The UBE fusion extension technique is a safe, less invasive and effective treatment option for lumbar interbody fusion extension and posterior pedicle screw revision with less morbidity and early recovery.
Dr. Rajendra Sakhrekar, Department of Spine Surgery, Yonsei Okay Hospital, Seoul, South Korea. E-mail: raj.sakhrekar1@gmail.com
Introduction: Recently, lumbar degenerative disease has been treated using unilateral biportal endoscopic (UBE) lumbar interbody fusion. However, the use of the UBE approach for symptomatic ASD following lumbar interbody fusion surgery isn’t illustrated widely in the literature. This case report and technical note describe the use of the UBE approach for symptomatic ASD.
Case Report: A 72-year-old female who underwent conventional fusion surgery elsewhere twelve years ago at the L5-S1 level presented with severe back pain (VAS 8/10) and radicular pain in both legs (left > right) (left VAS 7/10, right VAS 7/10) for 1 year with an ODI score of 70%. Preoperative X-ray and MRI showed dynamic instability with spondylolisthesis at L4–5. We performed an upper-level extension using UBE FES techniques to resolve ASD. The operative time was 132 minutes, blood loss was 40 ml. After surgery, the patient was followed up at 1 week, 6 weeks, 3 months, 6 months, 12 months, and 2 years. The pain and tingling sensation in the legs got better at the 1-week follow-up itself with a VAS score of 0/10 and an ODI score of 10% at the 2-year follow-up. Patient satisfaction was surveyed using Odom’s criteria at each follow-up visit (at 1 week, 6 weeks,3 months, 6 months, and 2 years) and found to be excellent. Postoperative imaging showed a good reduction and canal decompression at L4–5.
Conclusion: The UBE fusion extension technique for ASD is a safe, less invasive, and effective treatment option for lumbar interbody fusion extension and posterior pedicle screw revision with less morbidity and early recovery.
Keywords: Unilateral Biportal Endoscopic, Adjacent Segment Disease, Case Report, Technical Note
The term “adjacent segment disease” (ASD) refers to degeneration at mobile spinal segments above or below a fused spinal segment and generally following spinal fusion or other spine procedures. The rate of ASD after posterior lumbar fusion surgery varies from 8.5 to 69.4%. Still, a significant rise in the incidence of ASD was linked to older age, BMI, a history of smoking and hypertension, preoperative adjacent disc degeneration, long-segment fusion, superior facet violation, high lumbosacral joint angle, pre-and post-operative L1-S1 SVA, post-operative LL, and preoperative PI[1–6]. Various surgical approaches are described for symptomatic ASD after lumbar interbody fusion surgery. The most commonly used approach is a conventional lumbar fusion extension surgery which has disadvantages such as extensive muscle dissection which increases risks of infection blood loss and dural leaks, increased healing time with decreased mobility, increased post-operative pain, and slower return to work and life[7]. Recently, lumbar degenerative disease has been treated using unilateral biportal endoscopic (UBE) lumbar interbody fusion. However, the use of the UBE approach for symptomatic ASD following lumbar interbody fusion surgery isn’t illustrated widely in the literature. This case report and technical note describe the use of the UBE approach for symptomatic ASD.
A 72-year-old female who underwent conventional fusion surgery elsewhere twelve years ago at the L5-S1 level presented with severe back pain (VAS 8/10) and radicular pain in both legs (left > right) (left VAS 7/10, right VAS 7/10) for 1 year with an ODI score of 70%. Her pain aggravated on bending forward and performing daily routine activities. She also complained of severe intermittent neurological claudication with a claudication distance of less than 50 meters. On physical examination power in lower limbs was 5/5 as per the MRC grading and deep tendon reflexes were normal. She was a known case of diabetes Mellitus and hypertension on treatment with oral medications. Preoperative X-ray and MRI showed dynamic instability with spondylolisthesis at L4–5. We performed an upper-level extension using UBE FES techniques to resolve ASD. The operative time was 132 minutes, blood loss was 40 ml. After surgery, the patient was followed up at 1 week, 6 weeks, 3 months, 6 months, 12 months, and 2 years. The pain and tingling sensation in the legs got better at the 1-week follow-up itself with a VAS score of 0/10 and an ODI score of 10% at the 2-year follow-up. Patient satisfaction was surveyed using Odom’s criteria at each follow-up visit (at 1 week, 6 weeks,3 months, 6 months, and 2 years) and found to be excellent. Postoperative imaging showed a good reduction and canal decompression at L4–5 (Fig.1,2).
