The novel endoscopic visualization pedicle screw insertion technique and UBE-transforaminal lumbar interbody fusion technique have the advantages of minimally invasive spine surgery; they are a safe and effective treatment option for treating lumbar spine pathologies.
Dr. Rajendra Sakhrekar, Department of Spine Surgery, Yonsei Okay Hospital, Seoul, South Korea. E-mail: raj.sakhrekar1@gmail.com
Introduction: Over the past two decades, unilateral biportal endoscopy (UBE) has brought a new paradigm shift in the surgical treatment of spinal disorders with its innovative technique. This study aims to review the development of the UBE technique with a technical note on the novel endoscopic visualization pedicle screw (EVPS) insertion technique and UBE-transforaminal lumbar interbody fusion technique (UBE-TLIF).
Case Report: A 66-year-old female presented with severe back pain (Visual Analog Scale [VAS] 8/10) and radicular pain in both legs (left > right) (left VAS 7/10 and right VAS 7/10) for one year with an Oswestry disability index (ODI) score of 70%. Her pain aggravated when bending forward and performing daily routine activities. She also complained of severe intermittent neurological claudication at a distance of <50 m. On physical examination, power in the lower limbs was 5/5 as per the Medical Research Council grading, and deep tendon reflexes were normal. She had a known case of diabetes mellitus and hypertension and was on treatment with oral medications. Pre-operative X-ray and magnetic resonance imaging showed dynamic instability with spondylolisthesis at L4–5. We performed UBE-TLIF with the EVPS insertion technique to resolve her symptoms. The operative time was 122 min; blood loss was 40 mL. After surgery, the patient was followed up at one week, six weeks, three months, six months, 12 months, and two years. The pain and tingling sensation in the legs improved at the 1-week follow-up, with a VAS score of 0/10 and an ODI score of 10% at the 2-year follow-up. Patient satisfaction was surveyed using Macnab’s criteria at the final follow-up visit of 2 years and was found to be excellent. Post-operative imaging showed a good reduction and canal decompression at L4–5.
Conclusion: The novel EVPS insertion technique and UBE-TLIF have the advantages of minimally invasive spine surgery; they are a safe and effective treatment option for treating lumbar spine pathologies.
Keywords: Unilateral biportal endoscopy, Endoscopic visualization pedicle screw insertion technique, Visual Analog Scale score, Oswestry disability index score
Over the past two decades, unilateral biportal endoscopy (UBE) has brought a new paradigm shift in the surgical treatment of spinal disorders with its innovative technique. A UBE is a spinal endoscopy with two portals on the same (unilateral) side of the midline. One is used as the endoscopic portal, and the other is used as the working portal. The benefit of the unilateral approach is that the surgeon uses the same surgical route as in open surgery, and the benefit of biportal endoscopy is that the endoscope of the endoscopic portal and the instruments of the working portal move independently. The functionality of the independent movement of the devices in each portal enables the surgeons to eliminate visual and motion limitations. This study aims to review the development of the UBE technique with a technical note on the novel endoscopic visualization pedicle screw (EVPS) insertion technique and UBE-transforaminal lumbar interbody fusion technique (UBE-TLIF).
The past of UBE
In 1983, Kambin and Gellman, an American-Iranian orthopedic surgeon, and his group were the pioneers to begin to try to use arthroscopy to perform lumbar discectomy. They published their work, “Percutaneous lateral discectomy of the lumbar spine: A preliminary report” [1]. In 1989, Schreiber et al. [2] also used bilateral dual-channel arthroscopy for lumbar discectomy removal. In 1996, De Antoni et al. from Argentina [3] were the first to use double-channel endoscopic surgery through a unilateral approach for translaminar lumbar discectomy. In 2001, Dr. Abdul Gaffer from Bahrain presented their work on UBE technology at the American Academy of Orthopedic Surgeons Annual Meeting, which inspired Korean surgeons. Dr. Eum from South Korea learned UBE under Dr. Gaffar. Eum et al. brought the technique to South Korea and trained several colleagues on the UBE technology [4]. In 2013 and 2015, Dr. Soliman from Egypt improved the UBE technology and published their work on lumbar discectomy and lumbar spinal stenosis, respectively [5, 6]. Research works by De Antoni et al. [3], Gaffar et al., Soliman [5, 6], Eum et al. [4], Park et al. [7], Eum et al., Ahn et al. [4, 8], Kim and Choi [9], and Choi et al. [10] on UBE technology in the 2010s have led to the foundation of current advancements in UBE technology.
