Fibular grafts have a high degree of versatility and are simpler than other complex procedures which address poor mechanics and biology in atypical femoral neck fractures.
Dr. Nicholas C Uren, Department of Orthopaedics, Southampton General Hospital, University of Southampton, Southampton, United Kingdom. E-mail: nu1g17@soton.ac.uk
Background: Neck of femur fractures (NOF) in younger adults are often treated by head-preserving fixation procedures. Non-union is an infrequent but troublesome complication following internal fixation, especially in atypical presentations. Vascularized (VFG) and non-VFG (NVFG) fibular grafting and realignment procedures have been described as an adjunct to internal fixation. Reports are rare regarding the versatility of fibular grafts, their use, and their outcomes in the United Kingdom.
Case Report: We present three complex NOF cases performed in the United Kingdom. One case is a 29-year-old Asian female treated with NVFG for a pathological transverse NOF fracture secondary to fibrous dysplasia. One case is a non-union following failed surgical management and revised using NVFG and dynamic hip screws. The last case is a VFG in a complex non-union intra-capsular fracture following conservative management in a 17-year-old male. Certain patient characteristics are described which make joint preserving surgery more attractive. All fractures united with no revisions at the time of final follow-up. Distinctions between the use of VFG and NVFG grafts are discussed.
Conclusion: This case series demonstrates the important versatility of fibular grafting and how its properties are used in different cases. Fibular grafting is an effective technique in pathological, non-union, and late-presenting NOF. Both types of grafts introduce additional biology for difficult cases where neck resorption and adequate fixation are an issue, with NVFG grafts much easier to perform.
Keywords: Neck of femur fractures, non-union, bone graft, vascularized fibular grafts, non-vascularized fibular grafts.
Neck of femur fractures (NOF) in young adults are uncommon and are usually due to high-energy trauma [1]. Fracture fixation is the mainstay of management aiming at joint preservation to avoid the increased risk of complications associated with arthroplasty at a young age [2]. NOF fracture fixation has been associated with a high risk of non-union [3]. The management of these non-unions is difficult and controversial. Hip preserving procedures are directed toward improving the biology and the mechanics to allow for healing. They can be broadly divided into bone grafting, realignment, or combined realignment and grafting procedures. Fibular grafts are the most common graft and can be either vascularized (VFG) or non-VFG (NVFG) [4]. NVBG was predominately used until the development of microsurgical techniques [5]. The effectiveness of fibular grafts is well demonstrated in Asia and other countries in the developing world, and although NVFG use has been reported in Western Europe, this simple procedure does not appear to be as widely adopted. This case series documents the use of fibular grafts in three difficult NOFs. Each case highlights factors which add to the complexity of fixation, documents differing indications for fibular grafting, and highlights the factors aiding in the decision-making between utilizing VFG and NVFG.
Case one: Pathological NOF fracture in a 29 years old with fibrous dysplasia
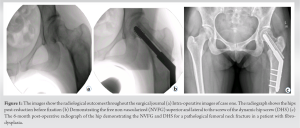
A 29-year-old female of Asian descent presented, reporting that her hip gave way first with an audible crack. Radiological examination revealed a pathological fracture through a large lytic lesion in the femoral neck (Fig. 1a). The available cancellous bone in the femoral head and neck was diminished with concerns about achieving adequate fixation with fixation devices alone. Fixation was performed using a dynamic hip screw (DHS) and NVFG (Fig. 1b). Fibrous dysplasia was confirmed by histopathological examination. At her 6-month follow-up, she denied any hip pain at any stage postoperatively and was ambulating normally. There was a small patch of improving numbness around the lateral forefoot related to fibular harvest, probably because of stretching the superficial peroneal nerve, with normal foot function. Radiological appearance at 6 months was reassuring (Fig. 1c). The new Oxford hip score (OHS) at her 1-year follow-up was 48 indicating satisfactory joint function, and post her 1-year follow-up appointment she has been advised that she can re-start high-impact activities.