Technical note
Careful preoperative planning is a must for revision spine surgery as previously placed pedicle screws or rods must be removed, surgical records should be sought and studied along with dynamic X-ray images and three-dimensional computed tomography and MRI scans must be performed before surgery to confirm the state of existing pedicle screws, rods, anatomy, and fusion mass of the previous surgery with neurological structures, adhesions, and soft tissues. The patient is positioned prone under general endotracheal anesthesia. However, surgeons can choose limited epidural anesthesia with sedation or their preferred choice of anesthesia. UBE-TLIF (Unilateral Biportal Endoscopic Transforaminal Lumbar Interbody Fusion). The first step is to perform an endoscopic transforaminal lumbar interbody fusion (UBE-TLIF) for adjacent levels that need to be extended before removing the previously inserted pedicle screws and rods. The portals are designed under C-arm fluoroscopy, similar to the well-known UBE TLIF technique [8]. The surgeon makes ipsilateral skin incisions vertically (authors preferred choice) or transversely on the pedicles of the ASD level and screw head of and previous fusion level (Fig. 3). 

The curved curate is placed on the ventral side of the rod, and the rod is lifted slightly through the lever principle. After holding the end part of the exposed rods with a rod holder, the rods can be pulled out gently through the skin incision. After removing the rods, we insert the endoscope into the skin incision point of the adjacent area. We confirm the location of the pedicle screw head using an endoscopic view. Finally, we attach a screwdriver to the screw head under endoscopic guidance. We then remove the pedicle screws. After removing the old screw, the entrance of the screw insert hole can be checked directly through the endoscope. We insert guide wires into the pedicle screw holes for the new pedicle screw insertion. The above-mentioned actions are repeated to remove all old screws and replace them with guide wires for new pedicle screws. The subsequent process is similar to the usual method of using the percutaneous pedicle screw system. In terms of lumbar interbody cage insertion and fusion on the level of ASD, complications of UBE FES techniques were similar to fusion surgeries using the unilateral biportal technique[8, 9]. In cases of old or broken hardware retained from previous surgeries, it may be difficult to remove the hardware under endoscopic assistance because the screw and head system may be complicated. In such cases, it is beneficial to switch to open surgery.
In 2015, Soliman published surgical results for lumbar disc herniation and spinal stenosis, using two independent portals, which is very similar to the current surgical technique to today’s UBE technique[10]. The advantages of continuous irrigation facilitating hemostasis, flushing of small bleeding, identification of the bleeding source, better identification of micro-anatomy under direct vision, and separation of tissue layers by simple irrigation and developments of instrumentation increased success rates and decreased complication rates of spinal surgeries using UBE over the last decade and widened the spectrum of indications. Currently, the UBE technique is used for discectomy and nerve decompression, spinal canal stenosis, excision of the perineural cysts, facet cysts, irrigation and debridement of an epidural abscess, excision of epidural lipomatosis, foraminal stenosis decompression, lumbar interbody fusion, and revision spine surgery. This study demonstrates UBE-assisted extension of fusion for ASD [11–15]. In addition, the implementation of UBE technology does not require the purchase of special lenses and instruments as seen in the percutaneous transforaminal endoscopic technique. UBE can use general arthroscopic lenses and open spinal surgical instruments, which is more conducive to wide acceptance in most hospitals. The unilateral biportal endoscopic (UBE) approach necessitates appropriate coordination between both hands and steady instrument operation with a single hand through the working portal. Both hands are required to operate simultaneously, the authors preferred to handle the lens in the non-dominant left hand and surgical tools in the right dominant hand. Spinal surgeons need to familiarize themselves with the arthroscopic tools and synchronize their perception of the depth and direction of the lens, move the instruments swiftly and smoothly in and out of the instrument channel, and quickly acquire the field of view in the early phase of the procedure during their learning curve. This study demonstrates the use of UBE-assisted extension of fusion for ASD which has several advantages including minimizing extensive muscle dissection, less blood loss, less post-operative pain, and faster recovery from the surgery. In this technique, adjacent level fusion is done with the advantages of the UBE technique and the previous surgery hardware is removed by exposing only the periphery of the screw head and under endoscopic vision. Furthermore, dural tear and cerebral spinal fluid (CSF) leakage from the previous laminectomy and risks of infection are very low as the muscle dissection with UBE is minimal (Fig 5). 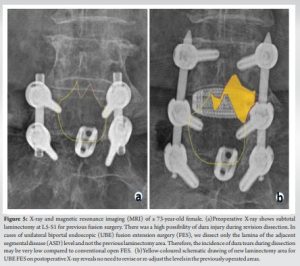
The UBE fusion extension technique for ASD is a safe, less invasive, and effective treatment option for lumbar interbody fusion extension and posterior pedicle screw revision with less morbidity and early recovery.
