Tubercular osteomyelitis may sometime mimic Ewing’s sarcoma radiologically.
Dr. Aayush Arora, Department of Orthopaedic Surgery, Tata Motors Hospital, Jamshedpur, Jharkhand, India. E-mail: ayush.arora52@gmail.com
Introduction: Ewing’s sarcoma in children is an extremely rare malignant tumor that is frequently challenging to identify. In addition to its rarity in young children, Ewing’s sarcoma can resemble an infectious disease, contributing to diagnostic delay. Both conditions have similar presenting symptoms, such as general weakness, pain, and fever.
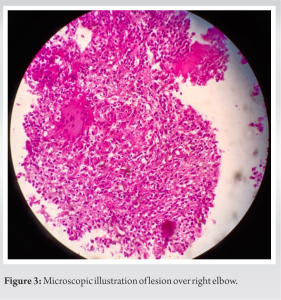
Case Report: We present a case of a 13-year-old girl with pain over the right distal humerus for 2 months. X-ray findings showed lesions over the distal humerus which led to a differential diagnosis of osteomyelitis and Ewing’s sarcoma. The patient underwent bone biopsy and was diagnosed with tuberculous osteomyelitis and was managed conservatively in the form of antituberculosis treatment.
Conclusion: For distinguishing Ewing’s sarcoma from osteomyelitis, imaging modalities can be unreliable, and these patients require a higher diagnostic yield in the form of a bone biopsy for greater accuracy.
Keywords: Osteomyelitis, Ewing’s sarcoma, young children.
Ewing’s sarcoma and infections both have similar routine investigation because leukocyte counts and erythrocyte sedimentation rates (ESR) show irregular elevations in both. Blood and tissue cultures may be sterile [1]. Atypical cases necessitate additional testing to rule out major differentials such as bone infection and skeletal tumors. The modality of choice for investigation is magnetic resonance imaging (MRI), and the assessment is determined through a combination of clinical and radiological follow-up to illustrate relapsing and remitting incidents [2]. However, distinguishing osteomyelitis from bone tumors remains difficult, particularly in long bones. Often, only after carefully examining the histologic characteristics of the lesions can a diagnosis be made. Unless tubercular osteomyelitis is promptly recognized and treated, it can be devastating with a high percentage of sequelae, particularly in resource-poor countries where patients present with advanced disease and survivors frequently have serious and long-term complications. Acute bone infection in children is most commonly caused by an hematogenous source [3]. We present a case of a 13-year-old female who presented with symptoms and investigations suggestive of osteomyelitis. This case also revealed histology suggestive of chronic osteomyelitis and was negative for malignancy. Despite negative microbiologic cultures, treatment was commenced on a presumptive diagnosis of osteomyelitis. The patient’s condition responded to antibiotic therapy and improved.
A 13-year-old patient presented to the outpatient department with a chief complaint of pain and swelling in the right elbow for 2 months. The patient was examined clinically and had tenderness over the lower aspect of the right arm. Radiograph of the right elbow was done in anteroposterior and lateral view which showed cortical thickening and periosteal reaction over the distal humerus (Fig. 1). MRI of the right elbow showed synovial thickening, marked joint effusion, and periosteal reaction measuring up to 7.3 mm extending into medial and lateral epicondyle. Moderate periarticular muscle edema was seen due to inflammation (Fig. 2). 
