This article highlights the importance of prompt open reduction through a palmar approach in case of complex metacarpophalangeal joint dislocation in children, involving entrapment of the metacarpal head within the palmar plate.
Dr. Yoann Durand, Department of Orthopaedic Surgery and Traumatology, Centre Hospitalier Universitaire Vaudois, Rue de Bugnon 46, 1005 Lausanne, Switzerland. E-mail: yoanndurand.mail@gmail.com
Introduction: This report highlights a rare case of complex metacarpophalangeal (MCP) joint dislocation, commonly referred to as Kaplan’s lesion. This type of dislocation typically results from a hyperextension injury and requires surgical intervention as closed maneuvers are unsuccessful in reducing the dislocation. Surgical reduction for complex MCP joint dislocations is commonly done through classic volar or dorsal approaches. This report presents a case of a complex MCP joint dislocation and the surgical approach taken to address the issue.
Case Report:We present a case of a complex MCP joint dislocation in a 5-year-old male patient who sustained a hyperextension injury to his index finger. The patient underwent open reduction surgery using a volar approach due to the buttonholing of the phalangeal head through the volar plate and blockage between the flexor tendons and lumbrical muscle. Following the procedure, the joint was immobilized in a palmar splint at 30° flexion for 2 weeks before being allowed unrestricted mobilization. At the 4-week follow-up, the patient reported being pain-free and had regained nearly full range of motion in the index finger MCP joint.
Conclusion: Although there are multiple techniques to address complex MCP dislocation, the classic volar approach is still considered an effective treatment option for pediatric patients with this injury. In such cases, open reduction through a volar approach can enable surgeons to access the joint and address complex dislocations, which are often difficult to manage with closed reduction alone. Consequently, this surgical approach can help achieve a successful reduction and restore the joint’s functionality. Therefore, despite the availability of alternative approaches, the classic volar approach should still be considered as a viable option for treating complex MCP joint dislocations in the pediatric population.
Keywords: Metacarpophalangeal joint dislocation, Kaplan’s Lesion, pediatrics, case report.
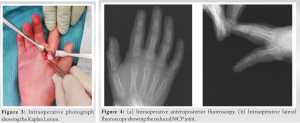
Metacarpophalangeal (MCP) joint dislocations, initially described by Kaplan in 1957, are rare injuries [1, 2] that can be categorized as simple or complex, with the latter being referred to as Kaplan’s lesion [2]. While simple volar dislocations can often be reduced through closed maneuvers, complex dislocations are complete and require surgical intervention as they are irreducible through closed maneuvers [2, 3]. The mechanism of injury typically involves hyperextension of the MCP joint, causing the metacarpal head to buttonhole through the volar plate and become blocked by the lumbrical muscles and flexor tendons (Fig. 1) [2-4]. Open surgical reduction for complex MCP joint dislocations is usually done through either the classic volar approach, as described by Kaplan, or a dorsal approach, initially introduced by Farabeuf in 1876 [5] and later popularized by Becton in 1975 [4]. Other surgical approaches, including percutaneous [6] and arthroscopic [7] methods, have also been described in the literature.
However, no superiority has been established between these approaches. Despite being a rare injury, several cases of these types of lesions, including a few pediatric cases, have been reported in the literature. This work follows the SCARE criteria [8].
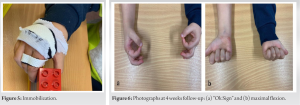
We report the case of a 5-year-old boy, brought to the emergency department after an isolated trauma of his right index during a fall of his height. The parent described a mechanism of hyperextension of his right index finger, causing a MCP joint dislocation. Conventional plain-film X-ray imaging performed in the emergency department shows a dorsal dislocation of the right index finger at that level of the MCP joint, without any fracture or osteochondral lesion (Fig. 2a and b).
During physical examination, the patient exhibited deformity of the MCP joint in the index finger, along with tenderness and swelling. There was no skin lesion, neurological and vascular examinations were normal. After several unsuccessful attempts at closed reduction under digital block anesthesia, decision was made to continue management in the operating room. The patient underwent open surgical reduction through a volar approach. Intraoperative images (Fig. 3) depicted a typical presentation of a MCP joint dislocation, consistent with the illustrations of Kaplan [1], with the metacarpal head dislocated volarly and trapped between the flexor and lumbrical tendons through the volar plate. After general anesthesia and the application of a tourniquet at the base of the arm, the dislocation was reduced through the volar approach using an elevator and subsequently, the volar plate lesion was repaired. C-arm fluoroscopy images show a reduction of the MCP joint (Fig. 4a and b).
After the surgery, the patient’s hand was immobilized in a palmar splint set at 30° of flexion for a period of 14 days. Following this initial immobilization, the patient was permitted unrestricted movement of the right hand and index finger (Fig. 5).
During the 4-week follow-up, the patient reported being pain-free with active and passive movement. Pulp to palm distance was 0 centimeter, and range of motion in the right index finger was almost fully restored compared to the uninjured side (Fig. 6a and b). At 1-year post-operative follow-up, no sign of growth disturbance was detected, and the patient had no clinical sign of MCP instability.
