This article elaborates our experience in managing a diabetic foot attack and explains the importance of early recognition and aggressive management.
Dr. Aakaash Venkatesan, Department of Trauma and Orthopaedics, Grange University Hospital, Aneurin Bevan Trust, NP44 8YN, United Kingdom. E-mail: aakaash.venkatesan2@wales.nhs.uk
Introduction: Diabetic foot attack (DFA), also known as diabetic foot ulceration, is a severe and potentially limb-threatening complication of diabetes mellitus. It refers to the development of open sores or ulcers on the feet of individuals with diabetes, often leading to infections, tissue damage, and, in extreme cases, amputation. The underlying cause of DFAs is multifactorial and involves a complex interplay of various factors, including peripheral neuropathy, peripheral arterial disease, foot deformities, impaired wound healing, and poor glycemic control. This case report would be first of its kind from an orthopedic perspective.
Case Report: A 55-year-old white British gentleman, a chronic uncontrolled Type 2 diabetic, was referred by the medical team on a busy on-call night. He presented with a sudden onset pain, swelling, and difficulty in weight bearing on his left foot. He had a non-healing plantar ulcer for over a year. His inflammatory markers were abnormally high and magnetic resonance imaging of his leg and foot showed massive collection in his foot with gas extending along the posterior compartment. Diagnosis of a severe DFA was made, and urgent debridement and washout were carried out. Despite aggressive debridement, patient progressively deteriorated warranting an admission into intensive care unit. After subsequent debridement and local antibiotic therapy, he recovered and was discharged with clinic follow-up.
Conclusion: Effective management strategies for DFAs encompass a multidisciplinary approach. Preventive measures play a key role in reducing the incidence of DFAs. Regular foot examinations, self-care education, proper glycemic control, and foot hygiene are essential components of preventive strategies. Patient education regarding self-monitoring, appropriate footwear, and early recognition of foot-related complications is crucial to empower individuals with diabetes to take proactive measures.
Keywords: Diabetic foot attack, debridement, local antibiotic delivery, time is tissue.
Diabetic foot disease is a major global challenge with the ever-increasing prevalence of diabetes. There has been a significant raise in the incidence of complications related to the diabetic foot disease and in turn the mortality rate. The costs incurred by both the individuals and the health care system are considerably high. The diabetes UK have estimated that the cost incurred by National Health Service in England was approximately 1.25 billion pounds in 2020–2021 and has predicted a further raise [1]. Each year, 60,000 patients present with Diabetic Foot Ulceration in the UK and 5 -year mortality rate for these patients is around 50% [2]. A comparison has been made between diabetic foot attack (DFA) and acute cardiac or cerebrovascular events. Similar to the latter, DFA could present as a subtle one, where in patients would not be able to recognize the symptoms at the initial stages. The presence of peripheral neuropathy, which would possibly dampen the local host defenses without obvious signs of inflammatory response. Patients can present with tissue necrosis as the first presenting sign due to the same reason. With the increasing rates of lower limb amputations, strategies similar to the golden hour management used in myocardial infarction and cerebro vascular accidents need to be employed in DFA. Hence, the concept of “time is tissue” has been promoted recently. It involves a pragmatic early recognition and intervention [3]. British Orthopaedic Foot and Ankle Society has laid down guidelines for management of acute DFA, which involves multidisciplinary approach, where in the Foot and Ankle surgeon takes the lead for the surgical management. The guidelines basically outline a tri-pronged intervention by urgent magnetic resonance imaging (MRI) to delineate affected tissue from the normal planes, aggressive and targeted intravenous antibiotic therapy, and aggressive surgical debridement exploring all the affected tissue planes [4]. Recently, use of Stimulan (antibiotic impregnated beads) has shown promising results in effective control of local infection, studies have shown that there has been 90% healing rates in severe diabetic foot infections with a mean healing time of 12 weeks and significant reduction in the use of systemic antibiotics and the related side effects [5]. We hereby share our experience on managing a case of acute DFA in a district general hospital.
