Accurate diagnosis and grading of SLAC can be achieved with radiographic analysis alone, enabling early identification and successful treatment without the need for surgery in some cases.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: Scapholunate advanced collapse is a rare condition of progressive deformity, instability, and arthritis that affects the radiocarpal and mid-carpal joints of the wrist. It occurs as a result of injury to the scapholunate ligament being left untreated.
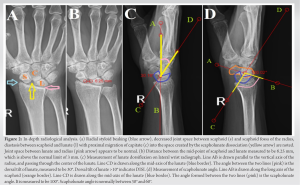
Case Report: We present the imaging of a 50-year-old woman who complained of pain in her right wrist for 2 years. Radiographs of the wrist revealed scapholunate diastasis (Terry Thomas Sign), arthritis of the radio-scaphoid joint, dorsal intercalated segment instability, radial styloid beaking, and proximal migration of capitate. We also demonstrate the measurement of radiological parameters such as scapholunate angle.
Conclusion: A complete in-depth radiological analysis can thus demonstrate several signs that can prevent missed diagnosis. Increased awareness regarding these radiological signs can avoid the unnecessary higher imaging modalities being performed.
Keywords: Scapholunate, collapse, wrist, radio-scaphoid joint.
Scapholunate advanced collapse (SLAC) is a term used to describe a degenerative wrist condition that exhibits progressive instability, deformity, and arthritis. This condition affects both the radiocarpal and mid-carpal joints in the wrist [1]. More specifically, the distinctive arthritic deformity and gradual loss of stability are the result of a prolonged and chronic separation between the lunate and scaphoid carpal bones [2]. SLAC wrist typically represents the final and most advanced stage that arises when a scapholunate ligament injury remains untreated [3, 4]. Epidemiological studies have shown that patients with SLAC wrist were more likely to be male, have a history of a traumatic injury, and be in the early fifth decade of life at the time of diagnosis [3, 5]. The diagnosis of SLAC is often missed or inaccurately diagnosed as general wrist arthritis [6,7]. We describe a case of SLAC wrist that demonstrates the identification and grading of SLAC enabling pertinent treatment.
A 50-year-old woman complained of pain in her right wrist for 2 years. The pain was dull aching and aggravated on lifting objects with her right hand. She had a history of falls on her outstretched right hand 4 years earlier. She had no pain in other joints. She had no other pre-existing medical conditions and was right-hand dominant. On examination, tenderness was present over the dorsal aspect of the radial half of the wrist. Range of movements of the wrist was limited with palmar flexion of 50°, dorsiflexion of 40°, ulnar deviation of 30°, and radial deviation of only 10°. Watson’s scaphoid shift test was positive. Her grip strength was found to be 8 kg less than the contralateral side. Her blood parameters including rheumatoid profile were found to be within normal limits. Radiographs of the wrist revealed scapholunate diastasis, arthritis of radio-scaphoid joint (Fig. 1a), and dorsal intercalated segment instability (DISI) (Fig. 1b).
SLAC is a wrist condition characterized by progressive instability, deformity, and arthritis due to chronic separation between the lunate and scaphoid carpal bones. SLAC is often misdiagnosed [9]. Early and accurate diagnosis of SLAC is crucial to prevent worsening symptoms, preserve wrist function, and reduce the need for invasive treatments. SLAC can be diagnosed with simple radiographs of the wrist but is commonly misdiagnosed as general wrist arthritis or scaphoid non-union advanced collapse (SNAC) [10]. Not all wrist osteoarthritis represents SLAC patterns; in fact, less than half of wrist osteoarthritis fall into the category of SLAC arthritis [11]. SLAC and SNAC can also be differentiated without requiring a magnetic resonance imaging (MRI). SLAC involves both radiocarpal and mid-carpal joints with a widened scapholunate gap, while SNAC primarily affects the radioscaphoid joint with a widened scapholunate gap but maintains a relatively normal radiocarpal joint space [12]. Our case report demonstrates that a careful radiological analysis can thus be sufficient to diagnose SLAC. Although MRI does make diagnosis easier [13], other studies have shown the reliability of diagnosis of SLAC based on radiographs alone [14, 15]. There are several treatment options for SLAC with no clear consensus on the most appropriate treatment algorithm [16]. Conservative treatment options include non-steroidal anti-inflammatory medications and splinting. Less invasive treatment options such as corticosteroid injections or injections of amniotic membrane and umbilical cord particulate have also been explored [17, 18]. Four-corner arthrodesis and proximal row carpectomy are the most commonly done surgical techniques for the management of SLAC [19]. Newer individualized options, such as osteochondral grafting in combination with proximal row carpectomy, arthroscopic distal resection of the scaphoid [20], and arthroscopic interposition tendon arthroplasty have been introduced in recent times [21]. With the availability of so many treatment options, it becomes imperative that the surgeon uses a classification or grading system to guide the treatment. The Watson and Ballet classification system remains the most commonly used classification system for the SLAC wrist [22]. This radiographic classification of SLAC wrist has proven to have moderate reliability and reproducibility, thus alleviating the necessity of an MRI [14].
