Surgical treatment of insufficiency fractures in RA patients with bone void filler seems promising.
Dr. Rasmus Elsøe, Department of Orthopedic Trauma Surgery, Aalborg University Hospital, Aalborg University, 18-22 Hobrovej, Aalborg, 9000 Denmark. E-mail: rae@rn.dk
Introduction : The aim is to report early clinical results of an experimental surgical procedure, injecting bone void filler, for patients with lower extremity rheumatoid arthritis (RA) insufficiency fractures.
Case Report: We used a cross-sectional design with retrospective follow-up. Patient-reported outcomes were reported by the body-region specific questionnaires, knee injury and osteoarthritis outcome score (KOOS), or foot and ankle outcome score (FOAS). The Eq5D-5L questionnaire reported overall health-related quality of life (QoL). Furthermore, patient satisfaction (semi-structured interview), pain reactions, and adverse events were reported. Results from the first five patients were included. The median age was 70 years (range 50–80). Fracture localizations were proximal tibia (2), distal tibia (2), and distal femur (1). Four out of five patients reported a high degree of patient satisfaction following treatment. Four out of five patients at follow-up reported no pain from the fracture location. The median improvement from baseline to follow-up on the KOOS/FAOS subscale scores was pain 65 (range 42–69), symptoms 39 (range 25–50), the activity of daily living 41 (range 29–51), sport and recreational activities (sport/rec) 48 (range 40–60), and QoL 60 (range 57–72). The median improvement for the Eq5D index was 0.30 (range 0.26–0.36).
Conclusion: Surgical treatment of insufficiency fractures in RA patients with bone void filler seems promising. Four out of five patients reported considerable improvement in function and QoL and substantially lower pain scores following treatment. More research is needed to investigate the efficacy of this novel surgical procedure.
Keywords: Bone void filler, insufficiency fractures, surgical.
Patients diagnosed with rheumatoid arthritis (RA) often have substantial pain and disability related to the affected joints. Increased RA activity may result in articular or periarticular pain. Such pain may also be related to juxta-articular insufficiency fractures [1]. Although patients often describe a sudden onset of pain at a site without prior trauma and a different type of pain from that related to increased disease activity, symptoms may be interpreted as an increase in RA activity and treated accordingly with intraarticular steroid injections and antirheumatic medications [2]. Insufficiency fractures in RA patients are often not detectable by conventional X-ray at the onset of pain but only visualized by magnetic resource imaging (MRI), causing a delay in diagnosis [1]. Pain from insufficiency fractures may cause considerable disability and inactivity [1, 2]. Insufficiency fractures in the lower limbs are mainly located close to the knee or ankle and in the foot [1, 2]. Fractures may be at a single site but are often seen at multiple sites [1, 2]. Recurring insufficiency fractures are not uncommon [2]. Conservative treatment of these fractures is frequently prolonged as pain, intraosseous edema, and fracture healing, assessed by MRI, resolve slowly, and resulting in an extended immobilization period [2]. The etiology of the development and configuration of insufficiency fractures is not clear but is likely multifactorial [1, 2]. The resulting fracture gaps are commonly very small, and the authors speculate that this increases strain, which, by itself, will increase the risk of a prolonged healing time. Combined with the inherent reduced ability to heal the fracture due to RA and probably also the pharmacological treatment of RA, this point may be an important factor in the observed pathology [3]. To reduce strain by stabilizing the fracture site, a bone void filler may be injected. This procedure may alleviate pain and increase function because the patients are allowed full weight bearing without restrictions immediately postoperative.
We aim to report the early clinical results of an experimental surgical procedure, injecting bone void filler at the fracture site, for patients with lower extremity RA insufficiency fractures. (Fig. 1).
The study design is a case report with retrospective follow-up.
The Danish Data Protection Agency (Journal number K2023-013) approved the study, which was performed according to the principles of the Helsinki Declaration. Informed consent was obtained from all patients. The reporting of the study complies with the Strengthening the Reporting of Observational Studies in Epidemiology statement [4].
Participants
The patients were included from the Department of Orthopedic Surgery, Aalborg University Hospital, Denmark, and assessed for eligibility between March 2021 and November 2022.
A patient was eligible for treatment if he/she met the following criteria
• Above 18 years of age
• Diagnosed with RA
• Lower extremity insufficiency fractures not responding to conservative treatment, defined as no improvement in the fracture-related pain within the first 3 months after the onset of symptoms.