The present of UBE technology
At present, UBE is being used for various spine disorders, most commonly lumbar pathologies for discectomy, decompression, and lumbar fusion. The use of the UBE technique for cervical and thoracic pathologies such as protruded intervertebral discs, ossification of the posterior longitudinal ligament, hypertrophic ligamentum flavum, and foraminal stenosis is also common [7, 11]. Here, we discuss the UBE-TLIF technique with the novel EVPS insertion technique.
Technical note
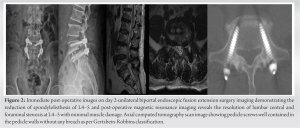
Careful pre-operative planning is essential with imaging modalities such as dynamic X-ray images to look for instability, and three-dimensional computed tomography and magnetic resonance imaging scans must be performed before surgery to plan pedicle screws and rods and understand the anatomy of neurological structures such as nerves, thecal sac, and soft tissues.
A 66-year-old female presented with severe back pain (Visual Analog Scale [VAS] 8/10) and radicular pain in both legs (left > right) (left VAS 7/10 and right VAS 7/10) for one year with an Oswestry disability index (ODI) score of 70%. Her pain aggravated when bending forward and performing daily routine activities. She also complained of severe intermittent neurological claudication at a distance of <50 m. On physical examination, power in the lower limbs was 5/5 as per the Medical Research Council grading, and deep tendon reflexes were normal. She had a known case of diabetes mellitus and hypertension and was on treatment with oral medications. Pre-operative X-ray and magnetic resonance imaging showed dynamic instability with spondylolisthesis at L4–5 (Fig. 1).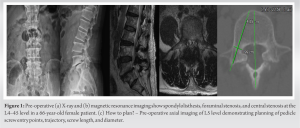
UBE-TLIF
The patient is positioned prone under general endotracheal anesthesia. However, surgeons can choose limited epidural anesthesia with sedation or their preferred choice of anesthesia.
Portal placement
The first step is to create the portals under C-arm fluoroscopy. The surgeon makes ipsilateral skin incisions vertically (author’s preferred choice) or transversely on the pedicles of the index level. In the case of left-sided approaches, the left cranial hole acts as the endoscopic viewing portal, and the right caudal hole serves as the working portal (Fig. 3). After making two small skin and fascia incisions, we insert serial dilators and dissectors to make two portals. After confirming bony feedback on the dorsal surface of the lamina, periosteal dissection is achieved gently after confirming the location using a C-arm fluoroscope. Finally, an endoscopic irrigation system is used, and the irrigation fluids are drained from viewing the endoscopic portal to the working portal. Irrigation water naturally forms a water chamber above the lamina; it helps control bleeding due to its hydrostatic pressure and provides clear surgical field visibility, creating space for endoscopic interbody fusion.
Unilateral laminectomy with facetectomy followed by bilateral decompression
We first perform a unilateral laminectomy with facetectomy and over-the-top/sublaminar decompression for bilateral decompression through a highly magnified endoscopic view. Authors prefer to use a high-speed burr to thin out and decorticate the outer cortex of the lamina at the inferior edge of the lamina until the insertion of the flavum ligament is seen and can be detached, followed by osteotome and chisel to resect the inferior articular process (IAP), the base of the spinous process, and the inner cortex of the contralateral lamina up to the contralateral facet joint to use the bony chunk as an autologous bone graft. In the cases of rigid listhesis, to get better release and reduction of the listhesis, contralateral facetectomies were performed with the same over-the-top approach. Foraminotomy is crucial for efficient discectomy, end-plate preparation, and adequate-size cage insertion. The IAP and the medial part, base, and tip of the superior articular process (SAP) are resected. Authors prefer the detachment of ligamentum flavum with the help of curettes and the Kerrison punch, followed by flavectomy piece-by-piece removal using the Kerrison punch; they feel that it is safer and more precise than total en bloc flavectomy. The flavectomy is continued medially under the spinous process, reaching the spinal canal’s contralateral side and foramen. Adequacy of complete decompression is confirmed with signs of a pulsating and free thecal sac, bilaterally traversing the nerve root and exiting the nerve root.
