Various techniques have been described for high-grade spondylolisthesis, with significant controversies regarding in situ fusion versus reduction and the techniques for achieving fixation. Spine deformity study group classification gives guidelines about balanced and unbalanced pelvis and advises reduction and fusion in case of unbalanced pelvis for correction of biomechanical and global sagittal alignment. Reduction techniques should emphasize the restoration of lordosis rather than focusing on translation.
Dr. Rajendra Sakhrekar, Yonsei Okay Hospital, Seoul, South Korea. E-mail: raj.sakhrekar1@gmail.com
IntroductionHigh-grade spondylolisthesis is defined as cases with more than 50% displacement and spondylolisthesis with Meyerding grade III and higher. The surgical management of high-grade spondylolisthesis is highly controversial. Many surgical methods have been reported such as posterior in situ fusion, instrumented posterior fusion with or without reduction, combined anterior and posterior procedures, spondylectomy with reduction of L4 to the sacrum (for spondyloptosis), and posterior interbody fusion with trans-sacral fixation. The literature has recently mentioned minimally invasive transforaminal lumbar interbody fusion for high-grade spondylolisthesis. This study aimed to review the recent literature that describes the surgical outcomes associated with various surgical techniques used for high-grade spondylolisthesis.
Materials and MethodsRecent articles were searched on search engines such as PubMed and Google Scholar using keywords such as “high-grade spondylolisthesis,” “surgical techniques,” and “complications.”
DiscussionThe surgical management of high-grade spondylolisthesis is an area of significant controversy. The literature is replete with regards to the need for reduction, decompression, levels of fusion, the nature of instrumentation, surgical approaches including open, minimally invasive, and “mini-open” procedures, and various techniques for reducing the slip and fusion strategy. The three basic options of high-grade spondylolisthesis include in-situ fusion, partial reduction and fusion, and complete reduction.
ConclusionVarious techniques have been described for high-grade spondylolisthesis. Spine deformity study group classification gives guidelines about balanced and unbalanced pelvis and advises reduction and fusion in case of unbalanced pelvis for correction of biomechanical and global sagittal alignment. Each of the surgical techniques has its advantages and disadvantages. However, individual authors’ experience, skill levels, and anatomic reduction with fusion techniques have yielded encouraging results.
KeywordsHigh-grade spondylolisthesis, surgical techniques, in situ fusion, reduction and fusion, complications.
High-grade spondylolisthesis is defined as cases with more than 50% displacement and spondylolisthesis with Meyerding grade III and higher [1]. The surgical management of high-grade spondylolisthesis is highly controversial, even though 90% of these patients are typically symptomatic and untreated, with often progressive slips. Patients can present with low back pain, leg pain, hamstring tightness, neurological deficits with impaired sphincter control manifesting as stress incontinence of urine, rare motor or sensory loss, and significant spinopelvic malalignment [2]. Patients first compensate through increased intervertebral segmental lumbar lordosis (LL), leading to an overall increase in total LL. To further compensate for worsened focal L5-S1 kyphosis, increased LL is followed by increased pelvic retroversion, increasing the pelvic tilt (PT) while decreasing the sacral slope (SS). The worsening of the L5-S1 kyphosis results in an overall positive sagittal imbalance, leading to compensation with hip flexion and knee flexion caused by an extension block from hyperlordosis and a retroverted pelvis, leading to the Phalen-Dickson gait [3] (Fig. 1).
The operative methods are indicated after the failure of appropriate non-operative measures for controlling the symptoms, postural deformity, and slip progression. Surgery is aimed at achieving pain relief, adequate neural decompression, correction of a kyphotic slip angle, and obtaining solid fusion. The surgical management of high-grade spondylolisthesis is highly controversial. Many surgical methods have been reported such as posterior in situ fusion, instrumented posterior fusion with or without reduction, combined anterior and posterior procedures, spondylectomy with reduction of L4 to the sacrum (for spondyloptosis), and posterior interbody fusion with trans-sacral fixation. The literature has recently mentioned minimally invasive transforaminal lumbar interbody fusion for high-grade spondylolisthesis. Numerous prospective and retrospective studies have been carried out over the past decades to evaluate surgical outcomes of various techniques for high-grade spondylolisthesis. This study aimed to review the recent literature that describes the surgical outcomes associated with different surgical techniques used for high-grade spondylolisthesis.
