Two distinct surgical procedures were used in a rare bilateral talus fracture scenario: open reduction and internal fixation with a cannulated cancellous screw, and percutaneous fixation with a CC screw after closed reduction, both of which resulted in comparable outcomes.
Dr. Niranjan Sunil Ghag, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: niranjanghag95@gmail.com
IntroductionBilateral talar fracture dislocations with concomitant medial malleolus fractures are rare and present complex challenges.
Case Report: We present a case study of a 30-year-old male painter who sustained these injuries following a significant fall. The surgical intervention included open reduction and internal fixation with a cannulated cancellous screw on one side and percutaneous fixation after closed reduction on the other.
Conclusion: The patient’s 3-year follow-up revealed excellent ankle function and minimal avascular necrosis changes, demonstrating the importance of well-planned delayed therapy over hasty acute procedures. Remarkably, both approaches yielded comparable and favorable outcomes, emphasizing the importance of surgical planning, soft-tissue management, and the choice of surgical approach in optimizing outcomes.
Keywords: Bilateral talus fracture-dislocation, comparative analysis, open reduction, and internal fixation versus percutaneous fixation.
Fractures of the talus result from high-energy trauma often associated with incidents such as automobile accidents and falls from significant heights [1]. The etiology of the injury involves the application of compressive stresses on the talus, which are transferred from the tibia due to the weight force exerted on it, as well as from the ground. Although talus fractures are the second-most prevalent fractures affecting the tarsal bones, the incidence of bilateral talus fracture-dislocation is rare [2]. It accounts for a mere 0.06% of dislocations and 2% of talus injuries [1]. Hawkins described fractures occurring in the neck of the talus with their associated joint dislocations [3]. These complex injuries pose unique challenges due to the risk of complications, including avascular necrosis and post-traumatic arthritis [2, 4]. Despite the use of suitable interventions and anatomical fixation, these injuries have a poor prognosis [2]. Management demands timely intervention, meticulous surgical planning, and a choice between surgical approaches. This case study explores the comparative outcomes of two surgical techniques in optimizing orthopedic results.
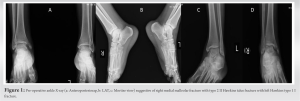
In this case study, a 30-year-old man had an injury to both ankles as a result of a fall from a five-storey height while engaged in his occupational duties as a painter. The individual fell on the floor with both feet in a dorsiflexed position – the potential mechanism of injury resulting from dorsiflexion, and supination. On admission, the patient remained awake and had stable hemodynamics, 4 h after the occurrence of the traumatic event, the Glasgow Coma Scale scoring was 15. The patient had pronounced bilateral ankle edema without any blisters. The extremities were warm, and there was no indication of any neurovascular impairment. Ankle radiographs revealed a closed talar neck fracture of the left ankle consistent with Hawkin type I classification. On the right side, there is a closed talus fracture of the Hawkin type II, accompanied by a fracture of the medial malleolus (Fig. 1). The patient received pre-operative management consisting of strict limb elevation using a below-knee splint, application of cold fomentation, and initiation of trypsin therapy from admission until the presence of skin wrinkling. The patient had trauma to the operation timing of 8 days. For the right side, he underwent a surgical procedure including open reduction and internal fixation, using a cannulated cancellous (CC) screw for the talus and tension band wire (TBW) for the medial. Percutaneous CC screw was used after closed reduction on the left side. The surgical procedure was conducted with combined spinal-epidural anesthesia while employing tourniquet coverage. The surgical procedure included performing bilateral fixation in a single setting, with an operating duration of 150 min.
In the case of a right talus fracture, a combined medial and anterolateral approach was employed. A 7–8 cm incision was made over the medial malleolus to access the fracture site. Following the reduction of the fracture, a 40 mm × 4 mm CC screw was inserted using a guide wire. In addition, an incision was made on the anterolateral aspect of the ankle joint, through which another guide wire was inserted and a 40 mm × 4 mm CC screw was inserted. During the surgery, a bone defect was identified and subsequently corrected using allograft material. The medial malleolus was successfully reduced under direct visualization, followed by the insertion of a Kirschner wire (K-wire) and TBW to complete the procedure. On the other side, percutaneous CC screw fixation followed closed reduction. A stab incision was made at the posterolateral aspect of the ankle and two guide wires were inserted diagonally in an anteromedial direction to intersect the fracture site, with the use of fluoroscopy guidance. Two screws measuring 45 mm × 4 mm were utilized for fixation. The confirmation of reduction was done by the use of fluoroscopy.
