In cervical spine fractures, vascular examinations by CTA or DSA should be performed in the early phase.
Dr. Taiki Isaji, Department of Neurosurgery, Nagoya Tokushukai General Hospital, 2-52 Kozojikita, Kasugai, Aichi, Japan. E-mail: isaji.taiki.007@gmail.com
Introduction: Blunt cervical injuries rarely cause vertebral artery injuries (VAIs), such as vertebral artery (VA) dissection or occlusion. To prevent subsequent embolic infarction, embolization of the injured VA is needed before surgical fixation of the cervical spine. However, evidence on endovascular treatment for asymptomatic low-grade VAIs with blunt traumatic cervical injury is insufficient.
Case Report:In the present case, a 79-year-old Japanese man presented tetraparesis after falling while walking. Digital subtraction angiography showed no intimal flap and only slight stenosis of the right VA. Embolization was not performed before spinal decompression surgery for this low-grade injury. However, on the 3rd day after surgery, diffuse-weighted imaging showed dot-like high signal intensity in the right thalamus and right posterior lobe, and magnetic resonance angiography (MRA) showed near occlusion of the right VA. 8 days after surgery, MRA showed recanalization of the right VA flow. We performed VA embolization to prevent emboli scattering to the distal region during recanalization of the intracranial blood flow.
Conclusion: According to the relevant literature, prophylactic embolization may be indicated to prevent the embolic infarction not only in cases of VA occlusion requiring fixation of the cervical spine but also in cases of low-grade VAIs in which fixation is not required. Embolization of the VA before spinal surgery might be an aggressive treatment strategy that avoids serious embolic infarction disorder after VAIs.
Keywords: Blunt cervical injury, vertebral artery injury, cervical fracture
Blunt cervical injuries (BVIs) rarely cause vertebral artery injuries (VAIs), such as dissection and occlusion. The reported incidence rate of VAI in patients with BVIs ranges from 0.24% to 2% [1-6]. Although the patients with VAI often have no symptoms at the beginning of the injury, embolic infarction can develop in the occipital lobe, cerebellum, and brainstem regions. These can cause very serious permanent disability: Consciousness disorder, motor paralysis, visual field disturbance, and dysphagia. Biffl et al. reported the classification for blunt cerebrovascular injury according to their angiographic appearance using the Denver grading scale [4, 7] (Table 1). Embolization of the injured vertebral artery (VA) must be performed before surgical fixation of the cervical spine to prevent subsequent embolic infarction. In the present case, the right VAI is classified as Grade Ⅰ. Although fracture through the transverse foramen (TF) was recognized, initial digital subtraction angiography (DSA) showed only slight stenosis and no obvious intimal flap. Moreover, as cervical spine surgery, only posterior decompression procedure was required; the patient did not need repositioning or fixation surgery. Therefore, pre-operative embolization of the VA was not performed. Nevertheless, 3 days after spinal surgery, the injured VA was occluded, with recanalization occurring 8 days after surgery. The indications for antithrombotic drugs and endovascular surgery in the treatment of asymptomatic low-grade traumatic VAIs have not been well established. In the present article, we discuss tactics of therapy for low-grade asymptomatic VAI in a patient who underwent surgical decompression of the cervical spine, but who did not require fixation.
The patient was a 79-year-old man who presented bilateral upper and lower limb paralysis after falling while walking. He had left lateral upper arm pain. Manual muscle testing revealed the following results: Right deltoid muscle, 3; left deltoid muscle, 4; right biceps muscle, 3; left biceps muscle, 4; right triceps muscle, 3; left triceps muscle 4; bilateral wrist flexors, 3/3; right wrist extensors, 2; left wrist extensors, 4; bilateral finger flexors, 2; right finger extensors, 1; left finger extensors, 2; right lower extremities, 1; left lower extremities, 0. His deep tendon reflex was decreased on the bilateral upper limb, and his bilateral patella tendon reflex showed hyperreflexia. Computed tomography showed the fracture through the right TF at C5 (Fig. 1a). Functional cervical X-ray showed no instability but slight posterior spondylolisthesis of C5. Magnetic resonance angiography (MRA) showed VA stenosis at the C5 level and wall irregularity distal of the stenotic lesion (Fig. 1c). We performed DSA and determined the necessity of embolization for VAI before direct cervical spine surgery. Right VA angiography showed no intimal flap, with only slight stenosis at the C5 level (Fig. 1d).
