LEH can be radiographically misdiagnosed or missed but its singular clinical presentation is diagnostic. In our case, the clinical diagnosis leads us to treat it with an early and appropriate closed method of reduction.
Maria Grazia Minicelli, Department of Orthopaedic Surgery of Pugliese Hospital, University Hospital Renato Dulbecco, viale Pio X n. 83, 88100 Catanzaro, Italy. E-mail: mariagraziaminicelli@tiscali.it
Introduction: Luxatio erecta humeri (LEH) is a rare type of inferior shoulder dislocation (ISD) and easy misdiagnosed or missed. We reported a case of a traumatic LEH with a radiological interpretation of ISD. We felt that the physical presentation was compatible with the LHE type and the closed reduction by the traction and countertraction method we accomplished without complications.
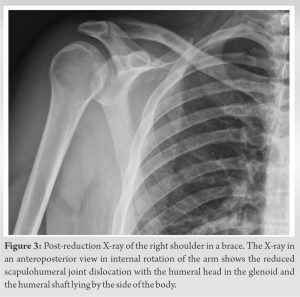
Case Report: We present a case of 38-year-old man with a LEH. We performed for the early diagnosis the clinical examination and the X-rays. We felt that the physical presentation was compatible with an erecta dislocation of the humerus, whereas radiologically, this injury was interpreted simply as the inferior dislocation of the right shoulder. The closed reduction by the traction and countertraction method was accomplished without complications. We kept the reduction with a Velpeau arm sling shoulder immobilizer brace for 3 weeks and after a shoulder rehabilitation, the outcome was good.
Conclusion: The luxation erecta humeri is a type of ISD still little known but the singular and unmistakable physical presentation should allow for an early diagnosis to obtain an easy closed reduction and a good outcome.
Keywords: Luxation erecta humeri, inferior shoulder dislocation, case report.
Luxatio erecta humeri (LEH) is an unusual injury. This dislocation is described in a series of cases reported in the literature [1-7] and recently identified a total of 199 patients [8]. Most cases can be treated with closed reduction and immobilization, but in case of irreducibility, it requires reduction under general anesthesia and/or further operative measures. The surgery is also reserved for patients with recurrent instability, open dislocation, or humeral fractures [4]. We present a case of an acute traumatic LEH reduced without anesthesia and treated with a Velpeau arm sling shoulder immobilizer brace.
A 38-year-old man, right-handed and healthy presented to our emergency room due to a fall. The patient reported that he had stumbled while walking and he fell backwards to the ground with the abducted right arm. The physical presentation of the right upper limb was distinctive: The elbow flexed, the forearm, and the hand pronated lying behind the patient’s head with the arm elevated and hyperabducted at the shoulder. He was setting with the left hand that grabbed the contralateral hand (Fig. 2a). At physical examination, this right arm position was fixed for the pain, the humeral head prominence was visible and palpable in the axilla, and there were no wounds and neurovascular deficits. We performed anteroposterior (AP) view of the right shoulder in the scapular plane projection and the comparative view X-ray that were interpreted simply as the inferior dislocation of the right shoulder (Fig. 1).

The LEH is a rare traumatic type of inferior shoulder dislocation (ISD). This injury represents only 0.5% of all shoulder dislocations. There are two mechanisms causing the ISD. The first mechanism is a hyperabduction force to an already abducted arm in which the acromion acts as lever on proximal humerus, and the second mechanism is an axial compression on the abducted arm in which a direct load of the humeral head breaks the capsule and the inferior glenohumeral ligaments. The ISD in 12% of cases is caused by the fall from standing height [8]. In our case, the LEH was caused by a low-energy trauma as a fall backward to the ground while the patient walking. Probably, both a hyperabduction force to an abducted arm to defend the skull from the impact on the ground and the axial load as a body weight on humeral head caused the LEH. The clinical presentation of LEH is distinctive, unmistakable, and diagnostic. In our case, the singular and fixed attitude of the arm elevated and hyperabducted at the shoulder and the forearm and the hand pronated lying behind the head, with the humeral head prominence visible and palpable in the axilla, helped us in the diagnosis before the radiographic examination. It is distinctive of LEH an abducted arm over 90° [1]. Some complications are reported for the LEH as fractures of acromion, greater tuberosity, humeral head, glena, clavicle, coracoid, furthermore, may be present with the LEH glenohumeral cartilage or capsular defects, rotator cuff and labral tears, humeral avulsion of glenohumeral ligament, disruptions of the adjacent muscles [5,9,10]. Severe or transient neurovascular injuries of brachial plexus, axillary nerve, radial and ulnar nerves may be associated with luxatio erecta [6]. In our case no fractures and no neurological deficits were present. There are two types of inferior dislocations shoulder joint: The sub glenoid dislocation and the true erecta dislocation. In the sub glenoid dislocation, the humeral head is locked in the sub glenoid region without the hyper abducted posture with the arm lying by the side of the body in neutral position [11]. This dislocation can be reduced with a traction on the arm and the lateral thrust of the humeral head and at the same time with a direct downward pressure on the top of the acromion. Instead, typical features of LEH in AP and in Y lateral views X-rays of the shoulder are the humeral head below the inferior rim of the glenoid or in sub coracoid location with abducted humeral shaft almost parallel to the scapular spine [1- 5]. We reported a case of LEH with suspicious and unclear signs of inferior dislocation of the right shoulder in AP view X-ray and for this reason, it was necessary to perform the comparative view X-ray in the scapular plane projection. The comparative projection confirmed more clearly the inferior dislocation of the head of the right shoulder with the abducted arm over 90° compared to the contralateral and the humeral shaft almost parallel to the scapular spine. In our case, we felt that the physical presentation was compatible with the diagnosis of an erecta dislocation of the humerus and the closed reduction by the traction and countertraction method was accomplished without complications as well as in the cases reported by Isaac Grate [12] and with a good outcome. We describe a clinical presentation of LEH with a missed or not specified radiographic interpretation. The LEH may be misdiagnosed or missed but the physical presentation and examination are diagnostics [12]. This is important for the prognosis of this dislocation that is directly influenced by early diagnosis and successful reduction [4, 10].
