This case report is about an unusual anatomical variation of the peroneal artery which was diagnosed preoperatively on angiography and confirmed intraoperatively during free fibula harvest.
Dr Mantu Jain, J-102, Cosmopolis, Dumduma, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Vascularized free fibula flap is one of the commonly used flaps in autologous soft-tissue and osseous reconstructions in the modern era. While there is abundant literature available on the variable branching pattern and course of the popliteal artery, tibial arteries, and dorsalis pedis artery, there is a paucity of text available on the not-so-common peroneal vessels.
Case Report: A case of a 60-year-old male who was diagnosed with carcinoma of buccal mucosa with involvement of the mandible of the right side was planned for wide local excision with modified radical neck dissection and resurfacing of the resultant defect using a contralateral free fibula osseocutaneous free flap. Intraoperatively, the peroneal vessels were noted to have a premature termination along the lateral border of distal one-third of the fibula, after giving a communicating branch to an anterior tibial artery. The flap was raised based on the same pedicle, without ligating any distal portion of the vessel. Reconstruction of the defect and post-operative recovery was uneventful. Full flap survival was observed.
Conclusion: We report this case as this vascular “anomaly” is one of its kind and has been oblivious to the literature and practicing microsurgeons globally.
Keywords: Osseocutaneous free flap, peroneal vessel anomaly, reconstruction.
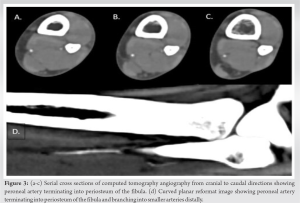
Vessels of the lower leg are oriented predominantly along the longitudinal axis of the limb. There are three main arteries of the lower leg – anterior tibial, posterior tibial, and peroneal arteries – which give off multiple branches to the bone, muscles, and the overlying skin in the form of numerous perforators (septocutaneous and musculocutaneous). The peroneal artery arises from the tibioperoneal trunk approximately 2.5 cm below the lower edge of the popliteus muscle. It runs laterally along the medial crest of the fibula, sends a nutrient artery to the fibula at its mid-point, and sends a communicating branch to the posterior tibial artery almost 6.5 cm above the lateral malleolus. The artery terminates by giving off calcaneal branches and forming the anastomosis around it. This conventional anatomy of lower leg vasculature has been well documented in the textbook “The Arterial Anatomy of Skin Flaps” by Cormack and Lamberty and is encountered 90% of the time while harvesting a free fibula flap [1]. However, in the remaining 10 % of the population, there might be variations existing in any of the above vasculatures as shown in Fig. 1 [1]. Apart from the above-mentioned variations, we present a case of a vascular anomaly in peroneal vessels during free fibula flap harvest, which, to the best of our knowledge, is one of its kinds and has not been reported in the literature. The aim was to make the surgeons aware of this variation that may be relevant to diagnostic evaluation, as well as minimizing complications during surgical procedures.
A 62-year-old male presented with complaints of a lesion in the right buccal mucosa present for 1.5 years with rapid progression in the past 3 months. The patient underwent an incisional biopsy for the same, which showed well-differentiated squamous cell carcinoma.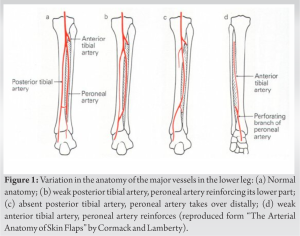
Anatomical landmarks
A line was drawn between fibula head and lateral malleolus to mark the posterior intramuscular septum. Six centimeters of the fibula were spared above and below to maintain the stability of the knee and ankle joints. Perforators were marked preoperatively with a handheld Doppler along the posterior border of the fibula. The skin paddle was designed in the middle third of the fibula (Fig. 4).
