Early diagnosis and timely intervention would be the cornerstone of the vascular injury following total hip arthroplasty.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr. MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: Vascular injury following total hip arthroplasty (THA) is uncommon but can lead to loss of life or limb. External iliac and common femoral arteries are commonly injured during THA.
Case Report: We report a case of thrombosis of the external iliac and femoral artery during THA in a mid-60-year female patient with 15-year-old neglected fracture neck of the femur. Six hours following THA through Harding’s approach, a feeble pulse was palpated in the operated limb. Ischemia of the limb led to sciatic nerve palsy and foot drop in the operated limb, which was intact following surgery. Computed tomography angiography confirmed thrombosis of the external iliac and femoral artery. Removal of thrombosis with the use of a Fogarty catheter could save the limb and lead to recovery of foot drop. Early detection of pulselessness and timely intervention in the post-operative period was the cornerstone of this case report.
Conclusion: Vascular injury during THA though rare but cannot be ruled out completely. Early diagnosis with a stringent post-operative protocol and timely intervention would be the cornerstone of the management of any vascular injury following THA.
Keywords: Thrombosis, arthroplasty, external iliac artery, angiography.
Vascular complications during total hip arthroplasty (THA) are rare, accounting for <0.04% of primary THA and 0.2% of revision THA. Vascular complication following THA has led to amputation in 15% of cases, permanent disability in 17%, and mortality in 7–9% [1]. THA involves soft-tissue release, retraction of soft tissue, use of spike retractors, and drilling through the acetabulum. Each surgical step carries a different degree of risk to iliac vessels and femoral vessels [2,3]. In addition to indirect trauma, direct trauma or compression by prosthetic components such as screws, cement, cables, anti-protrusio cages, threaded acetabular components, or structural allografts can injure vascular structures. The vicinity of some vessels in the surgical field put them more prone to injury. The external iliac vein lies within 7 mm of the anterior column of the pelvis at the level of the anterior inferior iliac spine and within 4 mm at the acetabular dome. The external iliac artery lies within 10 mm of the bone at the level of the anterior inferior iliac spine and within 7 mm at the acetabular dome. The external iliac artery has thicker intima and is far from the bone compared to the external iliac vein. The femoral artery is situated anteriorly and medial to the hip capsule. The iliopsoas muscle usually protects the femoral artery during surgery at the level of the hip joint. The femoral vein lies medial to the artery and is less likely to be injured. The obturator vessel is also at risk of injury, being situated within 2 mm of quadrilateral bone, and just separated by the obturator internus muscle. We have performed more than 500 THA in the past 7 years and encountered the first case of vascular injury during THA. We present a case of vascular injury during THA leading to thrombosis of the external iliac artery. Gradual obliteration of external iliac vessels due to intramural thrombosis led to a compromise in blood supply to the lower limb. The patient developed sciatic nerve palsy and foot drop following ischemia of the lower limb. The function of the sciatic nerve was intact in the early post-operative period but developed palsy nearly 2 h following the obliteration of distal pulsation of the limb. Timely assessment and intervention could save the limb and reverse sciatic nerve palsy. This case carries a significant learning aspect for us and for other hip replacement surgeons who have not encountered such an incident.
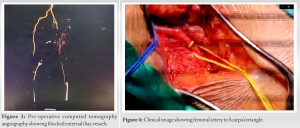
A mid-60-year female presented with complaints of pain in her left hip for 6 months associated with limping for the past 10 years. The patient had a fall 15 years back and was treated by a general physician and she was able to walk without support for the next 5 years. In the past 10 years, her limping progressed gradually to the present state, interfering in her daily life. The pain and limping were remarkable in the past 6 months which forced her to seek medical management. The attitude of the left lower limb was flexed, abducted, and externally rotated. Movement of the left hip was painful and restricted to a few degrees. The left lower limb had a true shortening of 6 cm due to proximal migration of the trochanter. Limb length was compensated to some degree by pelvic obliquity. The neurovascular status of both the lower limb was normal without any radiculopathy before surgery. All the peripheral pulses including femoral and popliteal arteries were well felt in the affected limb and comparable to the normal side. A radiograph of the pelvis revealed; an old fracture of the neck of the femur, pelvis tilted downward to the affected side, decreased joint space of hip joint, osteophytes inferiorly to the head of the femur, proximal migration of trochanter, etc. The tip of the trochanter is abutting against the ilium with a visible callus between the trochanter and ilium with exuberant callus all around (Fig. 1 and 2).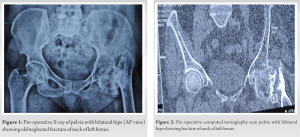
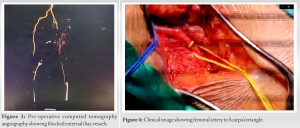

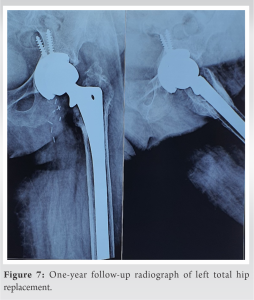