Articles were searched on search engines such as PubMed and Google Scholar using keywords like “high-grade spondylolisthesis,” “surgical techniques,” and “complications.” Additional articles were identified by checking the references. Studies were initially screened based on titles and references, studies of relevant topics were selected, and a review was done.
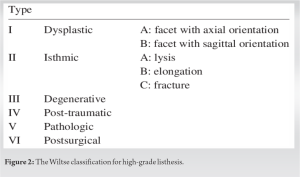
Various classification systems have been described for high-grade listhesis. The Wiltse classification is divided into five classes: (1) Dysplastic/congenital – implies there are components of underdevelopment of the arch of L5 and the facet joint at L5-S1, (2) isthmic – implies the common pars defects as the etiology – Type 2-A: Pars fatigue fracture; Type 2-B: Pars elongation due to a healed fracture; and Type 2-C: Pars acute fracture, and (3) degenerative – most commonly occurs in patients older than age 40 due to disk degeneration and subsequent facet degeneration with an intact neural arch. (4) Traumatic – fracture of the posterior column bilaterally such that spondylolisthesis occurs and (5) pathologic – an underlying metabolic bone disorder, such as osteogenesis imperfecta or metastatic disease [3–5] (Fig. 2).
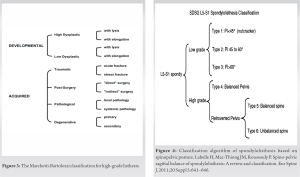
The Marchetti-Bartolozzi classification is divided into developmental and acquired. Developmental implies that there are congenital predispositions with high and low dysplastic. Acquired traumatic stress fracture is the common type of low-grade isthmic/lytic spondylolisthesis seen in teenagers and athletes. Degenerative spondylolisthesis is most commonly the acquired degenerative primary spondylolisthesis. The advantages of the Marchetti-Bartolozzi classification are that it considers the amount of dysplasia at L5-S1 (i.e., the underdevelopment of the arch of L5), whether the posterior column defect is an acute fracture versus a stress fracture, and whether the patient has had prior surgery (Fig. 3).
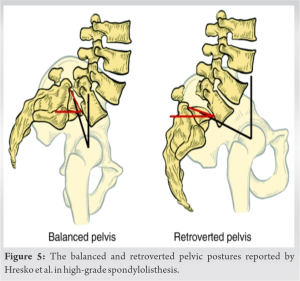
The spinal deformity study group (SDSG) recently proposed a modified classification system based on each patient’s pelvic incidence, sacropelvic balance, and spinal balance as measured radiographically [5]. This classification identifies specific lumbosacral morphology associated with high-grade slips. These deformities can be categorized into two generalized subgroups: The pelvis in high-grade spondylolisthesis can be considered balanced when the SS is high, and PT is low. In a balanced pelvis, the global spine alignment is normal and fusion without reduction is acceptable. However, a reduction with fusion is indicated in the case of an unbalanced pelvis with a low SS and high PT. In an unbalanced pelvis due to the significant retroversion of the pelvis and a vertical sacrum, the global sagittal alignment is abnormal, which necessitates the need to reduce the lumbosacral kyphosis, PT and a partial reduction in the translation, which can restore the spinal sagittal balance. Almost all patients with high-grade slips have pelvic incidence values >60°. Furthermore, patients with a retroverted pelvic posture had significantly higher rates of positive sagittal imbalance (Fig. 4 and 5).
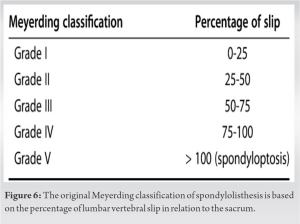
The original Meyerding classification remains the most commonly used classification for spondylolisthesis and is based on the percentage of lumbar vertebral slip in relation to the sacrum [1,6] (Fig. 6).
Investigations
X-rays- lateral view is considered the most critical view demonstrating the amount of slip of the L5 vertebra over S1, elongation of the pars or stress fracture, and instability of the lumbosacral junction with the anterior translation of L5 with L5-S1 kyphosis. AP view may show sclerosis of the stress reaction, facet and laminar dysplasia, or spina bifida occulta of the sacrum. Oblique views may show sclerosis and elongation in pars interarticularis (Scotty dog sign). However, current literature suggests that it might provide less information than AP and lateral views, with an increased risk of radiation exposure.
