These findings encourage the development of specific treatment protocols with CDT to heal hematoma and edema, enhance tissue regeneration, and improve functional recovery after trauma or surgical interventions.
Dr. Eric Choudja Ouabo, Private Practice, Center of Orthopedic Surgery, Clinique Bois-Cerf, 1006 Lausanne, Switzerland. E-mail: e_choudja@hotmail.com
Introduction: Carbon dioxide therapy (CDT) has been used since the Roman Empire to improve the microcirculation and oxygenation of tissues altered. The classical indications are vasculopathies and ischemic diseases.
Hypothesis: The CDT could be effective in favoring joint mobility recovery and pain reduction in patients with post-surgical or post-traumatic hematoma, edema, and pain.
Study Design: Case report.
Materials and Methods: Eight patients were treated once a day for 5–10 days; a single session lasted 50 min. For post-surgical cases, the treatment began the day or the day after they were discharged from the hospital.
Results: For all patients in this series, the CDT has brought clinical benefits in terms of decreasing pain and improving of joint mobility.
Conclusion: The CDT is a safe and effective treatment to provide a greater amount of oxygen to the injured tissues. It favors the healing of post-surgical and post-traumatic hematoma and edema, promoting the mobility recovery of patients.
Keywords: Carbon dioxide therapy, hematoma, edema, pain, mobility recovery, case report.
The term “carboxytherapy” has appeared for the first time in the scientific community in 1995 by Parassoni during the XVI National Assembly of Aesthetic Medicine in Rome, and it refers to the transcutaneous or percutaneous administration of CO2 with therapeutic purposes [1]. Carbon dioxide therapy (CDT) finds its origins in Royat, France, where the first Roman spa called “Rubiacum” (because of rosy water contenting ferrum) was found, dating to 20 BC during the empire of Augustus. It arouses the interest of people even in the following eras, like the Celts, who worshiped this place as miraculous, but, however, after the invasion of the Barbarians in the 5th century, the site was forgotten [2]. Later, in 1932, Barrieu first treated patients with arterial and venous disorders with CO2 spring gas injections [3]. In 1946, in France, the Institute of Research of Royat was inaugurated, managing to produce during the second half of the century nearly 400 publications about carboxytherapy, also called carbocrenotherapy [2]. Over the years, CDT has found considerable development until a consensus regarding the effects of CO2 was formulated during the International Conference in Freiburg-en-Breisgau, Germany, in 1989 and 1999. The following therapeutic effects were highlighted in consensus: (a) local increase of blood supply and opening of functionally closed capillaries; (b) dilatation of precapillary segments; (c) improvement of tissue oxygenation by arterial increased liberation of oxygen; (d) improved deformability of erythrocytes; (e) modification of threshold of thermoreceptors; (f) antiseptic effect [4, 5]. The physiopathological bases of these therapeutic effects reside in the administration of CO2, which improves the arterial blood flow, the microcirculation, and increase the tcPO2 in ischemic tissues, which is explained by the Bohr effect. In fact, the presence of CO2 causes a rightward shift of the O2-Hb dissociation curve with a consequent increase in pCO2 or decrease in pH. In lower pH and higher pCO2, the affinity of hemoglobin to oxygen is decreased [6]. The traditional therapeutic indication is vasculopathy or ischemic diseases, including diabetic periphery syndrome, Morbus Buerger, Reynaud’s syndrome, chronic venous insufficiency, chronic venous-lymphatic insufficiency, and recently also erectile dysfunction associated with microangiopathy. The CDT has found indications in other branches of medicine, such as dermatology, where this method is very useful in wound healing, including leg ulcers and hair disorders, and helps to improve psoriasis and sclerodermia [6]. Depending on the method of administration of CO2, different types of treatment are available: (a) use of spa therapy like in Royat Center; (b) use of artificial CO2-enriched water for bathing to improve ischemic limb symptoms; (c) subcutaneous injection of CO2 in plastic surgery; (d) percutaneous administration of CO2-rich spa gas [7]. Considering all these indications, the different methods, and the effects of CDT, the authors have assumed clinical benefits in other ischemic disorders like hematoma: A blood collection inside a tissue following a breaking blood vessel involved a reduction of oxygen in the affected tissues, which showed signs of adaptation to hypoxia [8]. The aim of the present article was to expose the effects of percutaneous CDT on the healing of wounded tissues in patients with post-surgical and post-traumatic hematoma, edema, and pain. Better oxygenation has an anti-inflammatory effect and decreases pain.