A patient was not eligible for treatment if he/she met any of the following criteria
• Multiple-site insufficiency fractures
• Diagnosed with conditions that cause cognitive impairment.
Intervention
After verifying RA insufficiency fractures with no response to conservative treatment, patients were offered experimental treatment with inforation and injection of Cerament VÒ, Bonesupport AB, and Sweeden. Cerament VÒ is a bone void filler consisting of hydroxyapatite, calcium sulfate, and Vancomycin. One or two small incisions were placed appropriately according to the fracture site and orientation. Large, gauged cannulas were used to inforate and inject Cerament V at the fracture site and to guide the infusion. The procedure was performed under fluoroscopy to ensure Cerament V was injected at the expected site. No immobilization was recommended postoperatively, and immediate full weight-bearing was allowed. The steps of the surgical procedure are presented in Fig. 1.
Descriptive and outcomes
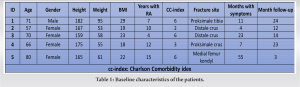
Baseline characteristics, including age, gender, height, weight, BMI, years of RA, fracture location, duration of symptoms, and months of follow-up, were collected.
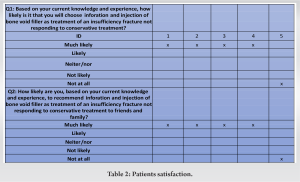
The patients’ experiences with the treatment were evaluated based on two questions:
Based on your current knowledge and experience, how likely is it that you will choose inforation and injection of bone void filler to treat an insufficiency fracture not responding to conservative treatment? This question intends to evaluate the overall patient satisfaction combined with patients’ expectations of the outcome. Based on your current knowledge and experience, how likely are you to recommend inforation and injection of bone void filler to treat an insufficiency fracture not responding to conservative treatment to friends and family? This question intends to evaluate the patients’ perceptions of to what degree inforation and injection of bone void filler can be introduced in the general population of RA patients presenting with an insufficiency fracture not responding to conservative treatment. A 5-point Likert scale was used on both questions regarding patient experience/satisfaction with the treatment. The answer scale was as follows: much likely, likely, neither/nor, not likely, and not at all likely.
Other outcome measurements
Adverse events/harms (AE): An AE was defined as any undesirable experience during follow-up. If an AE results in hospitalization, prolonged inpatient hospital care, death or re-surgery.
KOOS
The knee injury and osteoarthritis outcome score (KOOS) is a standardized patient-reported questionnaire developed to evaluate knee problems [5]. The questionnaire includes five subscales: pain, activity of daily living (ADL), symptoms, sport, and quality of life (QoL). A total score of 100 indicates no symptoms, and 0 indicates major symptoms. KOOS was used for patients with knee-related fractures. KOOS outcome before treatment and at follow-up was included in this study.
FAOS
The foot and ankle outcome score (FAOS) is a standardized patient-reported questionnaire developed to evaluate foot and ankle problems [6]. The questionnaire includes five subscales: pain, ADL, symptoms, sport, and QoL. A total score of 100 indicates no symptoms, and 0 indicates major symptoms. FAOS was used in patients with distal crus fractures. FAOS outcomes before treatment and at follow-up were included.
Eq5D-5L
Eq5D-5L is a standardized questionnaire developed to assess general health outcomes. It consists of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression, and a self-rated health scale on a 20 cm vertical, Visual Analog Scale (VAS) with endpoints labeled “the best health you can imagine” and “the worst health you can imagine.” An Eq5D-5L index of 1.0 indicated full health, and −0.59 denoted death. Eq5D outcome before treatment and at follow-up was included.
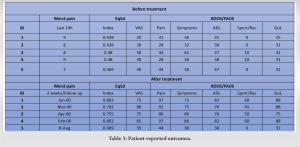
Pain reaction
The pain intensity of the fractured location was measured. Worst pain during the past 24 h and rest pain was measured on a 10 cm VAS with the endpoints “no pain” and “maximal pain.” The pain outcome was included before treatment, 2 weeks after treatment, and at follow-up.
A total of five patients were treated. The median age was 70, with a range from 56 to 80 years of age. Four patients were female. The insufficiency fracture localizations were proximal tibia (2), distal tibia (2), and distal femur (1). High pain intensity and low scores in the KOOS/FAOS and Eq5d-5L questionnaires were observed before treatment. Detailed baseline characteristics of individual patients are presented in Table 1.