Computed tomography helps to delineate and understand the anatomy of lesions. Magnetic resonance imaging (MRI) helps to understand soft-tissue structures such as disk anatomy and nerve root compression. MRI also helps in acute presentation with neurological deficits, showing stress reactions at the pars with the advantage of no radiation exposure. Earlier bone and single photon emission computer tomography scans were used to diagnose acute cases with negative findings on X-rays [2].
Surgical techniques
The surgical management of high-grade spondylolisthesis is an area of significant controversy. The literature is replete with regards to the need for reduction, the need for decompression, levels of fusion, the nature of instrumentation, surgical approaches including open, minimally invasive, and “mini-open” procedures, as well as various techniques for reduction of the slip and fusion strategy. The three basic options of high-grade spondylolisthesis include in situ fusion, partial reduction and fusion, and complete reduction. The main aim of surgical treatment is to restore the posterior tension band and anterior structural support, eventually preventing the conversion of axial load to shear forces at the lumbosacral junction. Philosophies in situ fusion vs reduction and fusion techniques for high-grade Spondylolisthesis Anatomical reduction and fusion techniques have been considered to have biomechanical advantages, improved cosmesis, improvement in gait biologics, restoration of spinal canal dimensions, and spinal sagittal alignment. However, they are technically challenging, with higher rates of blood loss, neurologic deficit, pseudoarthrosis and implant failure. The in situ fusion technique demonstrated in patients with high-grade spondylolisthesis has demonstrated few studies with less blood loss, operative time, and less technically challenging with high fusion rates. However, few studies have reported cauda equina syndrome in patients with high-grade spondylolisthesis treated with in situ fusion. Joelson et al. [7]evaluated long-term outcomes with a mean follow-up of 29 years (range 23–35 years)of 35 consecutive patients who underwent in situ arthrodesis for high-grade isthmic spondylolisthesis. They reported that these patients had self-reported outcome scores (Short Form-36 and EuroQol-5 Dimension) statistically similar to the age-matched general population and were equally likely to return to work. The same group in another article reported on the 30-year radiographic follow-up data for 39 patients who underwent in situ arthrodesis for HGS. The authors found that only three patients had global sagittal imbalance (T1 Spino-pelvic inclination >0°) at the final follow-up and that there was a significant decrease in SS at the latest follow-up when compared with 8-year follow-up data, suggesting that this surgical technique is also productive in the long-term[8]. The dilemma continues for the spinal surgeon as the literature reports few studies from a single institution in which the relative complications and functional outcomes have been compared among the various surgical procedures available for treating high-grade spondylolisthesis.
In situ fusion
The first in situ fusion for spondylolisthesis through an anterior approach using a tibial autograft strut to stabilize L5-S1 spondylolisthesis was attempted by speed in 1938 [9].
Poussa et al. studied 22 patients of high-grade listhesis operated by in situ fusion over 14.8 years from 1983 to 1991. They reported improved Oswestry disability index (ODI) scores and Scoliosis Research Society scoring questionnaire scores. They also demonstrated a lesser chance of adjacent segment disc degeneration, decreased mean slip in the reduction group and less muscle atrophy on magnetic resonance imaging. The study’s drawbacks include a relatively small population size and reductions that were not anatomic [10]. In 2007, Lamberg et al. studied high-grade spondylolisthesis in children and adolescents -21 patients treated using posterolateral, 23 using anterior, and 26 using the circumferential fusion technique without instrumentation over 17.2 years from 1977 to 1991 and concluded that circumferential fusion provided significantly better long-term clinical, radiographic, and SRS total score than posterolateral or anterior fusion groups [11]. The advantages of in-situ fusion include shorter operative times, lesser blood loss, lesser chance of adjacent segment disease, and lower risk of neurological deficit. However, a 6% chance of cauda equine syndrome has been reported with in situ fusion techniques without reduction. The possible explanation suggested was that muscle relaxation caused by general anesthesia may have compromised the neural canal, leading to cauda equina syndrome. Furthermore, higher chances of pseudoarthrosis, progression of deformity, and persistence of symptoms have been reported with in situ fusion techniques.