MCP joint dislocations are rare injuries1, much less common than PIP dislocation. The MCP joint is a synovial joint that enables flexion, extension, adduction, and abduction. MCP joint dislocations are the result of a hyperextension mechanism and can be reduced through closed maneuvers or open surgical techniques. The MCP joint is surrounded by an articular capsule with ligamentous reinforcements on all sides, as well as a volar plate on the palmar aspect. Simple dislocations may be reduced by reducing tension on the flexor tendons and applying dorsal pressure to the base of the proximal phalanx. However, distracting the joint may sometimes entrap adjacent structures and convert the dislocation into a complex one. One of the most relevant structures that hinder reduction is the volar plate, which can become trapped in a dislocated MCP joint, rendering it irreducible. In addition, the metacarpal head may penetrate through the volar soft tissues and become buttonholed. In the pediatric population, care must be taken due to the possibility of cartilage fractures and growth arrest. Children also present more lax ligamentous structures, making them more susceptible to dislocations. Open surgical reduction techniques for MCP joints include the classic volar approach, dorsal approach, and arthroscopic and percutaneous methods. The classic volar and dorsal approaches are the most frequently used and well-described techniques [4, 6, 7, 9, 10]. It should be noted that the dorsal and volar approaches present distinct advantages and disadvantages, and controversy exists about which approach is superior [11]. The dorsal approach provides easier access to the entrapped volar plate injury and a lower risk of damaging the neurovascular bundle [12]. However, it requires splitting the extensor mechanism and dorsal joint capsule, and it does not enable repair of the volar plate lesion. Moreover, it makes delayed diagnosis of dislocations of more than 3 weeks challenging due to entrapment of potential lesions of the flexor and lumbrical muscle tendons [3, 4]. The volar approach, as described by Kaplan, enables easy reduction of entrapment caused by structures other than the volar plate and allows for volar plate repair. However, its disadvantage lies in the vulnerability of the neurovascular bundles, which may become displaced anteriorly, making them more vulnerable during the approach [3, 4]. A lateral approach has also been described by Pereira et al. [13], allowing access to both dorsal and palmar structures while reducing the risk of scarring, making it useful in cases requiring the fixation of osteochondral fragments. However, the risk of neurological injury is higher than with other approaches, which therefore limits use. Regardless of the chosen approach, it is crucial that the joint reduction is performed as early as possible to minimize the risk of growth arrest, osteonecrosis, or joint stiffness [14]. In summary, while MCP joint dislocations are rare, they can be managed through various techniques. The classic volar and dorsal approaches are the most commonly used and well-described techniques. Each approach presents distinct advantages and disadvantages that must be carefully considered by the surgeon when selecting the most appropriate technique for the patient.
We recommend the classic volar approach as the preferred surgical technique for repairing MCP joint dislocations. This approach allows for better access to the volar plate and avoids dorsal structures, resulting in greater stability and facilitating early active and passive mobilization of the repaired joint. Moreover, using careful dissection and a thorough understanding of anatomy, the surgeon can protect and preserve the neurovascular bundle. Overall, the classic volar approach provides a safe and effective option for treating MCP joint dislocations while minimizing the risk of complications.
MCP dislocation requires prompt management through open reduction via palmar approach, especially in children, to reduce the risk of secondary growth arrest or osteonecrosis.
References
- 1.Sumarriva G, Cook B, Godoy G, Waldron S. Pediatric complex metacarpophalangeal joint dislocation of the index finger. Ochsner J 2018;18:398-401. [Google Scholar]
- 2.Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am 1957;39-A:1081-6. [Google Scholar]
- 3.Dinh P, Franklin A, Hutchinson B, Schnall SB, Fassola I. Metacarpophalangeal joint dislocation. J Am Acad Orthop Surg 2009;17:318-24. [Google Scholar]
- 4.Becton JL, Christian JD Jr., Goodwin HN, Jackson JG 3rd. A simplified technique for treating the complex dislocation of the index metacarpophalangeal joint. J Bone Joint Surg Am 1975;57:698-700. [Google Scholar]
- 5.Farabeuf LHF. De la luxation du pouce en arrière. Bull Soc Chir. 1876;11:21-62. [Google Scholar]
- 6.Kodama A, Itotani Y, Mizuseki T. Arthroscopic reduction of complex dorsal metacarpophalangeal dislocation of index finger. Arthrosc Tech 2014;3:e261-4. [Google Scholar]
- 7.Sodha S, Breslow GD, Chang B. Percutaneous technique for reduction of complex metacarpophalangeal dislocations. Ann Plast Surg 2004;52:562-5, discussion 566. [Google Scholar]
- 8.Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler AJ, Orgill DP, et al. The SCARE 2018 statement: Updating consensus surgical CAse REport (SCARE) Guidelines. Int J Surg 2018;60:132-6. [Google Scholar]
- 9.Light TR, Ogden JA. Complex dislocation of the index metacarpophalangeal joint in children. J Pediatr Orthop 1988;8:300-5. [Google Scholar]
- 10.Durakbasa O, Guneri B. The volar surgical approach in complex dorsal metacarpophalangeal dislocations. Injury 2009;40:657-9. [Google Scholar]
- 11.Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: A comparison of the surgical approaches. J Hand Surg Br 1988;13:466-8. [Google Scholar]
- 12.Sattari SA, Sattari AR, Heydari K, Sadat Kiaei SM, Zandrahimi F, Mohammadpour M. Dorsal approach in the surgical treatment of complex dorsal dislocation of index metacarpophalangeal joint; A case report. Arch Acad Emerg Med 2022;10:e13. [Google Scholar]
- 13.Pereira JM, Quesado M, Silva M, Carvalho JD, Nogueira H, Alves J. The lateral approach in the surgical treatment of a complex dorsal metacarpophalangeal joint dislocation of the index finger. Case Rep Orthop 2019;2019:1063829. [Google Scholar]
- 14.Rubin G, Orbach H, Rinott M, Rozen N. Complex dorsal metacarpophalangeal dislocation: Long-term follow-up. J Hand Surg Am 2016;41:e229-33. [Google Scholar]