The fixed attitude of the arm elevated and hyper abducted at the shoulder and the forearm and the hand pronated lying behind or in front of the skull with the humeral head prominence visible and palpable in the axilla are diagnostic features of the luxation erecta humeri. Radiographically, this injury can be missed or misdiagnosed. In our case, we felt that the physical presentation was compatible with the diagnosis of erecta dislocation of the humerus and the closed reduction by the traction and countertraction method was accomplished without complications.
LEH is a rare type of traumatic ISD and for this reason can be radiologically misdiagnosed or missed, but the singular physical presentation, and the humeral head prominence visible and palpable in the axilla are diagnostics and the closed reduction by the traction and countertraction can be performed.
References
- 1.Diallo M, Kassé AN, Mohamed LS, Sané JC, Dembélé B, Sy MH. Erecta dislocation of the shoulder joint- a rare injury: about four cases. Clin Case Rep 2019;7: 1319-22. [Google Scholar]
- 2.Cift H, Soylemez S, Demiroglu M, Ozkan K, Ozden VE, Ozkut AT. Rare inferior shoulder dislocation (Luxatio Erecta). Case Rep Orthop 2015; 12:624310. [Google Scholar]
- 3.Martinez-Romo MA, Lotfipour S, McCoy CE. Bilateral luxatio erecta humeri. Clin Pract Cases Emerg Med 2021; 5:249-50. [Google Scholar]
- 4.Ngam PI, Hallinan JT, Sia DS. Sequelae of bilateral luxatio erecta in the acute post-reduction period demonstrated by MRI: A case report and literature review. Skeletal Radiol 2019; 48:467-73. [Google Scholar]
- 5.Petty K, Price J, Kharasch M, Novack J. Bilateral luxatio erecta: A case report. J Emerg Med 2014; 46:176-9. [Google Scholar]
- 6.Kaziz H, Triki MA, Benzarti S, Mouelhi T, Naouar N, Ayeche ML. Inferior dislocation of the shoulder complicated with brachial plexus palsy: A case report. J Musculoskelet Disord Treat 2018; 4:056. [Google Scholar]
- 7.Khedr H, Al-Zahrani A, Al-Zahrani A, Al-Qattan MM. Bilateral irreducible inferior shoulder dislocation: A case report. Int J Surg Case Rep 2017; 31:124-7. [Google Scholar]
- 8.Nambiar M, Owen D, Moore P, Carr A, Thomas M. Traumatic inferior shoulder dislocation: A review of management and outcome. Eur J Trauma Emerg Surg 2018; 44:45-51. [Google Scholar]
- 9.Hassanzadeh E, Chang CY, Huang AJ, Shaqdan K, Mansouri M, Aran S, Abujudeh HH. CT and MRI manifestations of luxatio erecta humeri and a review of the literature. Clin Imaging. 2015;39(5):876-9. [Google Scholar]
- 10.Groh GI, Wirth MA, Rockwood CA. Results of treatment of luxatio erecta (inferior shoulder dislocation). J Shoulder Elbow Surg. 2010;19(3):423-6. [Google Scholar]
- 11.Sonanis SV, Das S, Deshmukh N, Wray C. A true traumatic inferior dislocation of shoulder. Injury 2002; 33:842-4. [Google Scholar]
- 12.Grate I Jr. Luxatio erecta: A rarely seen, but often missed shoulder dislocation. Am J Emerg Med 2000; 18:317-21. [Google Scholar]