The UBE fusion extension technique for ASD is safe, and less invasive with good clinical and radiological outcomes with less morbidity and early recovery.
References
- 1.Wang T, Ding W. Risk factors for adjacent segment degeneration after posterior lumbar fusion surgery in treatment for degenerative lumbar disorders: a meta-analysis. J Orthop Surg Res 2020;15:582. https://doi.org/10.1186/s13018-020-02032-7. [Google Scholar]
- 2.Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, Lee MY. Risk factors for adjacent segment disease after lumbar fusion. European Spine J 2009;18:1637–1643. https://doi.org/10.1007/s00586-009-1060-3. [Google Scholar]
- 3.Soh J, Lee JC, Shin BJ. Analysis of Risk Factors for Adjacent Segment Degeneration Occurring More than 5 Years after Fusion with Pedicle Screw Fixation for Degenerative Lumbar Spine. Asian Spine J 2013;7:273. https://doi.org/10.4184/asj.2013.7.4.273. [Google Scholar]
- 4.Shasti M, Koenig SJ, Nash AB, Bahrami S, Jauregui JJ, O’Hara NN, Jazini E, Gelb DE, Ludwig SC. Biomechanical evaluation of lumbar lateral interbody fusion for the treatment of adjacent segment disease. Spine J 2019;19:545–551. https://doi.org/10.1016/j.spinee.2018.09.002. [Google Scholar]
- 5.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 2004;4:S190–S194. https://doi.org/10.1016/j.spinee.2004.07.007. [Google Scholar]
- 6.Adogwa O, Parker SL, Shau DN, Mendenhall SK, Devin CJ, Cheng JS, McGirt MJ. Cost per quality-adjusted life year gained of laminectomy and extension of instrumented fusion for adjacent-segment disease: defining the value of surgical intervention. J Neurosurg Spine 2012;16:141–146. https://doi.org/10.3171/2011.9.SPINE11419. [Google Scholar]
- 7.Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev 2019;42:753–761. https://doi.org/10.1007/s10143-019-01114-3. [Google Scholar]
- 8.Han H, Song Y, Li Y, Zhou H, Fu Y, Li J. Short-term clinical efficacy and safety of unilateral biportal endoscopic transforaminal lumbar interbody fusion versus minimally invasive transforaminal lumbar interbody fusion in the treatment of lumbar degenerative diseases: a systematic review and meta-analysis. J Orthop Surg Res 2023;18:656. https://doi.org/10.1186/s13018-023-04138-0. [Google Scholar]
- 9.Gao X, Gao L, Chang Z. Case series of unilateral biportal endoscopic-assisted transforaminal lumbar interbody fusion in the treatment of recurrent lumbar disc herniation. Am J Transl Res 2022;14:2383–2392. [Google Scholar]
- 10.Soliman HM. Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J 2015;15:2282-9. https://doi.org/10.1016/j.spinee.2015.07.009. [Google Scholar]
- 11.Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: a comprehensive review. Expert Rev Med Devices 2019;6:373–380. https://doi.org/10.1080/17434440.2019.1610388. [Google Scholar]
- 12.Heo DH, Park CK. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg Focus 2019;46:E18. https://doi.org/10.3171/2019.1.FOCUS18695. [Google Scholar]
- 13.Heo DH, Hong YH, Lee DC, Chung HJ, Park CK. Technique of Biportal Endoscopic Transforaminal Lumbar Interbody Fusion. Neurospine 2020;17:S129–S137. https://doi.org/10.14245/ns.2040178.089. [Google Scholar]
- 14.Heo DH, Lee DC, Kim HS, Park CK, Chung H. Clinical Results and Complications of Endoscopic Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Meta-Analysis. World Neurosurg 2021;145:396–404. https://doi.org/10.1016/j.wneu.2020.10.033. [Google Scholar]
- 15.Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus 2017;43:E8. https://doi.org/10.3171/2017.5.FOCUS17146. [Google Scholar]