A 55-year-old gentleman presented to A and E with 24 h history of increasing swelling and redness of his left foot with associated superficial blistering. He had poorly controlled Type 2 diabetes mellitus (HbA1C- 95 mmol/mol) and associated peripheral neuropathy. He had an injury to the plantar aspect of his left foot, while he was on a holiday in July 2022 and developed a non-healing ulcer ever since and has been managed without surgery. On presentation, he had a red, hot, and swollen left foot with an infected plantar ulcer. His inflammatory markers were significantly elevated (C-reactive protein [CRP]-295 mg/L). He has a background of metastatic renal cell carcinoma with brain metastases managed with chemotherapy and Grade-2 hepatitis secondary to immunotherapy awaiting a liver biopsy. He was started on broad spectrum antibiotics and a MRI showed a collection measuring 48 × 37 × 35 mm extending from the dorsal to the plantar aspect of the foot traversing between second and third metatarsal heads with chronic osteomyelitis around third metatarsal head (Fig. 1).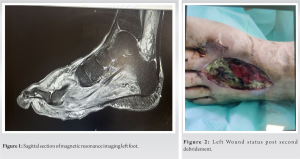
DFA is one of the most devastating presentations of diabetic foot disease, presents as an acute inflammation associated with rapid progressive necrosis, without timely intervention can rapidly progress to limb and life-threatening complications [6]. This can be an entirely new presentation or sudden deterioration of a diabetic foot ulcer, ischemia, or both. Immediate recognition and urgent aggressive management are the key to limb salvage and patient survival [7]. Thus, the concept of “Time is Tissue” referring to tissue salvage and maximal limb preservation plays a significant role. The use of term DFA has been more of a recent development [3]. DFA could manifest as typical and atypical presentation. Typical presentation can start as an apparent simple injury but could rapidly escalate over hours to life-threatening proportions. Atypical presentations are more subtle, may follow a chronic ischemic limb, more frequently in diabetes and despite the distinct pathophysiological process involved, inflammatory stage of Charcot’s foot could also be considered to be an atypical presentation.
The ideal management plan of a DFA would be to prevent it from developing. International guidelines do not provide much information on management of DFA but do mention on how to recognise the severity of the presentation and act accordingly. For instance, international working group on diabetic foot has laid down recommendations on management of DFA. The key is not to underestimate the extent of damage caused by the speed of deterioration though, it may appear local, but might have already advanced along the tissue planes and tendon sheaths. The identification of this limb and life-threatening infection involves clinical, radiological and microbiological investigations.
A proper clinical assessment would definitely aid in identification of this infection and prevent catastrophe, along with basic blood investigations including the infection markers would further enhance in the diagnosis. Diabetic foot ulcer infections are generally polymicrobial (especially bacterial and Fungal). Although fungal infections are more common in tropical and sub-tropical regions, we would like to emphasise the importance of ruling out fungal infections in treating DFAs. This would aid in treatment planning and predicting the possible outcomes and prognosis. Dermatophyte infections of toe web spaces provide an environment for subsequent colonization by bacteria [8-11]. Fungal infections in the foot could either be superficial or more complicated deep tissue infections. Candida species being the commonly delineated organism. The incidence of fungal infection was directly related to the duration of diabetes mellitus. Patients with a mean duration of diabetes of 7.7 years were having fungal infections [11]. We have ruled out fungal infection based on tissue cytology in our patient though an adequate microbiological assessment for fungal infection on our samples would have been beneficial. A trimodal approach of rapid surgical debridement has been suggested along with adequate radiological investigations. Although a MRI or computed tomography would definitely aid in surgical planning as it would aid in delineating the extent of collection, presence of gas loculations within soft tissues (indicating severity of infection), extent of bony involvement; a simple plain radiograph would be sufficient enough to diagnosing bone involvement in cases of severe diabetic foot infections. In centres with limited resources, an ultrasound along with plain radiograph could definitely aid in surgical planning, as DFAs are limb threatening conditions which in turn can progress to harm life. However, both ultrasound and plain radiograph would not be able to provide a surgical target, as the extent of infection is not clearly delineated. Hence, we would like to emphasize the transfer of patient care to a higher center for further management. Culture-specific antibiotic therapy is of crucial importance in treating severe diabetic foot infections.[8] Manas et al. [10] compared deep wound samples taken at the time of admission with those taken during the surgical debridement and concluded only fair concordance between the two samples. Although it has been polymicrobial, various studies suggest that S. aureus has been the most prevalent, highly consistent pathogen in severe diabetic foot infections, as it has a bone penetration time of <30 min on exposure [12]. Alongside targeted antibiotic therapy and fluid resuscitation, aggressive surgical debridement plays a key role in management of DFAs. Most of these infections would warrant multiple debridements in theater to control the spread and vigour of the infection. Long duration of intravenous antibiotics has its own downside, including the side effects. Hence, local antibiotic delivery systems have been utilized alongside aggressive surgical debridement. In our case study, we had utilized local antibiotic delivery system (stimulan) and has proved to be very effective. Patient was given a course of oral antibiotics to complete the treatment. Wai et al. [5], in their case series states that there has been a significant reduction in the amputation rates using local antibiotic delivery system. Qin et al. [13], in their study, have described that there has been a significant healing in almost all patients on local antibiotic delivery system alongside surgical debridement in comparison, with those on intravenous antibiotics post-debridement.
