Removal of periaortic pedicle screw, even without a frank vascular wall breech, should be carried out with a multidisciplinary team including vascular surgeons, radiology, and the anesthetic teams on standby to ensure a successful outcome.
Dr. Athanasios I. Tsirikos, Consultant Orthopaedic and Spine Surgeon, Honorary Clinical Senior Lecturer-University of Edinburgh, Scottish National Spine Deformity Centre, Royal Hospital for Children and Young People, 50 Little France Crescent, Edinburgh Bioquarter, EH16 4TJ, UK. E-mail: atsirikos@hotmail.com;
Introduction: Vascular injury due to direct contact with malpositioned pedicle screws is perhaps the most devastating complication associated with screw instrumentation. While frank perforation of major vessels warrants urgent open or endovascular repair, the management of pedicle screws in close vicinity of large vessels is unclear. We present a systematic multi-disciplinary approach to manage a patient with a periaortic pedicle screw.
Case Report: A 20-year-old female underwent posterior scoliosis correction and spinal fusion for an adult thoracic scoliosis with spinal instrumentation extending from T3-T12. In the immediate post-operative period, an episode of acute desaturation prompted a computed tomography pulmonary angiography (CTPA) to rule out pulmonary embolism. While CTPA demonstrated an enlarged right side of the heart (corresponding to a large atrial septal defect as evident on 2D-ECHO), an incidental lateral breech at the left T10 pedicle screw level was also identified with the screw tip in close proximity to the aorta. At this time, cardiac management was prioritized and a successful atrial septal defect repair procedure was performed. After recovery from the cardiac procedure, a plan was formulated with a multidisciplinary team to remove the pedicle screw. To determine the exact position of the screw tip in relation to the aorta, an angiogram and an intravascular ultrasound were done which showed no evidence of intra-luminal extension of the screw tip. In addition, a transesophageal ultrasound was performed and this ruled out any extra-luminal contact with the aorta. Subsequently, the spinal instrumentation was removed safely with the vascular surgeon and interventional radiologist being on standby.
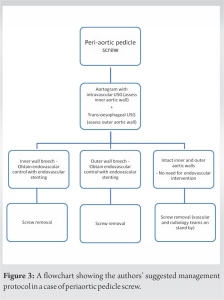
Conclusion:The authors suggest the removal of spinal pedicle screws in proximity to major vessels and describe an algorithm for this. Thorough pre-operative planning and detailed vascular imaging, as well as a multidisciplinary approach resulting in a clear surgical plan are critical to allow safe removal of such implants.
Keywords: Periaortic pedicle screw, scoliosis, vascular injury.
Posterior spinal instrumentation is the most common form of spinal fixation used during scoliosis correction. Although it is a robust fixation technique and provides 3-column vertebral stabilization, it carries a risk of serious complications primarily due to pedicle screw misplacement. Vascular injury due to direct contact with a pedicle screw that breaches the vertebral cortex is perhaps the most devastating complication and this is often associated with significant morbidity and potential mortality. While frank perforation of major vessels warrants urgent open or endovascular repair, the management of pedicle screws in close vicinity of large vessels is unclear. We present a systematic multi-disciplinary approach to manage a patient with a periaortic pedicle screw.
A 20-year-old female underwent deformity correction and spinal fusion surgery for presumed adult idiopathic scoliosis with posterior spinal instrumentation comprising pedicle screws and hooks extending from T3-T12 (Fig. 1). The pre-operative assessment including an ECG did not demonstrate any abnormalities and her past medical history was uneventful while she had a normal level of physical activities including sports. The anesthetic and scoliosis surgery was uncomplicated with the patient maintaining good O2 levels and blood pressure while the intraoperative neuromonitoring showed stable motor and sensory potentials throughout. Her initial post-operative course was without incident until post-operative day 2 when she had episodes of acute de-saturation which prompted USG Doppler for bilateral lower limbs and computed tomography pulmonary angiography (CTPA). While both the studies ruled out any evidence of pulmonary embolism, CTPA revealed right heart strain pattern and an enlarged right side of the heart. A subsequent 2D echocardiography revealed a large atrial septal defect (ASD) which had remained asymptomatic up to that point. In addition, the CTPA demonstrated a lateral breech at the left T10 pedicle screw level with the screw tip being in close proximity to the aorta. A multidisciplinary team meeting was held where it was decided to prioritize cardiac management for ASD and keep the malpositioned screw under observation with removal planned for a later date. An ASD repair procedure was performed and this was uneventful with the patient making a good recovery.
After recovery from the cardiac procedure, a repeat computed tomography (CT) scan was performed to plan removal of the screw; the CT scan showed the position of the left T10 screw in close vicinity of the aorta (Fig. 2). To determine the exact position of the screw tip in relation to the aorta, an angiogram and an intravascular ultrasound was done which showed no evidence of intra-luminal extension of the screw tip. In addition, a transesophageal ultrasound was performed and this ruled out any extra-luminal contact with the aorta. Two years following the primary scoliosis correction, it was decided to proceed with removal of the spinal instrumentation with the vascular surgeon and intervention radiologists being on standby. The midline longitudinal scar was reopened and the spine was exposed across the previously operated segments from T3-T12. A solid posterior spinal fusion was noted across the previously operated levels which allowed the spinal instrumentation to be removed without compromising the surgical outcome of scoliosis correction. Intraoperative neuro-monitoring was used and the procedure was uncomplicated. The fusion mass was re-grafted using allograft bone. The patient was followed in our clinic for an additional period of two years during which there was no clinical or radiographic evidence of scoliosis recurrence.