Patient experiences
Four out of five patients reported much likelihood on the two questions regarding the patients’ perceptions indicating that bone filler may be feasible in treating insufficiency fractures.
One patient reported not likely on the two questions regarding patients’ perceptions. Detailed outcome results divided by individual patients are presented in Table 2.
AE
No AE or serious AE were observed during the study.
Pain reactions and patient-reported outcomes
Two weeks after treatment and at the final follow-up, four of the five patients reported considerably better KOOS/FAOS and Eq5D-5L scores and substantially lower pain scores than the baseline. Detailed results divided by individual patients are presented in Table 3.
The median improvement from baseline to follow-up on the KOOS/FAOS subscale scores are pain 65 (range 42–69), symptoms 39 (range 25–50), ADL 41 (range 29–51), sport and recreational activities (sport/rec) 48 (range 40–60), and QoL 60 (range 57–72). The median improvement for the Eq5D index was 0.30 (range 0.26–0.36).
We reported early clinical results of an experimental and novel surgical procedure for insufficiency fractures in not responding to conservative treatment in RA patients. Four out of five patients reported considerable improvement in the KOOS/FAOS/Eq5D scores and reported substantially lower pain scores than the baseline. Four out of five patients reported a high degree of satisfaction with the surgical treatment. One patient experienced no improvement following treatment and was thus not satisfied. Surgical treatment with bone void filler for rheumatoid insufficiency fractures may advance the current treatment and improve patient satisfaction. The five patients reported on in this study were all open to individual experimental treatment due to prolonged pain with no improvement in pain and function following conservative treatment. Due to the treatment’s surprising and substantial impact on function, QoL, and pain scores, the authors believe that it is time to report early clinical results from the first five patients treated before initiating a formal study to inform the public and facilitate further research. Four out of the five patients reported much likelihood on the two questions regarding the patient’s perception of the treatment, indicating a high degree of patient satisfaction with the experimental surgical procedure. At the final follow-up (range 3–24 months), four out of five patients reported no pain from the fracture location.
Four out of five patients reported considerably better patient-reported scores following the surgical treatment. The median improvement on the body-region-specific KOOS/FAOS subscale scores ranged from 39 in symptoms to 65 in pain. KOOS thresholds for clinically relevant improvement range from 8 to 18 [7-10]. FAOS thresholds for clinically relevant improvement range from 5 to 22 points [11-14]. Results indicated a considerable improvement compared to baseline status. A comparable result was observed for the generic Eq5D index score with a median improvement of 0.30 (range 0.26–0.36). Clinically relevant improvement for the Eq5d in rheumatoid arthritis patients is reported to be 0.06–0.20, indicating a clinically relevant improvement from baseline to follow-up [15]. At the 2-week follow-up, four out of five patients experienced substantial improvement in function and lower pain scores compared to baseline. However, the median duration of symptoms and pain before treatment was 23 months. The authors speculate that the inforation and injection of a bone void filler at the insufficiency fracture site may have reduced the strain by bridging the fracture gap and reducing the motion across the fracture. The bone void filler may also act as a bone-conducting agent promoting fracture healing after stabilizing the fracture site. This may have been a factor in alleviating pain and increasing the ability to ambulate postoperatively. However, the medium- to long-term effects on all parameters and the effects on final bone healing are unknown. One of the five patients experienced no improvement following treatment and was thus not satisfied. At follow-up, comparable results to baseline status were observed for the pain scores and the patient-reported outcomes. Regarding the two questions about satisfaction, the patient reported: “not likely.” The patient was an 80-year-old woman with an insufficiency fracture localized to the left medial femur condyle. The surgical procedure was performed without complications. A secondary MRI scan of the lower extremity was performed. It showed early changes compatible with insufficiency fractures localized to the left proximal tibia and calcaneus, which likely may have influenced the result of treatment. Simultaneous multiple sites of insufficiency fractures are well known, indicating the significance of entire lower extremity MRI scans in evaluating patients before surgery [2]. Today’s conservative approach to the treatment of insufficiency fractures, including prolonged periods of pain and immobilization, has been without real advancement in recent years and comes with considerable morbidity in an already challenged patient group. Insufficiency fractures may be treated only by drilling, decreasing the strain at the fracture site. However, the proposed treatment with bone void filler is a minimally invasive surgical procedure and may potentially advance clinical practice and patient satisfaction. The procedure may alleviate pain and increase or maintain function as the patients are allowed full weight bearing without restrictions immediately postoperative. We used a bone void filler with antibiotics (vancomycin) to decrease the risk of local infection. Still, the optimal properties of a bone void filler are currently unknown for this treatment.