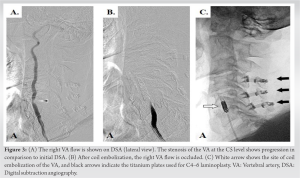
Under local anesthesia, a 6-Fr short sheath was inserted in the right brachial artery. A 4.2-Fr catheter (Hanaco Medical Co., Ltd, Saitama, Japan) was advanced into the right VA, because a 6-Fr guiding catheter could not be advanced to the right VA. The angiography of the right VA showed that the stenosis of the right VA at the C5 level had progressed in comparison to that observed on initial DSA (Fig. 3a). A Phenom 17 microcatheter (Medtronic, Dublin, Ireland) was also advanced at the C6 level of VA. Using seven AXIUM PRIME detachable coils (Medtronic, Dublin, Ireland), we achieved complete occlusion of the right VA (Fig. 3b and c). The blood supply from the left VA into the cranial region was observed to be sufficient. The patient did not experience any complications in association with endovascular treatment. After endovascular therapy, DWI shows no additional infarction.
The patient was transferred to the rehabilitation hospital 7 weeks after suffering cervical injury with a modified Rankin scale grade of 4. At that time, his MMT demonstrated a mild improvement compared to the pre-operative findings with the following scores: Right upper extremities, 3; left upper extremities, 4; and bilateral lower extremities, 3.
BVIs rarely cause VAI (VA dissections and occlusions). The incidence rate of VAI in BVI patients is reported to range from 0.24% to 2% [1-6]. It is not uncommon for VAI to be asymptomatic at the time of injury. Therefore, particularly in cervical spine fractures, vascular examinations by CTA or DSA should be performed first to confirm the presence of vascular injury [8, 9]. Delayed embolization may occur or progress, even in the absence of symptoms. Emergency physicians and spine surgeons need to be aware of this possibility. The evidence is not sufficient to support standard treatment for VAI with blunt traumatic cervical injuries. Some have suggested that antithrombotic or anticoagulant therapy is effective for patients with traumatic VAI, and it would reduce stroke rates [3, 8, 10, 11]. On the other hand, Scott et al. reported that the post-traumatic infarction rate of low-grade (Grade Ⅰ and Grade Ⅱ) injuries was as low as 1.7%, with no correlation between the stroke rate and the use of antiplatelet or anticoagulant therapy [12, 13]. Embolization of the injured VA must be performed before surgical fixation of the cervical spine to prevent subsequent embolic infarction. This is because embolic cerebrovascular ischemia can occur when the interrupted blood flow of the VA is recanalized by movement during surgical repositioning [6, 8, 14].
In the present case, we confirmed that there was no obvious dissection or stenosis of the VAs on DSA; however, post-operative MRA showed that the VA was almost occluded. The risk of VA occlusion may remain, even in patients treated with decompression surgery alone, without repositioning or fixation. The intraoperative surgical position (cervical flexion) may influence the flow of the VA and aggravate the VAI. In patients with VAI, even those without dislocation or obvious dissection, a more aggressive approach — with embolization of the VA — may be needed to prevent subsequent disorder. During follow-up, the occlusion of the VA was observed by MRA; however, the blood flow gradually began to increase on the 8th day after surgery. We performed endovascular therapy to prevent distal embolization because we considered that there was a risk of embolic infarction from the injured artery to distal regions. Because the presence of cerebral infarction was recognized on MRI obtained on day 8, we chose not to administer additional antithrombotic medications. Instead, we performed endovascular therapy as an additional treatment for recanalization VA. It remains controversial as to whether embolization of the VA should be performed in the early phase if the VAIs are unremarkable or mild (corresponding to Grade Ⅰ of the Denver grading scale). The treatment techniques for artery dissection include deconstructive (parent artery occlusion) and reconstructive (stent or flow-diverter placement) approaches. In Sӧnmez’s study of the vertebrobasilar dissecting aneurysms, both techniques were associated with high rates of good long-term neurological outcomes and similar low rates of recurrence and retreatment. Deconstructive techniques achieved higher rates of complete angiographic occlusion in comparison to reconstructive techniques; however, reconstructive techniques were associated with a lower rate of periprocedural morbidity [15]. As a matter of course, endovascular therapy itself is associated with the risk of complications. An adequate assessment of the intracranial blood flow is necessary to determine the patient’s eligibility for embolization, including whether the intracranial posterior circulation is from the contralateral side or from the collateral flow of anterior circulation, and whether the contralateral VA can also develop delayed injuries.
