THA with dual mobility cup (DMC) is a promising solution for ochronotic arthropathy, as it enhances joint stability, mobility, and durability, and reduces implant failure and dislocation risk.
Dr. Sujoy Bhattacharjee, Department of Orthopaedics, Robotic Joint Replacement Unit, Sarvodaya Hospital Research Centre Sector 8, Sarvodaya Hospital Sector 19, Faridabad, Haryana, India. E-mail: propesi2020@gmail.com
Introduction: Total hip arthroplasty (THA) is a common procedure used to treat various hip conditions. However, patients with ochronotic arthropathy, a rare genetic disorder characterized by the abnormal accumulation of homogentisic acid, are at a higher risk of post-surgical dislocation and instability due to poor bone quality and joint degeneration.
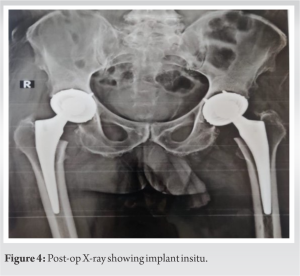
Case Report: This case study features a 52-year-old male patient diagnosed with ochronotic arthropathy who underwent bilateral THA with the use of a dual mobility cup (DMC). Ochronotic arthropathy had caused significant joint degeneration and stiffness, leading to considerable functional impairment.
Conclusion: The application of a DMC in THA for patients with ochronotic arthropathy has shown promising outcomes. The DMC offers increased range of motion and improved stability, effectively reducing the risk of post-surgical dislocation and implant failure. This case study highlights the potential of DMC as a viable solution for addressing the challenges posed by poor bone quality in patients with ochronotic arthropathy undergoing THA.
Keywords: Total hip arthroplasty, ochronotic arthropathy, dislocation, dual mobility cup, range of motion.
Total hip arthroplasty (THA) is widely acknowledged as a highly successful surgical procedure that effectively alleviates pain and enhances the functional capacity of patients who suffer from end-stage hip arthritis that has not responded to non-operative treatments [1]. Ochronotic arthropathy is a rare musculoskeletal condition associated with alkaptonuria, which is a rare genetic disorder caused by a deficiency of the enzyme homogentisate 1,2-dioxygenase [2]. This enzyme is responsible for the breakdown of aromatic amino acids, including tyrosine and phenylalanine, resulting in the accumulation of homogentisic acid in the body, lending the development of ochronotic arthropathy [3]. Ochronotic arthropathy is inherited in an autosomal recessive pattern, and its prevalence ranges from 1 in 1,000,000 to 1 in 250,000 [4]. The pathogenesis of ochronotic arthropathy is due to the abnormal accumulation of homogentisic acid, which is a strong reducing agent that converts to a dark pigment upon oxidation [5]. This pigment deposits in the cartilage, tendons, ligaments, capsule, and articular cartilage of peripheral joints, leading to loss of elasticity and poor resistance to mechanical strain [6]. Ochronotic arthropathy is typically asymptomatic until the third or fourth decade of life, and symptoms include low back pain, stiffness, and degenerative arthritis of the knee, hip, and shoulder [7]. Treatment options for ochronotic arthropathy are limited, and THA poses unique challenges due to the deposition of homogentisic acid in connective tissues, resulting in joint degeneration and stiffness [8]. However, the dual mobility cup (DMC) has emerged as a promising solution for THA in ochronotic arthropathy, providing increased range of motion (ROM) and stability to help reduce the risk of dislocation and implant failure [9].
