Permanent subluxation of lateral meniscus is a rare entity, impossible to diagnose with clinical and radiological examination, with a guarded prognosis.
Dr. Deven R Kuruwa, Department of Orthopaedics, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, India. E-mail: generalkuruwa@gmail.com
Introduction: Locking of the knee attributed to non-discoid lateral meniscus in an atraumatic setting is a rare phenomenon. One such cause is permanent subluxation of lateral meniscus (PSLM). In the entire literature, there is only one documented case of a 37-year-old female.
Case Report: We present a case of a 10-year-old boy who suffered two episodes of knee locking reported radiologically as a bucket handle tear of the lateral meniscus. No tear was found during arthroscopy. The lateral meniscus was malformed with meniscocapsular discontinuity and irreducibly subluxated into the intercondylar space. No salvage procedure was possible. We ended up performing a subtotal meniscectomy.
Conclusion: This is the first case of PSLM reported in the pediatric age group and second overall. Management options are limited. Further genetic and fetal studies are needed in this area to determine the exact causality.
Keywords: Permanent subluxation of lateral meniscus, lateral meniscus malformation, irreducible non-discoid lateral meniscus, meniscocapsular discontinuity.
Discoid lateral meniscus, meniscus tears, and loose bodies are common causes of knee locking in the pediatric age group [1-3]. Hypermobility and subluxation of the lateral meniscus are rare entities which can cause atraumatic knee pain and locking [3, 4]. Patients with hypermobility present with knee pain with or without locking, and the characteristic feature is an intact meniscus with abnormal mobility when probed [3]. The posterior segment of the lateral meniscus is the culprit in most cases, although a solitary case attributing hypermobility to the anterior segment has been reported [3-7]. Subluxations of the lateral meniscus can be recurrent or permanent, always present with episodes of locking [8]. Recurrent subluxation of the lateral meniscus (RSLM) is characterized by the ability of the posterior segment of the lateral meniscus to displace anteriorly only during episodes, whereas in permanent subluxation of the lateral meniscus (PSLM), the posterior segment stays displaced anteriorly [8, 9]. PSLM is so rare that it has only been reported once [9]. We report a case of PSLM in a 10-year-old child who presented to us with two episodes of knee locking without any history of trauma. This is the youngest and only the second case of PSLM reported in literature.
A 10-year-old male child, an aspiring footballer, presented to our clinic with an insidious onset of right knee pain in October 2022. The pain was intermittent on the lateral aspect of the knee with no association with the level of his physical activity. He later suffered two episodes of knee locking. The first episode occurred in March 2023, lasted 5 minutes, and reduced on its own. There was no history of trauma or twisting injury. The last episode occurred in May 2023. Only this time, the knee stayed locked. Family history was negative for similar episodes of knee pain and locking. On examination during the first consultation, he only had mild lateral joint line tenderness. There was no effusion, range of motion (ROM) was complete without any audible click. Clinical tests for meniscus tear were negative. Findings were the same when his knee locked for the first time. After the second episode, lateral joint line tenderness was aggravated with painful ROM between 30 and 50 degrees of flexion without effusion. Magnetic resonance imaging (MRI) of the right knee was done after the first episode. It revealed a bucket handle tear of the lateral meniscus with displacement in the intercondylar notch and a 10 × 15 mm lesion in the subchondral bone at the center of the lateral femoral condyle with intact articular cartilage (Fig. 1a and b). 

