Management of Central fracture dislocation of the hip with delayed one staged Total Hip Replacement has good functional outcome.Dual mobility cup is essential in patients with parkinsonism and other neurodegenerative disorders.
Dr. Akshay V Pawar, MUHS Fellow, Department of Arthritis and Joint Replacement Surgery, Nanavati Hospital, Mumbai - 400 056, Maharashtra, India. E-mail: akshaypawar993@gmail.com
Introduction: The combination of a central fracture-dislocation of the hip, acetabulum fracture, and neck of the femur fracture is a rare injury, with a few reports described in the literature. Guidelines regarding managing this type of injury in single or multiple stages, the requirement of acetabular augmentation with plates, metal rings or cages, and the implant selection in elderly patients are not adequately defined while planning a total hip arthroplasty (THA). The successful management of such a complex fracture pattern in an elderly patient with neurodegenerative disorder is described in our case report.
Case Report: An 81-year-old male presented to our outpatient department with a 2-month-old neglected post-traumatic central fracture-dislocation of the right hip with an ipsilateral femoral neck fracture. The patient had a known case of Parkinson’s disease on treatment with oral medication. A single-stage hybrid THA with dual mobility (DM) prosthesis was done with femoral head autograft acetabular impaction bone grafting. The patient was mobilized full weight bearing with the support of a walker on the 2nd post-operative day. At the 1-year follow-up the functional Harris hip score was 87. Radiographs revealed a well-healed acetabular fracture with the incorporation of a bone graft. No signs of implant loosening were observed. We did not encounter any complications such as dislocation, infection, and heterotrophic ossificans.
Conclusion: Management of central fracture-dislocation of the hip with delayed one-staged THA has a good functional outcome. DM cup is essential in patients with parkinsonism and other neurodegenerative disorders.
Keywords: Central fracture-dislocation of the hip, neck of femur fracture, total hip arthroplasty, dual mobility, Parkinsonism.
The combination of a central fracture-dislocation of the hip, acetabulum fracture, and a fractured neck of the femur is a rare injury, with a few reports described in the literature [1-7]. However, this type of injury pattern in an elderly patient with parkinsonism and its management with dual mobility (DM) total hip arthroplasty (THA) has not been described till now, and to our knowledge, this is the first case report described in the literature. The successful management of such a complex fracture pattern is highlighted in our case report.
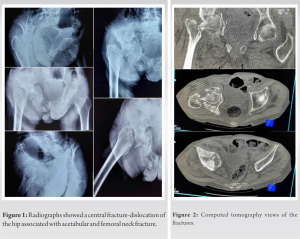
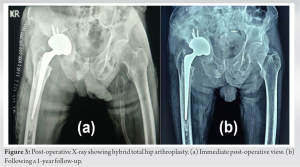
An 81-year-old male presented to our outpatient department with a history of falls at home and was unable to walk for 2 months. On clinical examination, there was tenderness over the right hip and proximal femur. The right limb shortening of 5 cm and external rotation deformity were present. Radiographs showed a central fracture-dislocation of the right hip associated with ipsilateral femoral neck fracture (Fig. 1). CT examination revealed a comminuted transverse acetabular fracture with a central migration of the femoral head fragment into the pelvic cavity (Fig. 2). There was no associated neurovascular injury.
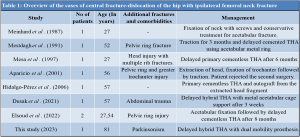
The patient had a known case of parkinsonism and was on oral tablets levodopa, carbidopa, and pramipexole for the treatment. As a definitive treatment, we planned to do femoral head autograft and THA with DM prosthesis. The hip joint was exposed by a posterior approach. The femoral head was migrated medially and embedded in the acetabular fracture. It was engaged with a corkscrew and found to be mobile inside the acetabular cavity and was extracted out with the assistance of blunt Hohman retractors without damaging the acetabular wall. On palpating the inner wall, the acetabulum showed a contained defect without any obvious breach into the pelvic cavity. We used the morselized cancellous bone from the femoral head to do impaction bone grafting over the acetabular defect. Additional reverse reaming was done over the impacted bone graft. A 54-mm cementless hydroxyapatite-coated cluster acetabular shell (Modular DM Trident PSL, Stryker, USA) was used to achieve a perfect fit. A high offset 37.5 mm size 1 cemented stem was used for the femur (Exeter, Stryker, USA) with a 28 mm metal head articulating with a highly cross-linked polyethylene DM liner of 46 mm. The wound was closed in layers without a drain.
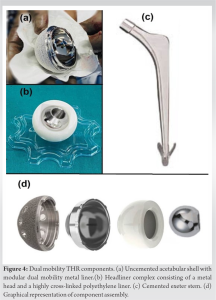
The patient was mobilized full weight bearing with the support of a walker on the 2nd post-operative day. There was no limb length discrepancy. He was able to do active straight leg raising and abduction against gravity by the 3rd week. At the end of 3 months, the patient was walking unaided with a stable and pain-free hip. At the 1-year follow-up, the functional Harris hip score was 87. Radiographs revealed a well-healed acetabular fracture with the incorporation of a bone graft. No signs of loosening were observed (Fig. 3). We did not encounter any complications such as dislocation, infection, and heterotrophic ossification.
Based on our literature search, this injury pattern was reported only in seven cases [1-7]. All these cases were in young patients without any neuromuscular abnormalities and were managed with fixation of fracture or a standard THA prosthesis (Table 1).
