar]
- 8.Kreder HJ. Tibial nonunion is worse than having a myocardial infarction: Commentary on an article by Mark R. Brinker, MD, et al.: The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am 2013;95:e1991. [Google Scholar]
- 9.Schmal H, Brix M, Bue M, Ekman A, Ferreira N, Gottlieb H, et al. Nonunion: Consensus from the 4th annual meeting of the Danish Orthopaedic Trauma Society. EFORT Open Rev 2020;5:46-57. [Google Scholar]
- 10.Harwood P, Newman J, Michael AL. An update on fracture healing and non-union. Orthop Trauma 2010;24:9-23. [Google Scholar]
- 11.Abumunaser LA, Al-Sayyad MJ. Evaluation of the calori et al. nonunion scoring system in a retrospective case series. Orthopedics 2011;34:359. [Google Scholar]
- 12.Perumal V, Roberts C. (ii) Factors contributing to non-union of fractures. Curr Orthop 2007;21:258-61. [Google Scholar]
- 13.Antonova E, Kim Le T, Burge R, Mershon J. Tibia shaft fracture-costly burden of nonunions. BMC Musculoskelet Disord 2013;14:42. [Google Scholar]
- 14.Tzioupis C, Giannoudis PV. Prevalence of long-bone non-unions. Injury 2007;38(Suppl 2):S3-9. [Google Scholar]
- 15.Aldemir C, Duygun F. Outcome of locked compressive nailing in aseptic tibial diaphyseal nonunions without bone defect. Indian J Orthop 2019;53:251-6. [Google Scholar]
- 16.Zimmerli W. Clinical presentation and treatment of orthopaedic implant-associated infection. J Intern Med 2014;276:111-9. [Google Scholar]
- 17.Kohlprath R, Assal M, Uçkay I, Holzer N, Hoffmeyer P, Suva D. Open fractures of the tibia in the adult: Surgical treatment and complications. Rev Med Suisse 2011;7:2482, 2484-8. [Google Scholar]
- 18.Bourguignat A, Férard G, Jenny JY, Gaudias J, Kempf I. Diagnostic value of C-reactive protein and transthyretin in bone infections of the lower limb. Clin Chim Acta 1996;255:27-38. [Google Scholar]
- 19.Arciola CR, Hänsch GM, Visai L, Testoni F, Maurer S, Campoccia D, et al. Interactions of staphylococci with osteoblasts and phagocytes in the pathogenesis of implant-associated osteomyelitis. Int J Artif Organs 2012;35:713-26. [Google Scholar]
- 20.Govaert GA, Bosch P, IJpma FF, Glauche J, Jutte PC, Lemans JV, et al. High diagnostic accuracy of white blood cell scintigraphy for fracture related infections: Results of a large retrospective single-center study. Injury 2018;49:1085-90. [Google Scholar]
- 21.Liodakis E, Liodaki E, Krettek C, Citak M, Gaulke R, Konstantinidis L, et al. Can the viability of a nonunion be evaluated using SPECT/CT? A preliminary retrospective study. Technol Health Care 2011;19:103-8. [Google Scholar]
- 22.Hoit G, Bonyun M, Nauth A. Hardware considerations in infection and nonunion management: When and how to revise the fixation. OTA Int 2020;3:e055. [Google Scholar]
- 23.Thonse R, Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma 2007;21:258-68. [Google Scholar]
- 24.Paley D, Herzenberg JE. Intramedullary infections treated with antibiotic cement rods: Preliminary results in nine cases. J Orthop Trauma 2002;16:723-9. [Google Scholar]
- 25.Nelson CK, Hickmon SG, Harrison BH. Elution characteristics of gentamicin-PMMA beads after implantation in humans. Orthopedics 1994;17:415-6. [Google Scholar]
- 26.Lei H, Yi L. One-stage open cancellous bone grafting of infected fracture and nonunion. J Orthop Sci 1998;3:318-23. [Google Scholar]