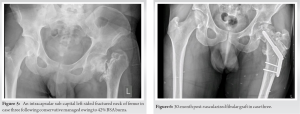
Case two: Non-union of a NOF fracture following cannulated screw fixation in a 59-year-old drinker and smoker. A 59-year-old Caucasian lady re-presented to the clinic 6 weeks following cannulated screw fixation for a left NOF. She had increasing severe pain and was struggling to mobilize. The patient was known to be a heavy smoker and drinker who did not comply with cessation advice. She had returned prematurely to full weight bearing. X-rays confirmed no evidence of healing, with further collapse of the fracture and backing out of the cannulated screws (Fig. 2). Given the radiological appearance and degree of pain, refixation and grafting versus total hip replacement were considered. Due to her substance history and age, she was considered at an increased risk for arthroplasty. A revision of the fixation with a DHS and a NVFG was therefore performed (Fig. 3). She recovered good function and was able to mobilize. Her OHS at 9 years postoperatively was 43 which indicates satisfactory joint function. Radiological appearance at 13 years postoperatively (Fig. 4) shows evidence of delayed avascular necrosis with minimal arthritic change, and the corresponding new OHS at this point was 19. She is consequently due to be seen in clinic at age 73.
Case three: Non-union of an intracapsular NOF fracture in a 17-year-old boy suffering severe extensive full-thickness burns. A 17-year-old boy sustained a left NOF secondary to an explosion on a speed boat and suffered an inhalational injury with associated third-degree burns to 42% of his body, including the trochanteric and gluteal regions of left hip, which required extensive skin grafting over many months. Owing to the extent and location of his burns, the fractured NOF was managed conservatively (Fig. 5).
After 9 months, he was referred with hip pain and 5 cm of leg shortening, presenting in a wheelchair. He was still smoking and used cannabis. His X-rays showed a displaced left intracapsular NOF fracture with severe proximal migration of distal fragment, femoral neck resorption, and a sclerotic fracture site. A pre-operative magnetic resonance imaging scan confirmed femoral head viability. A discussion with plastic surgeons took place about providing a VFG, which had theoretical advantages in his case due to the delivery of potentially more vascularity to the dense scarring and sclerosis around the hip. The femoral head was reduced through an open approach in combination with traction. The VFG was guided up a channel created by a DHS reamer, taking care to maintain the vessels which were plumbed through microsurgical techniques to the descending branches of the lateral circumflex vessels. An inferior, parallel DHS lag screw was then inserted, with surgery completed after 6 h.
Postoperatively, the wounds healed well, and the patient was instructed to toe-touch weight bear. The first post-operative X-rays demonstrated maintenance of a satisfactory position, yet no callus formation. At the 18-month follow-up, the patient was progressing well. He could walk unaided, however, occasionally experienced lateral groin pain when walking a significant distance. On examination, he was Trendelenburg negative on the left side and almost equal in leg length with optimal abductor function. Additionally, his non-arthritic hip score at 2 years was 82.5/100. His X-rays at 30 months demonstrated no displacement of the fracture or the implants and no signs of loosening around the DHS screw and the VFG (Fig. 6). Considering the starting point, this case is an excellent functional outcome.