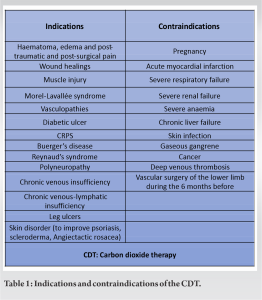
Between the patients treated from 2019 to 2022, we selected 8 patients, 2 men and 6 women, with a mean age of 56.8 years (range 36–72 years), who were treated at the Center of Surgery, Hand, and Aesthetics in Lausanne, Switzerland. Informed consent was obtained from all patients, and the rights of the subjects were protected. The device used was the CARBO® Fit system produced by Derma Art, Slovenia. Their selection is based on the presence of hematoma, edema, pain, and joint functional reduction after a trauma (3 patients) or a surgical intervention (5 patients). The patients were treated once a day for 5–10 days. For post-surgical cases, the treatment began the day or the day after they were discharged from the hospital. A clinical examination was conducted to check the correct indication for the CDT and to exclude any contraindications during the first day of therapy (Table 1). In view of the fact that the effect of CDT depends on many effects (its concentration, surface area exposure, contact time, skin temperature, number, and frequency of sessions), the number of sessions is variable depending on the patient’s clinical condition and his evolution after the first or second CDT treatment. In some acute cases, double-daily administration may be indicated. During the treatment, the patient is positioned supine on the table, and the body region to be treated is covered with a sealed envelope (Fig. 1a and b). The ambient air is removed and replaced with 99.5% medical carbon dioxide at a pressure of 49.5 bars at 15°C. The quantity of CO2 used depends on the body surface to be treated; generally, we use between 0.25 and 0.3 L of CO2 per session. A single session lasted 50 min. The patient is comfortable and can relax by reading a book, listening to music, or sleeping. If necessary, during the wintertime, the skin is heated for a few minutes stay in an infrared sauna, which increases the passage rate of carbon dioxide.
Post-traumatic cases
Case No. 1: A 76-year-old male patient (70 kg, 172 cm) was evaluated for strong leg pain (visual analog scale [VAS]: 8/10) after a fall on skiing. He walked with crutches without leaning his foot on the ground, with a limited extension of 30° of the left knee.

Case No. 2: A 57-year-old female patient (58 kg, 173 cm) had shown up for a severe ankle sprain (initial VAS: 5/10); she walked with crutches and presented edema and hematoma on the peroneal side (Fig. 3a). The indication was given for carboxytherapy treatment: 1 time a day for 5 days. After 1 day of therapy, the malleolar swelling was greatly decreased (Fig. 3b); after 4 days, the malleolar edema disappeared, and the hematoma was almost completely reduced (Fig. 3c). After 6 days from her accident, the patient returned to sport, and she resumed swimming (final VAS: 0–1/10).
Case No. 3: A 47-year-old female patient (60 kg, 168 cm) was evaluated after a scooter accident. Clinically, she presented right zygomatico-maxillary fractures and an extended hematoma and edema on the whole lower limb with almost full limitation of knee mobility (Fig. 4a). The diagnosis of Morel-Lavallée syndrome was posed (initial VAS: 7–8/10). The knee blending was surgically drained, with post-operative improvement of knee flexion up to 80° (Fig. 4b). A few days later, treatment for CDT was initiated. After 10 days of treatment, the patient had no pain anymore, and the hematoma and edema were greatly reduced. Moreover, the knee flexion was improved by up to 120° (final VAS: 1–2/10) (Fig. 4c and d).
Post-surgical cases
Case No. 4: A 36-year-old male patient (72 kg, 178 cm) consulted 3 days after arthroscopic combined anterior cruciate ligament and anterolateral reconstruction with hamstring autograft complaining pain and knee limited extension at 25° and flexion at 60° (VAS: 8–9/10) (Fig. 5a and b) despite taking strong doses of antalgic drugs. After a cycle of seven sessions of carboxytherapy, the patient had no pain anymore and an improved knee range of motion: a complete extension and flexion of 90° (final VAS: 1–2/10) (Fig. 5c). He was now able to begin post-surgical rehabilitation.
Case No. 5: A 59-year-old female patient (60 kg, 174 cm) was evaluated 4 days after a bilateral Revel osteotomy of the 1st metatarsus and Akin osteotomy of the 1st phalanx foot and percutaneous pinning of the 2nd toe of the left foot for bilateral hallux valgus and claw toe (Fig. 6a and b). She took a triple dose of NSAIDs and paracetamol for pain control (initial VAS: 7–8/10). After 3 carboxytherapy sessions, the patient was able to stop any medication, and the edema was sharply reduced. After 7 sessions of therapy, she had no pain anymore (VAS: 1–2/10) (Fig. 6c).
Case No. 6: A 62-year-old female patient (50 kg, 165 cm). The patient had on the left foot a plate removal of the second metatarsal bone and a resection of an exostosis of the navicular bone. In the same operation, she also had on the right foot a Revel osteotomy of the 1st metatarsal bone, an Akin osteotomy of the first phalanx of the great toe, and an exostosis resection (Fig. 7a). She complained of important post-operative pain and edema of both feet and a slight dehiscence of the osteotomy scar (initial VAS: 6–7/10) (Fig. 7b). Treatment with carboxytherapy was indicated. After 7 sessions of CDT, the patient had no pain anymore, and the edema was clearly reduced (VAS: 1–2/10) (Fig. 7c).
