The management of a rare dislocation in children.
Dr. Amine El Khassoui, Department Pediatric Orthopedic, Mother and Child Unit, University Hospital Mohamed VI of Marrakech, Faculty of Medecine and Pharmacy, Cadi Ayyad University, 40000 Marrakech, Morocco. E-mail: a.elkhassoui@uca.ma
Introduction: Sternoclavicular dislocation (SCD) occurs very rarely in children. There is different clinical manifestations that reflect the direction of displacement; diagnosis is difficult, especially if the dislocation was initially unnoticed. We will report this case while conducting a review of the literature to evaluate and adapt our management.
Case Report: We report the case of a 12-year-old boy who presented with a right posterior SCD after a trauma occurring 24 h earlier at a sports activity. Clinical examination and radiological investigations by X-ray and computed tomography scan leads to diagnosis. He underwent an orthopedic closed reduction treatment without complications at 24 months of follow-up.
Conclusion: Management of posterior sternoclavicular dislocation is different between teams, with a tendency to use orthopedic reduction in case of fresh dislocation and absence of complications. Late diagnosis and management, as well as the presence of complications, may be difficult and life-threatening (due to vascular or tracheal compression).
Keywords: Sternoclavicular dislocation, posterior displacement, child, sports, orthopedic treatment.
Sternoclavicular dislocation (SCD) is a rare dislocation, representing <1% of all dislocations in men and 3% of dislocations in the shoulder region [1, 2], rarer if it is posterior, which represents 3–5% of dislocations of the sternoclavicular joint [3, 4]. Described for the 1st time by Rodrigues in 1843 [5], it is associated with a high rate of complications compared with anterior dislocation [2]. We report the case of a 12-year-old boy who presented with a right posterior SCD while conducting a review of the literature to evaluate and adapt our management.
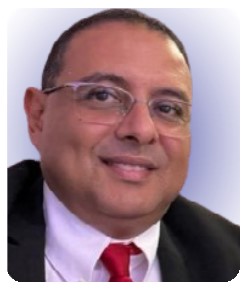
It was a closed trauma of the right hemithorax by a direct mechanism in a 12-year-old boy, occurring 24 h before admission, following a sports accident (kickboxing), with a fall of another boy directly on the right clavicle (the fulcrum was the knee on the clavicle). On examination: The child was conscious, hemodynamically, and respiratory stable, with a trauma attitude of the right upper limb (Fig. 1a). 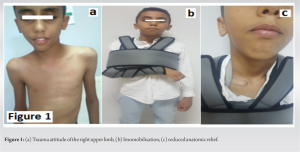
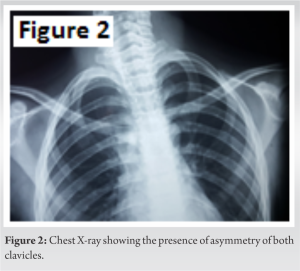
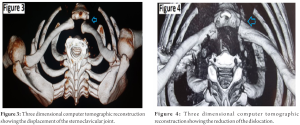
Posterior dislocation of the sternoclavicular junction is most often secondary to high-energy trauma (sports accidents, fall from height, traffic accident [2], but can also occur following low-energy trauma [6]. Non-traumatic dislocations are rare, occurring most often in patients with generalized hyperlaxity [3]. The mechanism is frequently direct with the medial border of the clavicle as the point of impact [1]. The symptomatology differs according to the side and direction of the dislocation [2]. Thus, in typical forms, we can find exquisite pain with limitation of shoulder movements without other associated lesions [1], or less obvious manifestations [2], such as a neurological or vascular deficit, brachial plexopathy, thoracic outlet syndrome, hoarseness, shortness of breath, dysphagia, respiratory distress due to tracheal compression, pneumothorax, esotracheal fistula, or shock [2, 5]. This clinical variability is responsible for the high rate of SCD that can be unnoticed in the emergency room [2]. The first-line examination is the standard frontal comparative chest radiograph, with specific incidences that can guide the diagnosis; the most used being the Heining radiograph [5]. It is most often inconclusive [5, 7], but may show indirect signs of dislocation or its complications, such as mediastinal enlargement, pneumothorax, hemothorax, or tracheal deviation [5]. CT scan, which has become a routine examination, allows both diagnosis and screening for complications with a 3D reconstruction that grants better visibility, contributing to the planning of the surgical procedure [2]. Some authors avoid the systematic use of CT because of the radiation involved, and it should only be indicated in the case of clinical manifestations that show the presence of associated lesions. The combination of standard radiography and ultrasound remains the recommended means of diagnosis [2]. We opted for cervicothoracic CT as a diagnostic tool in addition to standard radiography because emergency ultrasound is an operator-dependent examination; it requires an experienced radiologist to make the diagnosis and search for complications, which is not always possible. Our patient had a posterior sterno-clavicular dislocation with no clinical signs of complications, whereas the CT scan showed discreet compression of the innominate trunk. This discrepancy between the clinical signs and the severity of the associated lesions found suggests that CT remains the examination of choice in cases of a very suspicious SCD, as described in the literature [3]. According to some authors, the definite assertion that it is a posterior dislocation and not aclavicle medial extremity fracture with posterior displacement is very difficult despite a diagnosis made by CT scan, and only open reduction can confirm the