The treatment of NOF fractures in young adults is centered around joint preservation. This case series documents the indication for the use of fibular grafts as an adjunct to fixation and presents their follow-up. At our institute, there is no pre-defined protocol for deciding between VFG and NVFG grafts, and owing to surgical difficulty and patient complexity in this series, this study provides insight into the surgical rationale regarding fibular grafting and the choice between VFG and NVFG grafts in turn demonstrating the adaptability of grafting. NOF fixation has a non-union rate reported between 10 and 33% [3, 6]. This can be mitigated in the elderly by offering them joint replacement surgery, which is a valid approach as the lifetime risk for revision (LTRR) is as low as 5% for patients aged 70 and above [2, 7]. This does not apply to young adults where higher LTRR has been reported, with one series reporting only 63% of replacements survived 10 years [8]. Additionally, younger adults are typically more active and are likely to engage in higher levels of activity pushing the limit of stability and durability. Certain traits such as drug or alcohol dependence and smoking place them at additional risk. This explains why every attempt should be made to preserve the native hip in intracapsular NOF fractures. In atypical presentations such as pathological fractures, non-unions, and delayed presentations, the risk of non-union increases with fixation alone, and adjuncts to fixation centered around improving the mechanics and the biology should be considered [9]. Cases one and two demonstrate the use of NVFG. From a mechanical perspective, as an adjunct to the DHS, the fibula acts as a strut graft resisting the varus moment created by the body weight and sharing the load with the fixed angle device. The triangular cross-section of fibula has “void filling” and anti-rotational properties as it engages the lateral femoral cortex and the femoral head. From a biological perspective, the graft provides a scaffold for osteo-condition and osteo-induction and in its vascularized form provides osteogenic cells. The first case describes the use of NVFG in pathological fractures. The principal issue in this case was mainly biological due to the absence of cancellous bone and marrow, with no angular or translational deformities in the proximal femur. The cancellous bone was replaced by fibrous tissue impairing osteo-conduction, osteo-induction, and osteogenesis. Internal fixation alone without grafting as well as a combination of osteotomies, grafting, and cancellous screws have previously been suggested [10, 11]. The senior author opted for the use of NVFG, which provided a “void filler” and supplemental side support for the DHS screw. The functional outcome has been excellent, and she remains under review.
The second case documents the use of NVFG to address non-unions. The choice for fibular grafting in this case differs from the first, in the sense that there is adequate biology in the femoral neck, but fracture stability required for healing was considered more of an issue with concerns regarding excess alcohol intake and history of falls. A fixed angle device in addition to NVFG not only increases resistance to varus collapse but imparts additional resistance to rotary and translational forces, preventing collapse at the fracture site. It is important to note osteonecrosis was identified at 13-year follow-up, and her most recent OHS was 19. She may now require further intervention, however, since she is now in her middle 70s, her corresponding LTRR will be much lower than if replacement surgery was performed in her 50s. Additionally, the lack of re-orientation osteotomies helps the arthroplasty surgeon in correctly inserting the implant. The last case details the use of VFG. It is questionable whether VFGs have any advantage over NVFG. NVFG has been shown to have acceptable union rates when used for the reconstruction of bone defects. Previous literature reports a 70% hypertrophy rate in NVFG, indicating that the graft is biologically active [12]. This strengthens the argument to use NVFG rather than the more complex and time-consuming VFG. Allsopp et al., conducted a systematic review that showed a higher risk of complications that require a surgical revision with VFG without increasing union rates or time to union compared to non-vascularized grafts [4]. Nonetheless, studies report good outcomes with VFG in intracapsular NOF fractures with success ranging between 77% and 91% [5, 13]. The patient’s age, delayed presentation, the proximal migration of the distal fragment, fracture gap, neck resorption, and the sclerosed fracture ends all contributed in the decision to involve the microsurgery team. This case is an example where biology and mechanics were unfavorable and the stability and osteogenic cells from the VFG graft were used to attempt to optimize outcomes. From a dismal starting point, with a delayed presenting severe intra-capsular fracture and extensive injuries, this case shows a vast functional improvement. There are other procedures including realignment procedures which address poor mechanics. Ideally, these aim to realign the hip so that the body weight vector is perpendicular to the fracture site, converting shear into a compression force. Varghese et al. reported a 91% union rate following a valgus femoral osteotomy in 40 patients [14]. Combined realignment and bone grafting procedures also report good outcomes, with Gadegone et al. reporting a 95% union rate for a combined valgus osteotomy and fibular strut grafting in 41 patients [15]. However, the osteotomy can come with a price. It increases the joint reaction force and can result in premature osteoarthritis. These procedures are also more complex than fibular grafts in their simplest forms. Additionally, if the realignment procedure is unsuccessful, it leaves the hip worse off than the starting point and affects the arthroplasty surgeons’ ability to correctly insert the implants.