Bilateral talar fracture-dislocations with medial malleolus fractures are uncommon in the medical literature. The low number of published cases exemplifies the complex nature of this injury pattern, also emphasizing its rarity. As demonstrated in the provided example, the mechanism of damage frequently involves a fall from a substantial height, resulting in high-energy trauma [1, 5]. A precise surgical technique is required to treat such a complicated injury. To provide stability and restore anatomical alignment, open reduction and internal fixation with CC screws for the right talus fracture and K wires with TBW for the medial malleolus were used in our case [6].
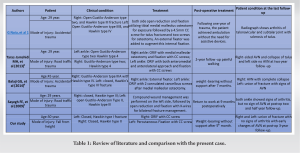
This case highlights the need for meticulous surgical planning, careful soft-tissue management, and the choice of surgical approach in achieving optimal outcomes in the management of bilateral talus fracture dislocations. The comparable outcomes of two surgical techniques (open reduction internal fixation vs. closed reduction percutaneous fixation) reaffirm the significance of surgical expertise and thoughtful planning in addressing these rare and challenging orthopedic cases.
In rare bilateral talar fracture dislocations, carefully planned delayed therapy with open reduction and stable osteosynthesis may offer superior outcomes compared to hasty acute procedures. Surgical teams should prioritize surgical expertise and comprehensive planning in managing such complex cases.
References
- 1.Noia G, Silluzio N, Sircana G, Maccauro G, Ziranu A. Aviator’s fracture - bilateral fracture-dislocation of talus in a 29-year-old patient: A case report. Malays Orthop J 2019;13:80-4. [Google Scholar]
- 2.Taraz-Jamshidi MH, Shapari O, Shiravani R, Moalemi S, Birjandinejad A. Simultaneous bilateral fracture dislocation of the talus: A case report. Trauma Mon 2013;18:90-4. [Google Scholar]
- 3.Alton T, Patton DJ, Gee AO. Classifications in brief: The Hawkins classification for talus fractures. Clin Orthop Relat Res 2015;473:3046-9. [Google Scholar]
- 4.Balaji GG, Arockiaraj J. Bilateral talus fracture-dislocation: Is avascular necrosis inevitable? BMJ Case Rep 2014;2014:bcr2014205367. [Google Scholar]
- 5.Vosoughi AR, Fereidooni R, Shirzadi S, Zomorodian SA, Hoveidaei AH. Different patterns and characteristics of Talar injuries at two main orthopedic trauma centers in Shiraz, south of Iran. BMC Musculoskelet Disord 2021;22:609. [Google Scholar]
- 6.Aygün Ü, Çalçk Y, Alkan B, Işçk C. Simultaneous bilateral fracture unilateral dislocation of the talus. J Am Podiatr Med Assoc 2016;106:370-4. [Google Scholar]
- 7.Sayegh FE, Nikolaides AP, Anagnostidis KS, Kapetanos GA. Simultaneous bilateral fracture-dislocation of the talus: A case report. Foot (Edinb) 2009;19:125-9. [Google Scholar]
- 8.Vints W, Matricali G, Geusens E, Nijs S, Hoekstra H. Long-term outcome after operative management of talus fractures. Foot Ankle Int 2018;39:1432-43. [Google Scholar]
- 9.Kopp L, Obruba P, Riegl J, Meluzinová P, Edelmann K. Chirurgická léčba zlomenin talu--střednědobé funkční a rentgenové výsledky [Surgical management of talus fractures: Mid-term functional and radiographic outcomes]. Acta Chir Orthop Traumatol Cech 2013;80:165-70. [Google Scholar]
- 10.Zeman J, Matějka J, Pavelka T. Chirurgické léčení zlomenin krčku a těla talu [Surgical treatment for factures of the neck and body of the talus]. Acta Chir Orthop Traumatol Cech 2012;79:119-23. [Google Scholar]