THA is associated with numerous complications, such as prosthetic joint infection, dislocation of prosthesis, limb length discrepancy, and sciatic nerve injury [4]. Vascular complications following THA are rare and its documentation in the literature is meager [5,6]. Vascular injuries are unfortunate for a surgeon as they can result in the loss of a patient’s limb or life [7-9]. Vascular injuries can be the result of direct injury by prosthetic components such as screws, cement, cables, anti-protrusio cages, and threaded acetabular components, or by indirect trauma due to extensive soft-tissue release, retraction of soft tissue, use of spike retractors, and drilling through the acetabulum [2, 3, 10]. In our case, as we retrospect; intraoperatively, we had to struggle to keep the spike against the anterior wall of the acetabulum. The anterior wall of the acetabulum was soft and used to cut out with the use of an anterior spike. We had a tough time retracting the anterior soft tissue to have a proper view of the acetabulum. There were multiple attempts to put the anterior retractor to have a good vision for the procedure. We attribute this step as a contributing factor for the formation of intimal injury to the common femoral artery and thrombus formation that later extended to the external iliac artery. The most common vessel to get injured in THA are the external iliac artery and common femoral artery [10]. Intraoperative bleeding was more than normal THA. A feeble pulse in the early post-operative period could not be ascertained as vascular injury as there was a good amount of blood loss during surgery. Besides, as it was the first incident for the surgical team, a hidden vascular injury was not the first diagnosis. The absence of a peripheral pulse in the operated limb after 6 h of surgery was the turning point for the team to act accordingly. For the past 15 years, it is our routine practice to evaluate the operated limb neurovascular status for 12 h following surgery. Our protocol has helped us to save the limb of this patient. As the patient was in a tertiary center, it was possible to arrange the preliminary investigations to reach the diagnosis and intervene at the earliest possible time. The patient was operated on the midnight within 12 h of index surgery by a vascular surgeon and orthopaedician. Thrombus from the external iliac and femoral artery was removed with the help of a Fogarty catheter. The patient regained normal blood flow within seconds of the removal of the thrombus. After weaning of spinal anesthesia effect, the patient regained normal motor and sensory activities in the operated limb. Knee, ankle, and toe movement of the operated limb had normal movement. After the onset of ischemia following thrombosis in the external iliac artery, the patient developed a foot drop in the operated limb. We were not able to ascertain the cause of the foot drop, either due to muscle ischemia or sciatic nerve ischemia. Within an hour of thrombectomy and reperfusion of the lower limb patients’ foot drop improved completely. One possibility could be an impending sciatic nerve ischemic damage that recovered following regain of blood supply.
Vascular injury during THA though rare but cannot be ruled out completely. Early diagnosis with a stringent post-operative protocol and timely intervention would be the cornerstone of the management of any vascular injury following THA. Thrombectomy if done in time can prevent irreversible disability.
CT angiography confirmed thrombosis of the external iliac and femoral artery. Removal of thrombosis with the use of a Fogarty catheter could save the limb and lead to recovery of foot drop. Early detection of pulselessness and timely intervention in the postoperative period was the cornerstone of the article.
References
- 1.Abularrage CJ, Weiswasser JM, Dezee KJ, Slidell MB, Henderson WG, Sidawy AN. Predictors of lower extremity arterial injury after total knee or total hip arthroplasty. J Vasc Surg 2008;47:803-7; discussion 807-8. [Google Scholar]
- 2.Wasielewski RC, Galat DD, Sheridan KC, Rubash HE. Acetabular anatomy and transacetabular screw fixation at the high hip center. Clin Orthop Relat Res 2005;438:171-6. [Google Scholar]
- 3.Keating EM, Ritter MA, Faris PM. Structures at risk from medially placed acetabular screws. J Bone Joint Surg Am 1990;72:509-11. [Google Scholar]
- 4.Avisar E, Elvey MH, Bar-Ziv Y, Tamir E, Agar G. Severe vascular complications and intervention following elective total hip and knee replacement: A 16-year retrospective analysis. J Orthop 2015;12:151-5. [Google Scholar]
- 5.Alshameeri Z, Bajekal R, Varty K, Khanduja V. Iatrogenic vascular injuries during arthroplasty of the hip. Bone Joint J 2015;97-B:1447-55. [Google Scholar]
- 6.Vetrhus M, Nybø TM, Stokkeland PJ, Young S. Delayed diagnosis of a late vascular complication after total hip replacement. EJVES Extra 2009;18:51-2. [Google Scholar]
- 7.Doi S, Motoyama Y, Itoh H. External iliac vein injury during total hip arthroplasty resulting in delayed shock. Br J Anaesth 2005;94:866. [Google Scholar]
- 8.Bergqvist D, Carlsson AS, Ericsson BF. Vascular complications after total hip arthroplasty. Acta Orthop Scand 1983;54:157-63. [Google Scholar]
- 9.Burlage E, Gerbers JG, Geelkerken BR, Verra WC. External iliac artery injury following total hip arthroplasty via the direct anterior approach-a case report. Acta Orthop 2020;91:485-8. [Google Scholar]
- 10.Shoenfeld NA, Stuchin SA, Pearl R, Haveson S. The management of vascular injuries associated with total hip arthroplasty. J Vasc Surg 1990;11:549-55. [Google Scholar]