Discectomy, end-plate preparation, and cage insertion
The possible source of bleeding comes from the complex epidural veins, plexus, and adhesion around neurovascular structures. We use radiofrequency (RF) probes of various types, like 30°, 90°, and ball type, before cutting epidural veins to prevent blood loss. RF probes also help expose the disc, clearing adhesions of the dura to the disc. The authors prefer to retract and mobilize the traversing root and the thecal sac medially with the help of the sheath attached to the endoscope, which also acts as a nerve root retractor. Through the working portal, an annulotomy is performed, followed by a discectomy using a shaver, curettes, and pituitary forceps. The adequacy of endplate preparation is confirmed by direct visualization of the excision of endplate cartilage with the evidence of multiple spots of bleeding and gritty sound from the bone with the curettes (Fig. 4). Cage trials are done, and the appropriate size of the cage and tentative position are confirmed under fluoroscopy. Preferably, the insertion of the cage for the L4–5 level is done through the left side of the patient and from the right side for the L5–S1 level, considering the oblique angle or tilt of the L5–S1 level in relation to the perpendicular surface of the floor. Adjunct to the demineralized matrix as an allograft, an autologous bone graft harvested from IAP, SAP, lamina, and spinous process with the help of chisel, osteotome, and Kerrison punch is used. Over the cage glider, a lordotic cage with good width and height is inserted straight after dural retraction with a nerve root retractor under fluoroscopic guidance. We tap the cage to change its orientation, positioning it anteriorly and covering the entire brim of the endplate in width.
Novel endoscopic visualization technique for pedicle screw insertion
The screw entry point, trajectory, screw length, and diameter were planned pre-operatively using a pre-operative computed tomography (CT) scan, X-rays, and intraoperative fluoroscopy. After completing the unilateral biportal interbody fusion of the index level, anteroposterior and lateral X-rays were taken to confirm the vertebral level and the pedicle of interest (Fig. 5). 
The UBE approach necessitates appropriate coordination between both hands and steady instrument operation with a single hand through the working portal. Both hands are required to operate simultaneously, and the authors preferred to handle the lens in the non-dominant left hand and surgical tools in the right dominant hand. Spinal surgeons need to familiarize themselves with the arthroscopic tools, synchronize their perception of the depth and direction of the lens, move the instruments swiftly and smoothly in and out of the instrument channel, and quickly acquire the field of view in the early phase of the procedure during their learning curve. UBE-TLIF has several advantages, including minimizing extensive muscle dissection, less blood loss, less post-operative pain, and faster recovery from the surgery [8, 12]. The UBE-TLIF is a versatile approach with good vision, which provides a feasible advantage of reducing muscle damage, blood loss, complications, length of stay, early post-operative recovery, and return to work [13-16]. The endoscopic fusion technique is performed using 1.5-mm portals; as mentioned earlier, the working portal for the instruments and viewing portal for the endoscope is separate, which helps in the surgical instrument’s handling, making it more convenient than uniportal surgery. Moreover, it is worth recalling that there is no surgical range limitation because of the unfettered accessibility of the endoscope. In addition, endoscopic surgery does not simply mean surgery with small skin incisions and wounds. There is no massive bleeding because there is minimal muscle damage. Furthermore, it is widely known that endoscopic surgery is a water-medium technique with an endoscopic lens view of the operative field more specified, showing vital structures at 40–50 times magnification. Continuous real-time irrigation wash out naturally forms a water chamber, which helps control bleeding due to hydrostatic pressure and provides clear surgical field visibility. Consequently, clear and high-ratio viewing causes more precise operations, enabling safer surgery. Furthermore, dural tears and cerebral spinal fluid leakage from the previous laminectomy and the risks of infection are very low as the muscle dissection with UBE is minimal. Fundamentally, UBE fusion surgery has all the advantages of the posterior approach, such as wide laminectomy or targeted minimal laminectomy; bilateral facetectomies are entirely available through the posterior process compared with the minimally invasive technique with an anterior, lateral, or oblique approach. As the working portal is used only as the entrance for the spinal instruments, various conventional surgical instruments and endoscopic devices are available. Furthermore, the posterior approach in the case of a traditional extension of fusion surgery has the apparent burden of revision on the previous operative area. The cost-effectiveness of this technique can be demonstrated by enabling faster post-operative recovery and an early return to work or social life. In addition, implementing UBE technology does not require the purchase of special lenses and instruments, as seen in the percutaneous transforaminal endoscopic technique. UBE can use general arthroscopic lenses and open spinal surgical instruments, which is more conducive to wide acceptance in most hospitals. There were supplemental benefits, no need for transfusion due to low bleeding during surgery, and a lesser chance of infection. In addition, the other benefits of this approach include enhanced recovery after surgery, even in severely comorbid patients, as it is one of the most minimally invasive endoscopic approaches with minimal post-operative morbidity compared to conventional open surgery. UBE surgery has various advantages over microtubular retractor surgery as UBE is a water-based surgery: The hydrostatic pressure helps to reduce bleeding, constant irrigation helps to separate soft tissue layers such as a thecal sac and ligamentum flavum, the irrigation effect also reduces the risk of infection, and the endoscope can go into the canal; thus, a clear or magnified view can help to see and differentiate anatomical structures in more detail. With tubular retractors, the vision is limited, and the range of motion of surgical instruments is restricted and limited to the tube. The disadvantages of the UBE over the tubular retractor include the learning curve associated with the new technique and the risk of water accumulation leading to intracranial pressure elevation, dural irritation, or seizure induction.