There has been a significant surge in the number of DFA presentations in the UK. Prevention is the key, but early recognition and active intervention would aid in preventing limb and life-threatening complications.
Diabetes UK has produced a booklet on “How to spot a Foot Attack” for people who have been identified as at risk. This booklet has been circulated among the GP’s in United Kingdom. This would help in early recognition of a foot attack and a rapid response to control and prevent its progression to a point where it might lead to limb loss and even death. The strength of the pathway and a multidisciplinary team is that the patients are referred at appropriate time to prevent such complications.
We would like to conclude by stating that a tri-pronged intervention by urgent MRI to delineate the affected from normal tissue planes, aggressive and targeted IV antibiotic therapy, and aggressive surgical debridement exploring all the tissue planes of the affected limb alongside local antibiotic delivery system is the way forward in managing these aggressive infections.
This article elaborates our experience in managing a DFA and explain the importance of early recognition and aggressive management.
References
- 1.Diabetes.co.uk - The Global Diabetes Community. Diabetes.co.uk; 2018. Available from: https://www.diabetes.co.uk [Last accessed on 03/09/2023]. [Google Scholar]
- 2.National Diabetes Foot Care Audit. NHS Digital. Available from: https://digital.nhs.uk/data-and-information/clinical-audits-and-registries/national-diabetes-foot-care-audit [Last accessed on 03/09/2023] [Google Scholar]
- 3.Vas PR, Edmonds M, Kavarthapu V, Rashid H, Ahluwalia R, Pankhurst C, et al. The diabetic foot attack: “’Tis too late to retreat!”. Int J Low Extrem Wounds 2018;17:7-13. [Google Scholar]
- 4.BOFAS > Hyperbook > Systemic Disorders > Diabetic Foot > Acute Diabetic Foot. Available from: https://www.bofas.org.uk/hyperbook/systemic-disorders/diabetic-foot/acute-diabetic-foot [Last accessed on 2023 Jul 06]. [Google Scholar]
- 5.Ting H, Hamish M, Kirupananthan P, Gmati A, Abdalla H, Hicks R. Stimulan® antibiotic impregnated beads for the treatment of diabetic foot infection. Arab J Intervent Radiol 2020;4:73-8. [Google Scholar]
- 6.Ahluwalia RS, Reichert IL. Surgical management of the acute severely infected diabetic foot - The “infected diabetic foot attack”. An instructional review. J Clin Orthop Trauma 2021;18:114-20. [Google Scholar]
- 7.Vig S, Alchikhal T, Turner B. The foot attack: Where are the defence mechanisms? Br J Diabetes 2014;14:72. [Google Scholar]
- 8.Soldevila-Boixader L, Fernández AP, Laguna JM, Uçkay I. Local antibiotics in the treatment of diabetic foot infections: A narrative review. Antibiotics (Basel) 2023;12:124. [Google Scholar]
- 9.Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann Med 2016;49:106-16. [Google Scholar]
- 10.Manas AB, Taori S, Ahluwalia R, Slim H, Manu C, Rashid H, et al. Admission time deep swab specimens compared with surgical bone sampling in hospitalized individuals with diabetic foot osteomyelitis and soft tissue infection. Int J Low Extrem Wounds 2020;20:153473462091638. [Google Scholar]
- 11.Kandregula S, Behura A, Behera CR, Pattnaik D, Mishra A, Panda B, et al. A clinical significance of fungal infections in diabetic foot ulcers. Cureus 2022;14:e26872. [Google Scholar]
- 12.Yu K, Song L, Kang HP, Kwon HK, Back J, Lee FY. Recalcitrant methicillin-resistant Staphylococcus aureus infection of bone cells: Intracellular penetration and control strategies. Bone Joint Res 2020;9:49-59. [Google Scholar]
- 13.Qin CH, Zhou CH, Song HJ, Cheng GY, Zhang HA, Fang J, et al. Infected bone resection plus adjuvant antibiotic-impregnated calcium sulfate versus infected bone resection alone in the treatment of diabetic forefoot osteomyelitis. BMC Musculoskelet Disord 2019;20:246. [Google Scholar]