diagnosis [3]. According to Gil-Albarova et al. [2], the stability of the closed reduction is an argument in favor of a true SCD, because it is more stable than in the case of a reduced clavicular fracture. Furthermore, a late control CT scan allows to differentiate between the two diagnoses by demonstrating the ossification of the fracture line. The therapeutic approach depends on the type of dislocation, the time of diagnosis, and the presence or absence of complications. Most teams propose closed reduction in case of recent trauma within 48 h [4], although some series report the success of closed reduction for dislocations of 10 days [4]. Open reduction should be proposed in case of failure of the latter. Other teams recommend the surgical approach for any SCD [8], or in the presence of complications, especially in the case of compression of the retrosternal mediastinal structures or after an unstable reduction [5]. We believe that closed reduction is more likely possible if the dislocation is recent. The closed reduction technique described by most authors consists of placing the patient in the supine position, with a log between the two scapulae, manual traction exerted on the clavicle in an anterior direction by a sandbag or non-traumatic forceps, the shoulder in antepulsion, the arm in abduction and under continuous and progressive traction. Successful reduction is marked by an audible snap and the disappearance of the sternoclavicular on palpation [9], which may be masked by edema and hematoma. The post-reduction radiograph or CT scan will confirm the success of the procedure. Failure of orthopedic reduction requires open reduction, bearing in mind that small, especially anterior and chronic disjunctions without other associated lesions indicate that treatment should be withheld for good functional evolution thereafter [2]. In the case of open reduction, each team uses different means of fixation to obtain a stable joint reduction. These may be eight sutures with absorbable or non-absorbable sutures and tendon sutures [2], placement of an external fixator [8], grafting of the palmaris longus or tibialis anterior with the use of synthetic ligaments, resection of the medial part of the clavicle, especially in the case of esophageal compression [10] or when thoracic outlet syndrome is present [3]. All the authors have proscribed the use of metallic fixation of the sternoclavicular joint by means of pins because of the numerous cases of serious complications following the migration of kirschner wires [2]. Immobilization with a clavicular ring and a truss for 4–6 weeks, with passive movements of small amplitude, may be allowed from the 4th week [4]. The right combination of a thorough clinical examination and an appropriate radiological work-up allows for a better and less invasive therapeutic attitude.
SCD in children remains a rare entity, and its diagnosis is often difficult. The clinical findings are heterogeneous, and its manifestations depend on the direction of the dislocation. Standard radiography and ultrasound have a good sensitivity but remain operator-dependent, so that is why cervicothoracic CT scan remains the preferred method for confirmation and screening of complications, despite the risk of radiation. Orthopedic closed reduction is usually successful and it depends on the precocity of the diagnosis.
We must think of sternoclavicular dislocation in front of a trauma localized in the medial extremity of the clavicle to start early management and avoid open reduction.
References
- 1.Ngom G, Mohamed AS, El Housseine MO, Ndour O. Traumatic posterior sternoclavicular joint dislocation in a child: A case report. Pan Afr Med J 2014;19:386. [Google Scholar]
- 2.Gil-Albarova J, Rebollo-González S, Gómez-Palacio VE, Herrera A. Management of sternoclavicular dislocation in young children: Considerations about diagnosis and treatment of four cases. Musculoskelet Surg 2013;97:137-43. [Google Scholar]
- 3.Garg S, Alshameeri ZA, Wallace WA. Posterior sternoclavicular joint dislocation in a child: A case report with review of literature. J Shoulder Elbow Surg 2012;21:e11-6. [Google Scholar]
- 4.Honeycutt MW, Cox K, Michaeli D, Hulon B, Brewer J. Pediatric posterior sternoclavicular dislocation closed reduction and management. J Orthop Trauma 2021;35:S11-2. [Google Scholar]
- 5.M. Rousset, P. Moreel, S. Descamps, posterior sternoclavicular dislocation, Journal de Traumatologie du Sport 2010;27(1):14-19. [Google Scholar]
- 6.Doss A, Lang IM, Roberts I, Bell MJ, Smith TW. Posterior sternoclavicular joint dislocation in children-role of spiral computed tomography. Pediatr Emerg Care 2005;21:325-6. [Google Scholar]
- 7.Aretz S, Benz-Bohm G, Helling HJ, Herkenrath P, Roth B. Right sternoclavicular dislocation after traumatic delivery: A case report. J Pediatr Surg 1999;34:1872-3. [Google Scholar]
- 8.Lehnert M, Maier B, Jakob H, Maier M, Laurer H, Marzi I. Fracture and retrosternal dislocation of the medial clavicle in a 12-year-old child.-case report, options for diagnosis and treatment in children. J Pediatr Surg 2005;40:e1-3. [Google Scholar]
- 9.Gove N, Ebraheim NA, Glass E. Posterior sternoclavicular dislocations: A review of management and complications. Am J Orthop (Belle Mead NJ) 2006;35:132-6. [Google Scholar]
- 10.Salvatore JE. Sternoclavicular joint dislocation. Clin Orthop Relat Res 1968;58:51-5. [Google Scholar]