Posterior spinal instrumentation using pedicle screws is the most common implant technique employed during scoliosis correction. However, this common and effective procedure is not without complications. Although rare (reported incidence of 0–0.05%), a vascular injury is the most catastrophic complication of spinal instrumentation [1]. The close proximity of the large vessels (aorta, vena cava, and renal vessels) to the spine puts the patients at risk of injury due to misplacement or long-sized pedicle screws [2, 3]. Clinical presentation of implant-related vascular complications can vary from life-threatening hemorrhage resulting from frank vascular perforation to incidentally discovered asymptomatic screws with the screw tips in close vicinity or abutting the large vessels. While the former scenario requires an immediate open or endovascular repair, management of the latter poses a dilemma whether to remove the screw or adopt an observational approach with serial imaging.
The authors favor a more proactive approach based on evidence from a number of case reports with delayed presentations by the impinging instrumentation [4-7]. Authors’ preferred management protocol for managing pariaortic screws is outlined in Fig. 3. The risks associated with delayed presentations of peri-vascular screws include delayed mediastinal or retro-peritoneal hemorrhage, pseudo-aneurysm formation or thrombo-embolic complications [4, 8]. Animal studies have shown evidence of significant wall thinning and decreased stress to failure in 96% of impinged aortic specimens [9]. Nevertheless, the majority of patients with misplaced screws close to the aorta is either silent and discovered incidentally or present with subtle signs such as pulsatile abdominal pain, deep-seated chest pain, or asymmetric distal pulsations [7, 8]. The authors discovered the impinging pedicle screw in a post-operative CT scan done for a different indication. Pre-operative planning and careful preparation are of paramount importance when scheduling the removal of the malpositioned implant. We followed a multi-disciplinary team approach with input from an interventional radiologist, a vascular surgeon and a cardiac anesthetist who contributed to the peri-operative plan for screw removal. Although CT scan is an essential investigation to identify the site and level of the offending screw, metal artefacts limit the knowledge of the exact position of the screw tip in relation to the wall of the aorta. In the current patient, the integrity of the inner and outer aortic walls was ascertained with the help of an intra-luminal ultrasound performed by the radiologist and a transesophageal ultrasound performed by the cardiac anesthetist. The treatment in the majority of cases in the literature comprises removing the misplaced instrumentation and simultaneous open or endovascular aortic repair in the presence of a vascular injury. While this approach is safe and effective, placing a graft in the aorta is not without complications with the incidence of these complications increasing with longer follow-up [10]. In agreement with the vascular surgeons, the authors avoided any intra-vascular intervention as there was no evidence of contact between the pedicle screw and the outer wall of the aorta. Nonetheless, the vascular and the radiology teams were on standby throughout the length of the procedure in the case of an acute aortic rupture that would require urgent treatment. The timing of screw removal after the index surgery was essential as the spinal fusion was already achieved which allowed the removal of the instrumentation without affecting the result of scoliosis correction. No recurrence of the deformity was noted at 2-year follow-up after removing the spinal implants.
Authors suggest the removal of spinal pedicle screws in close proximity to the major vessels. Thorough pre-operative planning and detailed vascular imaging, as well as a multidisciplinary approach resulting in a clear surgical plan, are critical to allow safe removal of such implants.
This case report emphasizes on the importance of the removal of the pedicle screw in close proximity to the large vessels to avoid long-term complications and a systematic approach with support from vascular surgeons, radiologists, and anesthetists to achieve a favorable outcome.
References
- 1.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine 2010;35:E465-70. [Google Scholar]
- 2.Kakkos SK, Shepard AD. Delayed presentation of aortic injury by pedicle screws: Report of two cases and review of the literature. J Vasc Surg 2008;47:1074-82. [Google Scholar]
- 3.Decker S, Omar M, Krettek C, Müller CW. Elective thoracotomy for pedicle screw removal to prevent severe aortic bleeding. World J Clin Cases 2014;2:100-3. [Google Scholar]
- 4.Kayacı S, Cakir T, Dolgun M, Cakir E, Bozok S, Temiz C, et al. Aortic injury by thoracic pedicle screw. When is aortic repair required? literature review and three new cases. World Neurosurg 2019;128:216-24. [Google Scholar]
- 5.Levy HA, Pinter ZW, Hobson SL, Yaszemski MJ. Delayed open treatment of aortic penetration by a thoracic pedicle screw: Illustrative case. J Neurosurg Case Lessons 2023;5:CASE22533. [Google Scholar]
- 6.Wegener B, Birkenmaier C, Fottner A, Jansson V, Dürr HR. Delayed perforation of the aorta by a thoracic pedicle screw. Eur Spine J 2008;17:351-4. [Google Scholar]
- 7.Potter MQ, Lawrence BD, Kinikini DV, Brodke DS. Periaortic pedicle screw removal with endovascular control of the aorta and intraoperative aortography: A case report and review of the literature. Evid-Based Spine-Care J 2013;4:149-53. [Google Scholar]
- 8.Choi JB, Han JO, Jeong JW. False aneurysm of the thoracic aorta associated with an aorto-chest wall fistula after spinal instrumentation. J Trauma 2001;50:140-3. [Google Scholar]
- 9.Faro FD, Farnsworth CL, Shapiro GS, Mohamad F, White KK, Breisch E, et al. Thoracic vertebral screw impingement on the aorta in an in vivo bovine model. Spine 2005;30:2406-13. [Google Scholar]
- 10.Quinney BE, Parmar GM, Nagre SB, Patterson M, Passman MA, Taylor S, et al. Long-term single institution comparison of endovascular aneurysm repair and open aortic aneurysm repair. J Vasc Surg 2011;54:1592-7; discussion 1597-8. [Google Scholar]