Transacral fixation techniques
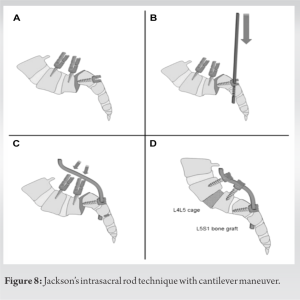
In 1982, using a posterior approach, Bohlman and Cook[12] attempted three-column spinal fixation in two cases for spondylosis. They introduced a fibular autograft across S1 into the L5 vertebral body along with decompression and uninstrumented L4-S1 posterolateral fusion, which achieved success. Jamshidi and Levi, in 2019, studied 14 patients: Six were treated with the modified Bohlman technique and eight with the reverse Bohlman technique [13]. They reported solid fusion in all cases with improvements in anterolisthesis, slip angles, and LL. The concept of three-column fixation achieved is achieved by transvertebral trans-sacral screw fixation by either posterior or anterior approach, which reduces the chances of pseudoarthrosis and reduces the shear forces across the disk space for better fusion. With advances in techniques and instrumentation, supplementary methods of achieving three-column fixation include transvertebral interbody cage fixation and the use of intrasacral rods and custom-made screws, which reduces complications including fibular graft fracture, graft resorption, slip progression, pseudoarthrosis, donor site morbidity, and graft-related complications associated with the use of fibular graft. In situ transsacral delta fixation In 2001, Smith et al.[14] reported an in situ transsacral delta fixation technique with good outcomes. In this technique, pedicle screws are placed in the L4 and L5 bilaterally. The S1 screw entry is taken in a standard fashion; however, the screw trajectory is planned to extend beyond the anterior sacral cortex and into the L5 vertebral body. Collados-Maestre et al.[15], in 2016, studied 56 patients operated on transdiscal screw fixation. They reported good ODI, COMI, SF-12, and physical and mental scores in the transdiscal group without pseudoarthrosis. The length of such delta screw is usually between 60 and 70 mm. Jackson’s intrasacral rod technique with cantilever maneuver. A cantilever maneuver is commonly advised in cases of kyphosis throughout the spine. Jackson’s intrasacral rod technique with cantilever maneuver was used by Ilharreborde et al. in 2007 to create lordosis at the level of the spondylolisthesis [[16]]. The technique involves sacral dome osteotomy followed by bilateral rods, which are then placed directly into the sacral alae caudal to the S1 pedicle screws, extending intraosseously to the level of S2 or S3 to create an “iliac buttress” to resist distal cut-out during reduction. With a cantilever maneuver, the sacrum can then be anteverted in the sagittal plane to reduce it to the L5 inferior endplate by locking the posterior rods into the L4 and L5 pedicle screw heads (Fig. 7). Hresko et al., in 2009Click or tap here to enter text., studied 26 patients with high-grade spondylolisthesis operated with posterolateral instrumented fusion using either Jackson intrasacral rods or Luque box instrumentation to achieve stable L4/sacrum fixation and reported successful fusion and good outcomes. They also wrote about the “unbalanced” high-grade listhesis with high PT and low SS and the “balanced” with low PT and high SS. They advised that reduction and fusion should be preferred in an unbalanced high-grade list thesis [5].
Distraction techniques. Harrington and Tullos, in 1969, demonstrated the technique of reduction for two cases of grade III and IV listhesis using the principle of distraction mediated through spinal instruments and lag screws with lateral gutter arthrodesis. One case had developed cauda equine syndrome, which recovered in the post-operative period [17].
External reduction techniques
Scaglietti et al.[18] and subsequently Bradford and Boachie-Adjei [17] described closed reduction and casting of spondylolisthesis. They described a 3-stage procedure: 1) initial decompression, 2) 10 days of skeletal traction, and 3) subsequent anterior reduction and fusion, with the improvement of sagittal alignment. Disadvantages of these techniques are prolonged inpatient stay and the need for prolonged bed rest during the traction period.