In elderly patients with femur neck fractures, there is a high risk of non-union and avascular necrosis of the head, especially in cases of significant displacement, and the treatment of choice is THA [8]. While planning a THA, guidelines regarding managing this type of injury in single or multiple stages, the requirement of acetabular augmentation with plates, metal rings, or cages and the implant selection in elderly patients are not adequately defined. Delayed THA after more than 3 months was successful in three studies [2, 3, 7]. In the case report by Dusak et al., delayed management after 3 weeks by primary cemented THA with bone grafting of the acetabular defect and insertion of an acetabular cage fixed with multiple screws was done [6]. Femoral head extraction and impaction bone grafting to strengthen the acetabular bed are recommended in previous studies for contained acetabular defects [6, 7]. Mesdadah in his case report did not extract the head fragment out during delayed THA. The CT scan showed that the head fragment had healed well and fused to the acetabular roof and column without going into avascular necrosis, thus creating a consistent acetabular bed. The entire mass was progressively reamed and a metal ring was inserted and fixed with screws. A cemented THA was done over this construct [2]. The use of cemented stem prostheses provides initial stability and immediate weight-bearing ambulation in elderly patients with osteoporosis. Parkinson’s disease (PD) is the most common movement disorder and represents the second most common degenerative disease of the central nervous system. It is characterized by worsening motor symptoms, including resting tremors, bradykinesia, rigidity, shuffling gait, and poor muscle coordination. The onset of the disease is usually at an age of 65–70 years. PD prevalence is increasing with age and PD affects 1% of the population above 60 years [9]. Patients with PD undergoing THA are at increased risk for medical complications and surgery complications, particularly superficial wound infection and deep vein thrombosis as compared to patients without PD. PD patients also exhibit increased length of stay and total hospital charges [10]. The instability in PD patients can potentially make them more likely to fall, resulting in post-operative prosthesis dislocation and periprosthetic fracture [11]. While there are no substitutes for proper positioning of the components and meticulous soft-tissue repair, DM implants can improve stability in patients with unmodifiable risk factors for dislocation. The use of DM THA is recommended in patients having a high risk of falls, neurodegenerative disorder, hip fractures, history of alcohol abuse, spine pathology, and other factors placing the patient at a high risk of dislocation [12]. DM systems allow the head-liner complex to function as a large femoral head, increasing the head-neck ratio and jump distance, thereby improving stability and terminal impingement (Fig. 4).
Our case report highlights the management of a complex hip fracture in an elderly with neuromuscular movement disorder with a good clinical outcome. Priority should be given for the evaluation of other injuries and stabilization of the patient as such complex fracture patterns are often associated with polytrauma. Central fracture-dislocation of the hip with a comminuted acetabular fracture can be successfully managed with delayed THA without acetabular fixation or metal cages. The use of DM prosthesis is beneficial in such situations as it decreases the risk of dislocation in elderly high-risk patients.
Management of central fracture-dislocation of the hip with delayed one-staged THA has a good functional outcome. A dual mobility cup is essential in patients with parkinsonism and other neurodegenerative disorders.
References
- 1.Meinhard BP, Misoul C, Joy D, Ghillani R. Central acetabular fracture with ipsilateral femoral-neck fracture and intrapelvic dislocation of the femoral head without major pelvic-column disruption. A case report. J Bone Joint Surg Am 1987;69:612-5. [Google Scholar]
- 2.Mestdagh H, Butruille Y, Vigier P. Central fracture-dislocation of the hip with ipsilateral femoral neck fracture: Case report. J Trauma 1991;31:1445-7. [Google Scholar]
- 3.Mesa AC, Manent RB, Rodriguez RP, Canto MP. Intrapelvic dislocation of the femoral head after central acetabular and femoral neck fracture. HIP Int 1997;7:75-7. [Google Scholar]
- 4.Aparicio AM, Garcia MD. Central acetabular fracture associated with ipsilateral fracture of the femoral neck with intrapelvic migration of the femoral head. Journal of Orthopaedics Surgery and Traumatology.2001;45:228-30. [Google Scholar]
- 5.Hidalgo-Perez M, Garces-Castillo J, Moleon-Camacho M. Central acetabular fracture-dislocation with intrapelvic migration of the fractured femoral head at the basicervical level . Journal of Orthopaedics Surgery and Traumatology.2006;50:217-9. [Google Scholar]
- 6.Dusak WS, Dharmayuda CG, Kawiyana KS, Afandi R, Nugraha GK. Central fracture dislocation of the hip associated with fracture of femoral neck treated by femoral head autograft and total hip arthroplasty: A rare case report. Int J Surg Case Rep 2021;78:90-5. [Google Scholar]
- 7.Abo-Elsoud M, El-Gebeily M, El-Desouky I. Combined acetabular and femoral neck fractures with intrapelvic femoral head dislocation: Successful staged management of a rare injury in two cases. Jt Dis Relat Surg 2022;33:230-7. [Google Scholar]
- 8.Ossendorf C, Scheyerer MJ, Wanner GA, Simmen HP, Werner CM. Treatment of femoral neck fractures in elderly patients over 60 years of age - which is the ideal modality of primary joint replacement? Patient Saf Surg 2010;4:16. [Google Scholar]
- 9.Tysnes OB, Storstein A. Epidemiology of Parkinson’s disease. J Neural Transm (Vienna) 2017;124:901-5. [Google Scholar]
- 10.Min H, Lin H, Chen G. Effect of Parkinson’s disease on primary total joint arthroplasty outcomes: A meta-analysis of matched control studies. Int J Surg 2019;71:124-31. [Google Scholar]
- 11.Balash Y, Peretz C, Leibovich G, Herman T, Hausdorff JM, Giladi N. Falls in outpatients with Parkinson’s disease: Frequency, impact and identifying factors. J Neurol 2005;252:1310-5. [Google Scholar]
- 12.Vajapey SP, Fideler KL, Lynch D, Li M. Use of dual mobility components in total hip arthroplasty: Indications and outcomes. J Clin Orthop Trauma 2020;11(Suppl 5):S760-5. [Google Scholar]