Dissection
Anterior exploratory incision was given and the lateral compartment was exposed. Septocutaneous perforators to the skin paddle were identified and preserved. The deep fascia was incised along the perforators and peroneus longus and brevis muscles were identified and separated from the fibula, leaving a 2-mm cuff of muscle adjacent to the bone. Next, the anterior compartment muscles, the tibialis anterior, extensor digitorum longus, and extensor digitorum hallucis were identified and separated from the fibula and were retracted away. 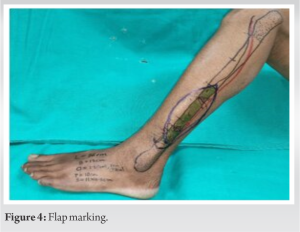
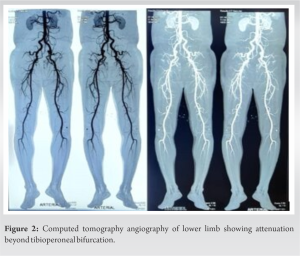
Arterial network of the lower limb is typically associated with the variations in femoral artery and its main branches [2, 3, 4]. The tibial arteries are shown to be particularly susceptible to congenital variations compared with the peroneal vessels [5]. Most variation results from non-standard arterial division, aplasia, or hypoplasia. However, these variations are extremely rare for the peroneal artery [6]. Although these anomalies may still be encountered by reconstructive surgeons, radiologists, and other lower limb surgeons, if one is vigilant. While a dominant peroneal artery (estimated prevalence – 0.4 %) precludes a free fibula flap harvest in view of significant limb ischemia, an aplastic peroneal artery is an absolute contraindication as it leads to an unusable flap [7]. Congenital anatomic anomalies in which the peroneal artery provides a significant contribution to the blood flow of the foot can be found in up to 5% of lower limbs [6]. Hence, pre-operative imaging for vascular mapping becomes a pre-requisite before free fibula harvest not only to rule out peripheral arterial disease or other congenital anomalies but also it paves the way to decide on alternative methods of reconstruction such as composite radial or iliac crest flaps [8, 9 10]. Lippert and Pabst and later modified by Kim et al. classified anatomical variations of lower limb vasculature [11, 12]. This classification is being widely used to describe infrapopliteal arterial variations, of which Group III is of particular interest to microvascular surgeons for free fibula harvest, as it groups hypoplasia or aplasia of the tibial arteries with dominant peroneal supply to the foot. Our case report highlights one such variation of the peroneal artery, to enhance the existing knowledge regarding lower limb vascular anatomy. This knowledge is important for orthopedists regularly performing knee replacement surgeries, for microvascular surgeons and even for the radiologists performing transluminal stenting, angioplasties, embolectomies, and diagnostic angiographies.
Vascularized free fibula flap is a highly practiced flap in the world of plastic surgery for various soft-tissue reconstructions. It is imperative for the operating microsurgeon to understand the vascular anatomy and anticipate the possible variations that one might come across during dissection. The variable anatomy of the peroneal artery reported here will help in expanding one’s knowledge regarding the vascular anatomy of the lower limb and being mindful during the harvest of a free fibula flap.
Premature termination of the peroneal artery in the distal periosteum is a rarely encountered intraoperative finding during free fibula harvest despite showing a normal CT angiography arterial anatomy during perioperative evaluation.
References
- 1.Cormack GC, Lamberty BG. The Arterial Anatomy of Skin Flaps. London: Churchill Livingstone 1986. [Google Scholar]
- 2.Nasr AY, Badawoud MH, Al-Hayani AA, Hussein AM. Origin of profunda femoris artery and its circumflex femoral branches: Anatomical variations and clinical significance. Folia Morphol (Warsz) 2014;73:58-67. [Google Scholar]
- 3.Rajani SJ, Ravat MK, Rajani JK, Bhedi AN. Cadaveric study of profunda femoris Artery with some unique variations. J Clin Diagn Res 2015;9:AC01-3. [Google Scholar]
- 4.Tomaszewski KA, Henry BM, Vikse J, Roy J, Pękala PA, Svensen M, et al. The origin of the medial circumflex femoral artery: A meta-analysis and proposal of a new classification system. PeerJ 2016;4:e1726. [Google Scholar]
- 5.Voboril R. Note on variability of the arteries of the lower extremities in man. Folia Morphol (Praha) 1990;38:265-72. [Google Scholar]
- 6.Rahmel BB, Snow TM, Batstone MD. Fibular free flap with arteria peronea magna: The role of preoperative balloon occlusion. J Reconstr Microsurg 2011;27:169-72. [Google Scholar]
- 7.Abou-Foul AK, Borumandi F. Anatomical variants of lower limb vasculature and implications for free fibula flap: Systematic review and critical analysis. Microsurgery 2016;36:165-72. [Google Scholar]
- 8.Alolabi N, Augustine H, Farrokhyar F, Levis C. Preoperative angiography for free fibula flap harvest: A case series. Plast Surg (Oakv) 2022;30:108-12. [Google Scholar]
- 9.Ou Q, Wu P, Zhou Z, Pan D, Tang JY. Complication of osteo reconstruction by utilizing free vascularized fibular bone graft. BMC Surg 2020;20:216 [Google Scholar]
- 10.Ghassemi A, Jost M, Fitzner C, Jalaie H, Hölzle F, Apitzsch J, et al. Factors influencing the necessity for preoperative vascular imaging before harvesting a vascularized fibular flap. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:289-92. [Google Scholar]
- 11.Lippert H, Pabst R. Arterial Variations in Man: Classification and Frequency. Munchen: J.F. Bergmann Verlag; 1985. p. 62-3. [Google Scholar]
- 12.Kim D, Orron DE, Skillman JJ. Surgical significance of popliteal arterial variants. A unified angiographic classification. Ann Surg 1989;210:776-81. [Google Scholar]