According to the relevant literature, prophylactic embolization may be indicated to prevent embolic infarction not only in cases of VA occlusion requiring fixation of the cervical spine but also in cases of low-grade VAI that do not require fixation [8]. The performance of embolization of the VA before spinal surgery might be an aggressive option that avoids the development of serious embolic infarction disorder after VAI.
Although VAIs in patients with blunt cervical spine injury are rare, they are a risk factor for embolic infarction. It is necessary to evaluate vascular injuries in the initial examinations. Aggressive preoperative embolization may avoid deterioration, even in cases with mild VAI who do not require spinal fixation surgery.
Pre-operative embolization may be indicated to prevent embolic infarction even in cases of low-grade asymptomatic VAI who do not require spinal fixation surgery.
References
- 1.Isaji T, Ohshima T, Nakura T, Miyachi S, Joko M, Matsuo N, et al. Efficacy of endovascular proximal occlusion before direct reposition surgery of blunt cervical fracture with unilateral vertebral injury. NMC Case Rep J 2019;6:131-4. [Google Scholar]
- 2.Miller PR, Fabian TC, Bee TK, Timmons S, Chamsuddin A, Finkle R, et al. Blunt cerebrovascular injuries: Diagnosis and treatment. J Trauma 2001;51:279-85. [Google Scholar]
- 3.Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M, et al. Prospective screening for blunt cerebrovascular injuries: Analysis of diagnostic modalities and outcomes. Ann Surg 2002;236:386-93. [Google Scholar]
- 4.Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ, et al. The devastating potential of blunt vertebral arterial injuries. Ann Surg 2000;231:672-81. [Google Scholar]
- 5.Drain JP, Weinberg DS, Ramey JS, Moore TA, Vallier HA. Indications for CT-angiography of the vertebral arteries after trauma. Spine (Phila Pa 1976) 2018;43:E520-4. [Google Scholar]
- 6.Stein DM, Boswell S, Sliker CW, Lui FY, Scalea TM. Blunt cerebrovascular injuries: Does treatment always matter? J Trauma 2009;66:132-44. [Google Scholar]
- 7.Cothren CC, Biffl WL, Moore EE, Kashuk JL, Johnson JL. Treatment for blunt cerebrovascular injuries: Equivalence of anticoagulation and antiplatelet agents. Arch Surg 2009;144:685-90. [Google Scholar]
- 8.Nakamura Y, Kusakabe K, Nakao S, Hagihara Y, Matsuoka T. Vertebral artery occlusion associated with blunt traumatic cervical spine injury. Acute Med Surg 2021;8:e670. [Google Scholar]
- 9.Brommeland T, Helseth E, Aarhus M, Moen KG, Dyrskog S, Bergholt B, et al. Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med 2018;26:90. [Google Scholar]
- 10.Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: Implications of a new grading scale. J Trauma 1999;47:845-53. [Google Scholar]
- 11.Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: A clinical review. Eur Spine J 2011;20:1405-16. [Google Scholar]
- 12.Scott WW, Sharp S, Figueroa SA, Madden CJ, Rickert KL. Clinical and radiological outcomes following traumatic grade 1 and 2 vertebral artery injuries: A 10-year retrospective analysis from a level 1 trauma center. J Neurosurg 2014;121:450-6. [Google Scholar]
- 13.Alterman DM, Heidel RE, Daley BJ, Grandas OH, Stevens SL, Goldman MH, et al. Contemporary outcomes of vertebral artery injury. J Vasc Surg 2013;57:741-6. [Google Scholar]
- 14.Indo M, Oya S, Shojima M, Inokuchi K, Yahata T, Sugiyama S, et al. Prevention of thromboembolic infarction after surgery for traumatic cervical fracture with vertebral artery occlusion by preoperative endovascular coil embolization. World Neurosurg 2019;129:e838-44. [Google Scholar]
- 15.Sönmez Ö, Brinjikji W, Murad MH, Lanzino G. Deconstructive and reconstructive techniques in treatment of vertebrobasilar dissecting aneurysms: A systematic review and meta-analysis. AJNR Am J Neuroradiol 2015;36:1293-8. [Google Scholar]