This case report demonstrates that the accurate diagnosis and grading of SLAC can be achieved with just clinical examination and radiographic analysis. If identified early, it can be managed successfully without the need for surgical procedures in some cases. This simple approach to the management of SLAC demonstrates that it can be effectively managed even by general orthopedicians if awareness about it is increased and is picked up early.
- SLAC occurs as a result of neglected scapholunate ligament injury
- Radiographs show radial beaking, decreased radio-scaphoid joint space, scapholunate diastasis, and DISI deformity, while the radiolunate joint is typically spared
- Identification of the signs on radiographs eliminates the need for higher imaging modalities.
References
- 1.Lane R, Tafti D, Varacallo M. Scapholunate advanced collapse. In: StatPearls. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537124 [Last accessed on 2023 Sep 18]. [Google Scholar]
- 2.Pomeranz SJ, Salazar P. Scapholunate advanced collapse. J Surg Orthop Adv 2015;24:140-3. [Google Scholar]
- 3.Ault DL, Mann DJ, Troutner AM, Kettner NW. Post-traumatic scapholunate advanced collapse of the wrist: A case report. J Chiropr Med 2018;17:128-34. [Google Scholar]
- 4.Pai SN, Kumar MM. Isolated lunate dislocation. BMJ Case Rep 2022;15:e248917. [Google Scholar]
- 5.Murphy BD, Nagarajan M, Novak CB, Roy M, McCabe SJ. The epidemiology of scapholunate advanced collapse. Hand (N Y) 2020;15:23-6. [Google Scholar]
- 6.Laulan J, Marteau E, Bacle G. Wrist osteoarthritis. Orthop Traumatol Surg Res 2015;101:S1-9. [Google Scholar]
- 7.Wessel LE, Wolfe SW. Scapholunate instability: Current concepts in diagnosis and management classification and treatment considerations-part 2. J Hand Surg Am 2023;S0363-5023(23)00329-5. [Google Scholar]
- 8.Watson HK, Ballet FL. The SLAC wrist: Scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am 1984;9:358-65. [Google Scholar]
- 9.Tischler BT, Diaz LE, Murakami AM, Roemer FW, Goud AR, Arndt WF 3rd, et al. Scapholunate advanced collapse: A pictorial review. Insights Imaging 2014;5:407-17. [Google Scholar]
- 10.Trehan SK, Lee SK, Wolfe SW. Scapholunate advanced collapse: Nomenclature and differential diagnosis. J Hand Surg Am 2015;40:2085-9. [Google Scholar]
- 11.Miller A, Lutsky KF, Shearin J, Cantlon M, Wolfe S, Beredjiklian PK. Radiographic patterns of radiocarpal and midcarpal arthritis. J Am Acad Orthop Surg Glob Res Rev 2017;1:e017. [Google Scholar]
- 12.Kompoliti E, Prodromou M, Karantanas AH. SLAC and SNAC wrist: The top five things that general radiologists need to know. Tomography 2021;7:488-503. [Google Scholar]
- 13.Li AE, Lee SK, Rancy SK, Burge AJ, Potter HG, Wolfe SW. Comparison of magnetic resonance imaging and radiographs for evaluation of carpal osteoarthritis. J Wrist Surg 2017;6:120-5. [Google Scholar]
- 14.Vishwanathan K, Hearnden A, Talwalkar S, Hayton M, Murali SR, Trail IA. Reproducibility of radiographic classification of scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist. J Hand Surg Eur Vol 2013;38:780-7. [Google Scholar]
- 15.Shah CM, Stern PJ. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med 2013;6:9-17. [Google Scholar]
- 16.Strauch RJ. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis-update on evaluation and treatment. J Hand Surg Am 2011;36:729-35. [Google Scholar]
- 17.Kim SR. Successful treatment of scapholunate advanced collapse: A case report. Clin Case Rep 2019;7:1230-2. [Google Scholar]
- 18.Kiefhaber TR. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg Am 2009;34:1527-30. [Google Scholar]
- 19.Kruse K, Fowler JR. Scapholunate advanced collapse: Motion-sparing reconstructive options. Orthop Clin North Am 2016;47:227-33. [Google Scholar]
- 20.Zhang Y, Gillis JA, Moran SL. Management of scapholunate advanced collapse and scaphoid nonunion advanced collapse without proximal row carpectomy or four corner fusion. J Hand Surg Eur Vol 2021;46:50-7. [Google Scholar]
- 21.De Villeneuve Bargemon JB, Merlini L, Mathoulin C, Levadoux M. Arthroscopic radiocarpal tendinous inter-position for grade 2 scapholunate advanced collapse - surgical technique. J Hand Surg Asian Pac Vol 2022;27:889-94. [Google Scholar]
- 22.McLean A, Taylor F. Classifications in brief: Watson and ballet classification of scapholunate advanced collapse wrist arthritis. Clin Orthop Relat Res 2019;477:663-6. [Google Scholar]