Limitations and future directives
However, there are some limitations to the UBE technique. Large prospective randomized multicenter cohort studies with long-term data are still lacking for the UBE technique. Furthermore, the role of the UBE technique for intradural pathologies, high-grade listhesis, benign tumours, infective pathologies, adult degenerative scoliosis, and pediatric deformities is yet to be established. In the case of a significant dural leak, the surgeon might have to convert UBE surgery to open surgery to repair it effectively. However, for future directives, to overcome the above, the authors suggest the use of an HR*[HaRaj] (Fig. 6) arm attached to the operating table to stabilize and have a firm hold of the endoscope to carry out practical intradural work and to improvise surgical time using both hands for working. At that point, the UBE technique can be used in the future with extended indications such as adult spine deformity, pediatric spine deformity, high-grade listhesis, benign intradural tumours, and benign spine tumour pathologies.
The unilateral biportal endoscopic has brought a paradigm shift in the treatment of spinal pathologies and has served as another treatment option for the past two decades. The novel EVPS insertion technique and UBE-TLIF have the advantages of minimally invasive spine surgery; it is a safe and effective treatment option for treating lumbar spine pathologies.
The novel EVPS insertion technique and UBE-TLIF have the advantages of minimally invasive spine surgery; they are a safe and effective treatment option for treating lumbar spine pathologies.
References
- 1.Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine: A preliminary report. Clin Orthop Relat Res 1983;174:127-32. [Google Scholar]
- 2.Schreiber A, Suezawa Y, Leu H. Does percutaneous nucleotomy with discoscopy replace conventional discectomy? Eight years of experience and results in the treatment of herniated lumbar disc. Clin Orthop Relat Res 1989;238:35-42. [Google Scholar]
- 3.De Antoni DJ, Claro ML, Poehling GG, Hughes SS. Translaminar lumbar epidural endoscopy: Anatomy, technique, and indications. Arthroscopy 1996;12:330-4. [Google Scholar]
- 4.Eum JH, Heo DH, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: A technical note and preliminary clinical results. J Neurosurg Spine 2016;24:602-7. [Google Scholar]
- 5.Soliman HM. Irrigation endoscopic discectomy: A novel percutaneous approach for lumbar disc prolapse. Eur Spine J 2013;22:1037-44. [Google Scholar]
- 6.Soliman HM. Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J 2015;15:2282-9. [Google Scholar]
- 7.Park JH, Jun SG, Jung JT, Lee SJ. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics 2017;40:e779-83. [Google Scholar]
- 8.Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: A comprehensive review. Expert Rev Med Devices 2019;16:373-80. [Google Scholar]
- 9.Kim JE, Choi DJ. Bi-portal arthroscopic spinal surgery (BASS) with 30° arthroscopy for the far lateral approach of L5-S1-technical note. J Orthop 2018;15:354-8. [Google Scholar]
- 10.Choi CM, Chung JT, Lee SJ, Choi DJ. How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir (Wien) 2016;158:459-63. [Google Scholar]
- 11.Zhu C, Zhou X, Ge G, Wang C, Zhuang X, Cheng W, et al. Unilateral biportal endoscopic laminectomy for treating cervical stenosis: A technical note and preliminary results. Medicina (B Aires) 2023;59:305. [Google Scholar]
- 12.Heo DH, Park CK. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg Focus 2019;46:E18. [Google Scholar]
- 13.Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: Technical note and preliminary clinical results. Neurosurg Focus 2017;43:E8. [Google Scholar]
- 14.Heo DH, Lee DC, Kim HS, Park CK, Chung H. Clinical results and complications of endoscopic lumbar interbody fusion for lumbar degenerative disease: A meta-analysis. World Neurosurg 2021;145:396-404. [Google Scholar]
- 15.Heo DH, Hong YH, Lee DC, Chung HJ, Park CK. Technique of biportal endoscopic transforaminal lumbar interbody fusion. Neurospine 2020;17:S129-37. [Google Scholar]
- 16.Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev 2019;42:753-61. [Google Scholar]