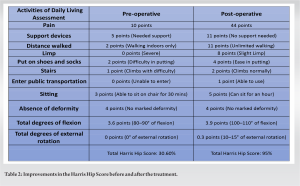
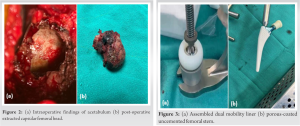
A 52-year-old male patient reported to the department of joint replacement Sarvodaya Hospital, a tertiary care hospital. He presented with chief complaints of stiffness in the back and bilateral painful hip joints, causing a limp. The pain was dull aching in nature, non-radiating, and localized to the hip region. The patient gave a positive medical history of similar pain for the past 2 years, which had flared up in the past 4 months, to the extent that he failed to perform daily activities. The patient also complained that his urine would turn brown on standing for some time after voiding. Later, the urine analysis showed the presence of HGA with an elevation factor of 2637.00, which is suggestive of Alkaptonuria. The family history of similar complaints was negative. However, the stiffness of the back was medically intervened through regular physiotherapy and was alleviated. On physical examination, stiffness of the spine was tested with SCHOBERS, which was negative (test to determine if there is a decrease in lumbar spine ROM due to any chronic condition). Fixed flexion deformities were found 5° and 10° noted in right and left knee respectively with a further flexion possible up to 120° bilaterally. Further evaluation showed that both the anterior superior iliac spine of the hip was at the same level without any increase in lumbar lordosis. Bilateral Hip joint flexion of up to 90° degrees was possible with painful restriction of internal and external rotation of the hips when the hips and knees were extended and in 90° of flexion. Radiological examination revealed severe degenerative changes of both knee and hip joint with tendinous calcification of the pelvis; spinal X-ray reveals ankylosis straightening of the lumbar lordosis with striking calcification of the intervertebral disc. Magnetic resonance imaging of the spine showed widespread involvement of the cervical and lumbar vertebrae with disc herniation at multiple levels (C4-5,C5-6,C6-7, T12-L1,L5-S1) (Fig. 1) without canal compromise at both cervical and lumbar spine with relative sparing of the dorsal vertebrae.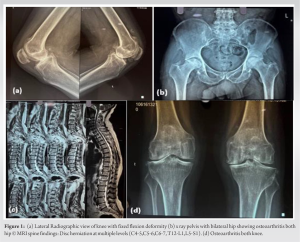
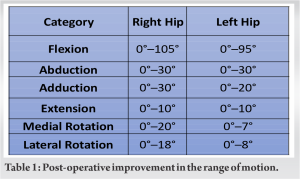
Patients with ochronotic arthropathy who also display complications such as spinal canal stenosis or prolapsed intervertebral disc, causing unilateral or bilateral buttock or lower extremity pain, heaviness, numbness, or weakness and which aggravates on walking, in cases as such treatment with THA show paramount clinical improvements (Fig. 1c). However, in the Asian culture, squatting is a common activity that can increase the risk of implant failure and dislocation after THA. Squatting involves deep flexion of the hip joint, which can cause the femoral head to move out of the socket of the implant, leading to instability and dislocation. In addition, the uneven distribution of forces on the implant during squatting can cause it to wear out or loosen over time. One successful option of this is the use of a DMC approach, as supported by multiple studies [10, 11]. In a retrospective study, the outcomes of 23 patients with ochronotic arthropathy who underwent THA with DMC has been shown to provide excellent stability and a low rate of dislocation, with no instances of aseptic loosening or implant fracture, which are common drawbacks of conventional surgical approaches [12]. Based on previously published data, DMC demonstrated greater efficacy compared to other implants in patients who underwent THA. In addition, a study found that the dual mobility group had a significantly lower rate of dislocation than the conventional group (1.5% vs. 6.7 %) [13]. Moreover, in another study consisting of 28 patients with ochronotic arthropathy, the DMC provided excellent stability and a low rate of dislocation, with no instances of component revision or dislocation. These findings have significant implications for future surgical procedures, particularly in terms of improving patient outcomes and reducing the risk of complications [14]. In patients at high risk of dislocation after primary THA, the DMC resulted in better outcomes than using fixed bearing THA. The study recommends the use of contemporary DM -bearing Vitamin-E-infused highly cross-linked polyethylene (VEPE) for patients with high life expectancy and early compelling hip stability. However, longer follow-up periods are necessary to assess the overall outcomes. This study highlights the importance of selecting the appropriate implant for THA in high-risk patients [15]. Overall, the use of a DMC in THA for ochronotic arthropathy appears to be a promising solution to the increased risk of dislocation associated with this condition. However, further research is needed to fully evaluate the long-term outcomes and potential complications of this approach.
The successful use of a DMC in THA for patients with ochronotic arthropathy improves joint stability, mobility, and decreases the risk of implant failure and dislocation. This treatment option has the potential to benefit patients with different degenerative diseases, including osteoarthritis, osteoporosis, and ochronotic arthropathy. However, patients must be informed about the possibility of consecutive replacement surgeries and recurrent postoperative effusions, which are frequently encountered in these patients. THA remains an effective and preferred treatment option for patients with ochronotic arthropathy, and the use of DMC can improve their quality of life.