Case No. 7: A 60-year-old female patient (65 kg, 170 cm) was evaluated after total knee arthroplasty with anterior tibial tuberosity osteotomy of the right knee for tricompartmental knee osteoarthritis with patella baja. She is complaining of pain, edema, and hematoma of the entire inferior leg (initial VAS: 9/10) (Fig. 8a and b). A clear clinical improvement was obtained after 10 sessions of CDT: almost complete pain disappeared and there was sharp reduction of hematoma and edema (final VAS: 2–3/10) (Fig. 8c).
Case No. 8: A 58-year-old female patient (79 kg, 157 cm) presented with hematoma of the leg after a tibial open wedge high tibia osteotomy left knee for varus medial femoro-tibial osteoarthritis, complaining of pain and reduced knee mobility (40° of knee flexion). She takes NSAIDs and morphine derivates (tramadol chlorhydate) (VAS: 9/10) (Fig. 9a and b). She was treated for 8 days with CDT and reported favorable clinical results: improvement of knee range of motion (knee flexion at 85°) and reduction of hematoma. After 4 days, she gave up tramadol chlorhydate, and after 8 days, she only takes NSAIDs if needed (VAS: 2/10) (Fig. 9c and d).
For all patients in this series, the CDT has brought clinical benefits in terms of decreasing edema, pain, and improving joint mobility (Table 2).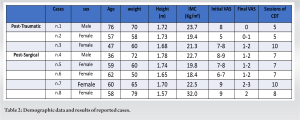
CDT is a safe and effective treatment to provide a greater amount of oxygen to the injured tissues. This series highlights his favorable clinical benefits for patients with post-surgical and post-traumatic hematoma, edema, and pain. Further studies are needed to confirm these promising results.
- The use of percutaneous coroxytherapy, started between D0 and D7, has a clear analgesic effect and allows faster functional recovery.
- Some contraindications to CTP treatment must be respected, as listed in Table 1.
References
- 1.Varlaro V, Manzo G, Mugnaini F, Bisacci C, Fiorucci P, De Rango P, et al. Carboxytherapy: Effects on microcirculation and its use in the treatment of severe lymphedema. Acta Phlebol 2007;8:79-91. [Google Scholar]
- 2.Fabry R, Dubost JJ, Schmidt J, Body J, Schaff G, Baguet JC. Thermal treatment in arterial diseases: An expensive placebo or an effective therapy? Therapie 1995;50:113-22. [Google Scholar]
- 3.Barrieu M. Royat thermal gas subcutaneous injections. Maroc Med 1949;28:265. [Google Scholar]
- 4.Body J, Morel F, Schaff G. Effets vaso-actifs du CO2 thermal. Angeiologie 2000;52:71-5. [Google Scholar]
- 5.Finzgar M, Melik Z, Cankar K. Effect of transcutaneous application of gaseous carbon dioxide on cutaneous microcirculation. Clin Hemorheol Microcirc 2015;60:423-35. [Google Scholar]
- 6.Sakai Y, Miwa M, Oe K, Ueha T, Koh A, Niikura T, et al. A novel system for transcutaneous application of carbon dioxide causing an ‘‘artificial bohr effect’’ in the human body. Plos One 2011;6:e24137. [Google Scholar]
- 7.Ito T, Moore JI, Koss MC. Topical application of CO2 increases skin blood flow. J Invest Dermatol 1989;93:259-62. [Google Scholar]
- 8.Brandi C, Grimaldi L, Nisi G, Brafa A, Campa A, Calabrò M, et al. The role of carbon dioxide therapy in the treatment of chronic wounds. In Vivo 2010;24:223-6. [Google Scholar]
- 9.Jackson DW, Feagin JA. Quadriceps contusions in young athletes. Relation of severity of injury to treatment and prognosis. J Bone Joint Surg Am 1973;55:95-105. [Google Scholar]
- 10.Pinheiro NM, Crema VO, Millan BM, Carvalho FA, Mendonca AC. Comparison of the effects of carboxytherapy and radiofrequency on skin rejuvenation. J Cosmet Laser Ther 2015;17:156-61. [Google Scholar]
- 11.Pianez LR, Custódio FS, Guidi RM, De Freitas JN, Sant’Ana E. Effectiveness of carboxytherapy in the treatment of cellulite in healthy women: A pilot study. Clin Cosmet Investig Dermatol 2016;9:183-90. [Google Scholar]
- 12.King S, King M. Using carboxytherapy as an adjuvant aesthetic treatment for patients with alopecia. J Aesthetic Nurs 2013;2:434-5. [Google Scholar]