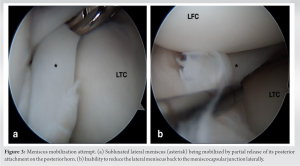
There are very few case series or cases reported in literature attributing atraumatic knee locking to non-discoid lateral meniscus pathology [1, 7, 10]. The pathoanatomic features in our case painted a picture of congenital or developmental malformation rather than a tear. Hypermobile meniscus is an established cause of knee pain and locking. It is characterized by an innocuous-looking MRI and the ability of the meniscus to displace beyond the lateral condyle of the femur on probing during arthroscopy [3, 5]. The posterior part of the lateral meniscus is the culprit in most of the cases due to disruption of the popliteo-meniscal fascicles near the popliteal tendon [3-6]. A solitary case of hypermobile lateral meniscus due to the anterior horn has also been reported [7]. In contrast, the MRI of our patient showed a displaced bucket handle lateral meniscus tear resembling the flipped meniscus sign described by Haramati et al. [11]. It is commonly associated with subluxated lateral meniscus [8]. Arthroscopy also revealed a non-reducible hypomobile lateral meniscus. The findings in our patient resemble a case of PSLM by Suganuma et al. [9] in a 37-year-old female. They reported that she had no history of trauma or locking symptoms. The middle segment of the lateral meniscus was dislocated anteriorly, and the posterior segment was in the intercondylar space in both knees. It could not be reduced due to adhesions in the intercondylar space. Her right knee which was more symptomatic had an osteochondral defect of 15 × 20 mm on the lateral femoral condyle. Suganuma et al. [9] stated that PSLM appeared to be related to both congenital and environmental factors, as the dislocated meniscus needs to be adhered to the surrounding tissue. However, as evident in our case, there was no adhesion between the meniscus and the intercondylar space. This could imply that the lesion is solely a congenital malformation. A late gestation period between 33 and 38 weeks has been postulated to cause lateral meniscus malformations [12]. During this interval, the fetal knee assumes a flexed posture from an extended position in the uterus. Internal rotation of the knee and disruption of the popliteo-meniscal fascicle have been proposed as risk factors for lateral meniscus subluxation [6, 8]. Once subluxated, it can reduce spontaneously during knee extension and failure to do so leads to irreducible subluxation. Sunguanuma et al. [9] did not perform any intervention for PSLM as the patient did not consent. Had she consented, they had a two-staged plan ready. The first stage would aim to release the adhesions between the meniscus and intercondylar space to reduce the meniscus back to normal position followed by casting for 3 weeks and rehabilitation. If recurrence occurred, meniscocapsular stabilization would be considered the second stage procedure. In our case, it was impossible to reduce the meniscus back due to the continuity of the outer aspect of the meniscus body directly with the anterior and posterior horns instead of the meniscocapsular junction. We attempted to mobilize the fragment with graduated junctional releases between the body and the horns to no avail. The only option we were left with was to leave the meniscus alone or sacrifice the dislocated chunk. Considering the history of locking, we decided to go ahead with subtotal meniscectomy. Had pain been the only symptom, we would have probably left the meniscus alone and observed. As opposed to PSLM, RSLM is a more common entity. It is characterized by repeated subluxations of the lateral meniscus which cause painful locking of the knee joint [8]. The subluxation is usually in the posterior segment, easily reducible without tears which makes them suitable for stabilization procedures [13, 14]. Hence, it carries a better prognosis than PSLM. The lateral meniscus absorbs more shock than the medial meniscus [15]. Young, active patients develop lateral compartment arthritis rapidly within a few months after partial or subtotal menisectomy [15, 16]. Meniscal allograft transplantation can also slow down the progression of osteoarthritis in the lateral compartment [17]. Lateral meniscus allograft transplant allows 75–85% return to sports with acceptable outcomes in adolescents with 67% returning to pre-injury levels of sports competition [18-20]. We have added our patient to the meniscus transplant list with the intention to operate on him once he nears skeletal maturity. Until then, he will be asked to avoid all contact and impact sports. The patient may have a similar picture in the contralateral knee. However, since he was asymptomatic and the malformation was not expected, we did not yet get the imaging or arthroscopy done for the opposite knee.
Our case is the youngest and only the second patient of PSLM reported in the literature, which presents a clinical challenge for diagnosis and treatment. It indicates that the pathophysiology may be more congenital than environmental. Further, genetic and fetal studies are needed in this area to determine the exact causality.
Surgeons need to be familiar with this condition while encountering an irreducible non-discoid lateral meniscus as the prognosis remains guarded with limited management options.