The use of DMC in THA is increasing worldwide, with the primary aim of reducing dislocation rates. DMC offers the benefit of increased stability without compromising clinical outcomes and implant longevity. However, there may be potential complications such as postoperative infection and recurrent postoperative effusions. It is important to review the evidence for the indications for dual-mobility implants in both primary and revision THA.
References
- 1.Austin MS, Higuera CA, Rothman RH. Total hip arthroplasty at the rothman institute. HSS J 2012;8:146-50. [Google Scholar]
- 2.Khan AH, Afroze B, Majid H, Zaidi Y, Jamil A, Jafri L. Musculoskeletal manifestations in Alkaptonuria: A cross-sectional study. Medicine (Baltimore) 2021;100:e28241. [Google Scholar]
- 3.Bernini A, Spiga O, Santucci A. Structure-function relationship of homogentisate 1,2-dioxygenase: Understanding the genotype-phenotype correlations in the rare genetic disease alkaptonuria. Curr Protein Pept Sci 2023;24:380-92. [Google Scholar]
- 4.Couto A, Sá Rodrigues A, Oliveira P, Seara M. Ochronotic arthropathy-a rare clinical case. Oxf Med Case Reports 2018;2018:omy069. [Google Scholar]
- 5.Inoue S, Iwata Y, Yoh K, Nakamura Y, Maruo S. A case of ochronotic arthropathy treated with total hip arthroplasty. Mod Rheumatol 2003;13:270-6. [Google Scholar]
- 6.Hughes JH, Keenan CM, Sutherland H, Edwards HR, Wilson PJ, Ranganath LR, et al. Anatomical distribution of ochronotic pigment in alkaptonuric mice is associated with calcified cartilage chondrocytes at osteochondral interfaces. Calcif Tissue Int 2021;108:207-18. [Google Scholar]
- 7.Gil JA, Wawrzynski J, Waryasz GR. Orthopedic manifestations of ochronosis: Pathophysiology, presentation, diagnosis, and management. Am J Med 2016;129:536.e1-6. [Google Scholar]
- 8.Pachore JA, Shah VI, Upadhyay S, Shah K, Sheth A, Kshatriya A. Primary hip arthroplasty for the treatment of alkaptonuric hip arthritis: 3- to 24-year follow-ups. Arthroplasty 2019;1:8. [Google Scholar]
- 9.Kreipke R, Rogmark C, Pedersen AB, Kärrholm J, Hallan G, Havelin LI, et al. Dual mobility cups: Effect on risk of revision of primary total hip arthroplasty due to osteoarthritis. J Bone Joint Surg 2019;101:169-76. [Google Scholar]
- 10.Lee WC, Tan TL, Chan YH. Total knee arthroplasty in ochronosis arthropathy: A case report and systematic review. Case Rep Orthop 2019;2019:1871856. [Google Scholar]
- 11.Harada S, Hamai S, Gondo H, Higaki H, Ikebe S, Nakashima Y. Squatting after total hip arthroplasty: Patient-reported outcomes and in vivo three-dimensional kinematic study. J Arthroplasty 2022;37:734-41. [Google Scholar]
- 12.de l’Escalopier N, Dumaine V, Auberger G, Babinet A, Courpied JP, Anract P, et al. Dual mobility constructs in revision total hip arthroplasty: Survivorship analysis in recurrent dislocation versus other indications at three to twelve-year follow-up. Int Orthop 2020;44:253-60. [Google Scholar]
- 13.Aguado-Maestro I, de Blas-Sanz I, Sanz-Peñas AE, Campesino-Nieto SV, Diez-Rodríguez J, Valle-López S, et al. Dual mobility cups as the routine choice in total hip arthroplasty. Medicina (Kaunas) 2022;58:528. [Google Scholar]
- 14.Lunebourg A, Mouhsine E, Cherix S, Ollivier M, Chevalley F, Wettstein M. Treatment of type B periprosthetic femur fractures with curved non-locking plate with eccentric holes: Retrospective study of 43 patients with minimum 1-year follow-up. Orthop Traumatol Surg Res 2015;101:277-82. [Google Scholar]
- 15.Moon NH, Do MU, Kim JS, Seo JS, Shin WC. The usefulness of dual mobility cups in primary total hip arthroplasty patients at a risk of dislocation. Sci Rep 2022;12:774. [Google Scholar]