Management of atypical intracapsular NOF fractures is difficult and controversial. The treatment should be tailored to every case. As demonstrated in this case series, there is no one-size-fits-all all solution. This study outlines the versatility of fibular grafting as an adjunct to fixation with a fixed-angle device to improve both mechanics and biology, including in pathological fractures, non-unions, and delayed presentations. VFG grafts are more complex and have a more limited indication as highlighted in this series. The use of fibular grafts yields good functional outcomes which are comparable to more complex procedures.
Every attempt should be made to preserve the native hip in intracapsular NOF fractures in young adults. Atypical presentations can add to the complexity of fracture fixation. Fibular grafts are simpler than other complex procedures which address poor mechanics and have a high degree of versatility.
References
- 1.Protzman RR, Burkhalter WE. Femoral-neck fractures in young adults. J Bone Joint Surg Am 1976;58:689-95. [Google Scholar]
- 2.Nugent M, Young SW, Frampton CM, Hooper GJ. The lifetime risk of revision following total hip arthroplasty. Bone Joint J 2021;103-B:479-85. [Google Scholar]
- 3.Karagas MR, Lu-Yao GL, Barrett JA, Beach ML, Baron JA. Heterogeneity of hip fracture: Age, race, sex, and geographic patterns of femoral neck and trochanteric fractures among the US elderly. Am J Epidemiol 1996;143:677-82. [Google Scholar]
- 4.Allsopp BJ, Hunter-Smith DJ, Rozen WM. Vascularized versus nonvascularized bone grafts: What is the evidence? Clin Orthop Relat Res 2016;474:1319-27. [Google Scholar]
- 5.LeCroy CM, Rizzo M, Gunneson EE, Urbaniak JR. Free vascularized fibular bone grafting in the management of femoral neck nonunion in patients younger than fifty years. J Orthop Trauma 2002;16:464-72. [Google Scholar]
- 6.Crawfurd EJ, Emery RJ, Hansell DM, Phelan M, Andrews BG. Capsular distension and intracapsular pressure in subcapital fractures of the femur. J Bone Joint Surg Br 1988;70:195-8. [Google Scholar]
- 7.Schreurs BW, Hannink G. Total joint arthroplasty in younger patients: Heading for trouble? Lancet 2017;389:1374-5. [Google Scholar]
- 8.Lee PT, Lakstein DL, Lozano B, Safir O, Backstein J, Gross AE. Mid-to long-term results of revision total hip replacement in patients aged 50 years or younger. Bone Joint J 2014;96-B:1047-51. [Google Scholar]
- 9.Papakostidis C, Panagiotopoulos A, Piccioli A, Giannoudis PV. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury 2015;46:459-66. [Google Scholar]
- 10.Ebeid WA, Hasan BZ, Mesregah MK. Management of fibrous dysplasia of proximal femur by internal fixation without grafting: A retrospective study of 19 patients. J Am Acad Orthop Surg Glob Res Rev 2018;2:e057. [Google Scholar]
- 11.Kataria H, Sharma N, Kanojia RK. One-stage osteotomy and fixation using a long proximal femoral nail and fibular graft to correct a severe shepherd's crook deformity in a patient with fibrous dysplasia: A case report. J Orthop Surg (Hong Kong) 2009;17:245-7. [Google Scholar]
- 12.Mueller ME. The intertrochanteric osteotomy and pseudarthrosis of the femoral neck. 1957. Clin Orthop Relat Res 1999;363:5-8 [Google Scholar]
- 13.Krieg AH, Hefti F. Reconstruction with non-vascularised fibular grafts after resection of bone tumours. J Bone Joint Surg Br 2007;89:215-21. [Google Scholar]
- 14.Varghese VD, Boopalan PR, Titus VT, Oommen AT, Jepegnanam TS. Indices affecting outcome of neglected femoral neck fractures after valgus intertrochanteric osteotomy. J Orthop Trauma 2014;28:410-6. [Google Scholar]
- 15.Gadegone WM, Ramteke AA, Lokhande V, Salphade Y. Valgus intertrochanteric osteotomy and fibular strut graft in the management of neglected femoral neck fracture. Injury 2013;44:763-8. [Google Scholar]