References
- 1.Haider Z, Syed MA, Saran D. Atraumatic sequential bilateral locking of the knee joints secondary to dislocation of non-discoid lateral menisci without radiological abnormality. J Clin Orthop Trauma 2017;8:S26-8. [Google Scholar]
- 2.Dykes HW Jr., Tytko J. A locked knee in an adolescent boy: Resolving meniscal pathology in young athletes. Phys Sportsmed 2004;32:43-7. [Google Scholar]
- 3.George M, Wall EJ. Locked knee caused by meniscal subluxation: Magnetic resonance imaging and arthroscopic verification. Arthroscopy 2003;19:885-8. [Google Scholar]
- 4.Van Steyn MO, Mariscalco MW, Pedroza AD, Smerek J, Kaeding CC, Flanigan DC. The hypermobile lateral meniscus: A retrospective review of presentation, imaging, treatment, and results. Knee Surg Sports Traumatol Arthrosc 2016;24:1555-9. [Google Scholar]
- 5.Kamiya T, Suzuki T, Otsubo H, Kuroda M, Matsumura T, Kubota C, et al. Midterm outcomes after arthroscopic surgery for hypermobile lateral meniscus in adults: Restriction of paradoxical motion. J Orthop Sci 2018;23:1000-4. [Google Scholar]
- 6.Kimura M, Shirakura K, Hasegawa A, Kobayashi Y, Udagawa E. Anatomy and pathophysiology of the popliteal tendon area in the lateral meniscus: 2. Clinical investigation. Arthroscopy 1992;8:424-7. [Google Scholar]
- 7.Nakashima H, Takahara Y, Uchida Y, Kato H, Itani S, Tsujimura Y, et al. Hypermobile anterior horn of the lateral meniscus: A case report and literature review. Case Rep Orthop 2020;2020:8870156. [Google Scholar]
- 8.Suganuma J, Ohkoshi T. Association of internal rotation of the knee joint with recurrent subluxation of the lateral meniscus. Arthroscopy 2011;27:1071-8. [Google Scholar]
- 9.Suganuma J, Sugiki T, Inoue Y. A case of bilateral permanent subluxation of the lateral meniscus. Case Rep Orthop 2016;2016:5912841. [Google Scholar]
- 10.Garofalo R, Kombot C, Borens O, Djahangiri A, Mouhsine E. Locking knee caused by subluxation of the posterior horn of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2005;13:569-71. [Google Scholar]
- 11.Haramati N, Staron RB, Rubin S, Shreck EH, Feldman F, Kiernan H. The flipped meniscus sign. Skeletal Radiol 1993;22:273-7. [Google Scholar]
- 12.Katz K, Mashiach R, Bar On A, Merlob P, Soudry M, Meizner I. Normal range of fetal knee movements. J Pediatr Orthop 1999;19:739-41. [Google Scholar]
- 13.Ahn JH, Lee SH, Kim KI, Nam J. Arthroscopic meniscus repair for recurrent subluxation of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2018;26:787-92. [Google Scholar]
- 14.Suganuma J, Inoue Y, Tani H, Sugiki T, Sassa T, Shibata R. Reconstruction of the popliteomeniscal fascicles for treatment of recurrent subluxation of the lateral meniscus. Arthrosc Tech 2017;6:e283-90. [Google Scholar]
- 15.Chatain F, Adeleine P, Chambat P, Neyret P, Société Française d’Arthroscopie. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy 2003;19:842-9. [Google Scholar]
- 16.Peña E, Calvo B, Martinez MA, Palanca D, Doblaré M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res 2006;24:1001-10. [Google Scholar]
- 17.Lee BS, Bin SI, Kim JM. Articular cartilage degenerates after subtotal/total lateral meniscectomy but radiographic arthrosis progression is reduced after meniscal transplantation. Am J Sports Med 2016;44:159-65. [Google Scholar]
- 18.Samitier G, Alentorn-Geli E, Taylor DC, Rill B, Lock T, Moutzouros V, et al. Meniscal allograft transplantation. Part 2: Systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2015;23:323-33. [Google Scholar]
- 19.Kocher MS, Tepolt FA, Vavken P. Meniscus transplantation in skeletally immature patients. J Pediatr Orthop B 2016;25:343-8. [Google Scholar]
- 20.Grassi A, Bailey JR, Filardo G, Samuelsson K, Zaffagnini S, Amendola A. Return to sport activity after meniscal allograft transplantation: At What level and at what cost? A systematic review and meta-analysis. Sports Health 2019;11:123-33. [Google Scholar]