Surgical treatment with bone void filler for insufficiency fractures in RA patients seems promising. A high degree of patient satisfaction with the surgical procedure was observed. Four out of five patients reported considerable improvement in function and QoL and substantially lower pain scores following treatment. More research is needed to investigate the efficacy of this novel surgical procedure, and further development of the procedure may be warranted.
We report early clinical results of the first five patients treated, and no efficacy testing is possible. The observed improvement in pain scores and patient-reported outcomes compared to baseline status for four out of five patients was unexpectedly high and seems promising. However, these data is the first clinical result of an experimental surgical procedure aiming to treat rheumatoid arthritis insufficiency fractures. More research is needed to investigate efficacy before introducing the treatment in clinical practice. Such research may include an adequately powered randomized controlled trial (RCT) to control bias and confounding and deliver effect size for the different patient groups. The present study’s results may inform a future large-scale RCT study.
References
- 1.Yurtsever A, Fagerberg SK, Rasmussen C. Insufficiency fractures of the knee, ankle, and foot in rheumatoid arthritis: A case series and case-control study. Eur J Rheumatol 2020;7:124-9. [Google Scholar]
- 2.Mäenpää HM, Soini I, Lehto MU, Belt EA. Insufficiency fractures in patients with chronic inflammatory joint diseases. Clin Exp Rheumatol 2002;20:77-9. [Google Scholar]
- 3.Claes L, Recknagel S, Ignatius A. Fracture healing under healthy and inflammatory conditions. Nat Rev Rheumatol 2012;8:133-43. [Google Scholar]
- 4.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Google Scholar]
- 5.KOOS/KOOS-12 Questionnaries [KOOS Web Site]. Available from: https://www.koos.nu [Last accessed on 2021 Jun 12]. [Google Scholar]
- 6.Faos. FOAS Questionnary [FAOS Web Site]; 2008. Available from: https://www.koos.nu [Last accessed on 2014 Jun 11]. [Google Scholar]
- 7.Lyman S, Lee YY, McLawhorn AS, Islam W, MacLean CH. What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop Relat Res 2018;476:2432-41. [Google Scholar]
- 8.Kuo AC, Giori NJ, Bowe TR, Manfredi L, Lalani NF, Nordin DA, et al. Comparing methods to determine the minimal clinically important differences in patient-reported outcome measures for veterans undergoing elective total hip or knee arthroplasty in veterans health administration hospitals. JAMA Surg 2020;155:404-11. [Google Scholar]
- 9.Soh SE, Harris IA, Cashman K, Heath E, Lorimer M, Graves SE, et al. Minimal clinically important changes in HOOS-12 and KOOS-12 scores following joint replacement. J Bone Joint Surg Am 2022;104:980-7. [Google Scholar]
- 10.Eckhard L, Munir S, Wood D, Talbot S, Brighton R, Walter WL, et al. Minimal important change and minimum clinically important difference values of the KOOS-12 after total knee arthroplasty. Knee 2021;29:541-6. [Google Scholar]
- 11.Sierevelt IN, van Eekeren IC, Haverkamp D, Reilingh ML, Terwee CB, Kerkhoffs GM. Evaluation of the dutch version of the foot and ankle outcome score (FAOS): Responsiveness and minimally important change. Knee Surg Sports Traumatol Arthrosc 2016;24:1339-47. [Google Scholar]
- 12.Larsen P, Al-Bayati M, Elsøe R. The foot and ankle outcome score (FAOS) during early recovery after ankle fracture. Foot Ankle Int 2021;42:1179-84. [Google Scholar]
- 13.Tapaninaho K, Uimonen MM, Saarinen AJ, Repo JP. Minimal important change for foot and ankle outcome score (FAOS). Foot Ankle Surg 2022;28:44-8. [Google Scholar]
- 14.Desai S, Peterson AC, Wing K, Younger A, Crump T, Liu G, et al. Minimally important difference in the foot and ankle outcome score among patients undergoing hallux valgus surgery. Foot Ankle Int 2019;40:694-701. [Google Scholar]
- 15.Kitchen H, Hansen BB, Abetz L, Hojbjerre, L, Strandber-Larsen M. Patient-reported outcome measures for rheumatoid arthritis: Minimal important differences review. Arthritis Rheum 2013;65:965. [Google Scholar]