Children and young adults are the most commonly affected by chronic osteomyelitis. It is distinguished by sclerotic osseous lesions in the absence of a noticeable causative organism or tumor. Long bone metaphyses are those that are most frequently affected. The clavicle and spine are also seen as being involved. The disease has a slow onset and a protracted course. Patients tend to experience repeated pain episodes. The test results are sometimes non-specific but they do point to an inflammatory process. Elevated ESR, alkaline phosphatase, and C-reactive proteins (CRPs) are all illustrations of abnormal laboratory tests. The patient will almost never have an irregular white blood cell count [4]. Early differentiation between chronic osteomyelitis and a tumor of the bone is critical for rapid and suitable management [5]. Children with osteomyelitis usually have clinical signs 3–4 days before disease presentation. According to Abdietal, infection is much more prevalent in the lower limbs than the upper limbs, with the femur (27%), tibia (22%), and humerus (12%) being the most frequently affected sites. The involvement of a single bone is more frequent than multifocal involvement. More than half of all cases involve children below the age of five. Patients with pain, swelling, fever, and pathological fractures with fever are related to the dissemination of disease. X-rays show lytic destruction and the formation of subperiosteal new bone. These non-specific findings can occur in a variety of conditions, including metastatic carcinoma, malignant lymphoma, and osteomyelitis, requiring a biopsy to verify the diagnosis. Several cases of Ewing’s sarcoma being misdiagnosed as osteomyelitis have been reported. Misdiagnoses have been attributed to a lack of suspicion, occurrence at an unusual site, and inadequate histologic specimens [6]. On radiological evaluation, we (the World Health Organization) discovered that involvement of the metaphyseal region is more frequent in patients with Ewing’s sarcoma compared to those with bony osteomyelitis. In children with a lesion on the diaphysis and clinical manifestations of osteomyelitis, a biopsy of the lesion is required to make an unambiguous diagnosis [7]. In comparison to bone tumors, osteomyelitis did not have a high level of alkaline phosphatase above an age-appropriate level [8]. Until culture outcomes are accessible, real-time polymerase chain reaction could help guide antibiotic treatment [9]. A few recent researchers advocate the use of procalcitonin and another inflammatory marker, but we doubt it adds anything to CRP, which is less expensive and easier and faster to measure [10].
For an accurate and timely diagnosis of Mycobacterium tuberculosis osteomyelitis, a high level of clinical suspicion is required. The role of imaging modalities in distinguishing a benign lesion from an infective lesion is limited. As a result, biopsies play an important role in the early diagnosis and management of these patients.
Chronic tubercular osteomyelitis should always be considered as a differential diagnosis in cases appearing to be Ewing’s sarcoma clinically and radiologically.
References
- 1.Durbin M, Randall RL, James M, Sudilovsky D, Zoger S. Ewing’s sarcoma masquerading as osteomyelitis. Clin Orthop Relat Res 1998;357:176-85. [Google Scholar]
- 2.Nepal P, Alam SI, Sajid S, Sapire J, Ojili V. Rare presentation of chronic recurrent multifocal osteomyelitis of the Iliac wing mimicking Ewing’s sarcoma. SA J Radiol 2021;25:2030. [Google Scholar]
- 3.Peltola H, Pääkkönen M. Acute osteomyelitis in children. N Engl J Med 2014;370:352-60. [Google Scholar]
- 4.Bracamonte JD, Roberts CC. Chronic recurrent multifocal osteomyelitis mimicking osteosarcoma. Radiol Case Rep 2006;1:42-6. [Google Scholar]
- 5.Shimose S, Sugita T, Kubo T, Matsuo T, Nobuto H, Ochi M. Differential diagnosis between osteomyelitis and bone tumors. Acta Radiol 2008;49:928-33. [Google Scholar]
- 6.Abdi R, Taheri MM. A case report of Ewing’s sarcoma of tibial epiphysis with retrobulbar mass. J Surg Trauma 2015;3:23-5. [Google Scholar]
- 7.Tountas AA, Kwok JM. Acute hematogenous diaphyseal osteomyelitis in childhood. Can Med Assoc J 1985;132:1287-8. [Google Scholar]
- 8.Shimose, S., Sugita, T., Kubo, T., Matsuo, T., Nobuto, H., & Ochi, M. (2008). Differential diagnosis between osteomyelitis and bone tumors. Acta Radiologica, 49(8), 928–933. Doi:10.1080/02841850802241809. [Google Scholar]
- 9.Arkader A, Brusalis C, Warner WC Jr., Conway JH, Noonan K. Update in pediatric musculoskeletal infections: When it is, when it isn’t, and what to do. J Am Acad Orthop Surg 2016;24:e112-21. [Google Scholar]
- 10.Pääkkönen M, Peltola H. Simplifying the treatment of acute bacterial bone and joint infections in children. Expert Rev Anti Infect Ther 2011;9:1125-31. [Google Scholar]