External transpedicular fixation
Magerl’s external fixator technique described in 1984 [19] uses three stages for the treatment. In the first stage, L5-S1 posterior wide decompression was done with both L5 nerve root identification with L5-S1 discectomy. Stab incisions were taken, and 6 mm Schanz pins were inserted in the pedicles of L4 and iliac crests, followed by Magerl’s external fixator assembled on them. In the second stage, gradual and progressive distraction of L5-S1 is done over Magerl’s external fixator, and once distraction is achieved, gradual reduction of L5 over S1 is done with retraction. Daily pin site care, radiographic and neurological status monitoring, and patient comfort evaluation are done. The average duration of the second stage is two weeks. Restriction to the supine posture was the drawback of this procedure, although the frame caused no activity restrictions, and patients were ambulated-free. In the third stage, once slip reduction is achieved through the anterior retroperitoneal approach, L5/S1 fusion is performed. Excision of the hypertrophied anterior longitudinal ligament and anterior annulus was done with thorough discectomy followed by autograft or allograft insertion in the disc space and kept in place using 6.5 mm cortical screws and washers (Fig. 8). They concluded that the procedure was effective and safe and corrected the lumbosacral kyphosis and cosmetic deformity without neurological complications [20]. Harms technique Harms, in their case series of 112 patients, reported good functional and radiological outcomes with decompression, distraction, reduction, and posterior lumbar interbody fusion. They achieved distraction using hooks in the upper lumbar spine, and reduction was accomplished using long-headed pedicle screws and sacral dome resection. The posterior diskectomy and posterior sacral dome resection facilitate reduction and, to some extent, shorten the path for the L5 roots. The author’s institutional bias and preference always has been to protect the tricortical sacral screws with iliac screws. They suggested that it should be preserved whenever the L4/L5 segment is not primarily involved [21].
Gaines procedure
Gaines reported 30 cases of high-grade spondylolisthesis operated over 30 years with a complex two-stage procedure. In the first stage, the L5 vertebral body, L4-5 disk, and L5-S1 disk are resected using an anterior approach. This is followed by a second stage posterior procedure in which L5 pedicels, and the posterior elements are excised to eventually allow the reduction of L4 over the S1 [22]. Shufflebarger and Geck, in their case series of 18 patients operated by Gill laminectomy, temporary distraction through sacral alar hooks and proximal lumbar hooks, lumbosacral discectomy, anterior decortications and grafting, and placement of bilateral titanium mesh cages packed with morselized autograft, kyphosis correction by posterior compression against anterior support reported significant improvement in slip angles, with slip angle improved from 35° to 3.8° initially and 4.3° at final follow-up with slip improvement from 77% to 13%. Fusion was achieved in all cases without any neurologic or infectious complications. They concluded that an ideal biomechanical environment for fusion will be created by reducing slip and lumbosacral kyphosis. Furthermore, structural anterior column support and posterior transpedicular instrumentation provide more resistance to shear forces than posterior instrumentation alone [23].
Minimally invasive techniques
Quraishi and Rampersaud reported the minimal access surgery approach for mobile high-grade spondylolisthesis (grade III) with good outcomes [24]. Rajakumar et al., in 2017, studied grade II (29 patients) and higher (grade III -7 patients) lumbar spondylolisthesis operated by the minimally invasive “rocking” technique and reported good radiological and patient outcomes [25]. Patel et al. 2020 reported minimally invasive transforaminal lumbar interbody fusion surgery in high-grade spondylolisthesis (grade III) patients with rheumatoid arthritis. Their surgical technique includes interbody disk space preparation, the distraction of disk space and achieving reduction by ligamentotaxis of soft tissues, inserting lordotic cage followed by percutaneous screw fixation with contoured lordotic rods fixation over reduction phalanges. They concluded it is a feasible, safe, and clinically effective technique, with less blood loss, perioperative pain, and hospital stay, with a reasonable recovery rate, solid fusion, and patient satisfaction [26].
Complications
Significant intraoperative hemorrhage, radiculopathy, neurological deficits, pseudoarthrosis, and wound infection are well-documented surgical complications with these techniques [2].
Various techniques have been described for high-grade spondylolisthesis, with significant controversies regarding in situ fusion versus reduction and the techniques for achieving fixation. SDSG classification gives guidelines about balanced and unbalanced pelvis and advises reduction and fusion in case of an unbalanced pelvis for correction of biomechanical and global sagittal alignment. Reduction techniques should emphasize the restoration of lordosis rather than focusing on translation. A cantilever reduction of the pelvis to the lumbar spine may decrease the risk of cauda equina syndrome and improve sagittal balance. Reduction lowers the pseudarthrosis rate and does not significantly increase the rate of L5 nerve injury. Each of the surgical techniques has its advantages and disadvantages. However, individual authors’ experience, skill levels, and anatomic reduction with fusion techniques have yielded encouraging results.
Various techniques have been described for high-grade
spondylolisthesis, with significant controversies regarding in situ fusion versus reduction and the techniques for achieving fixation. SDSG classification gives guidelines about balanced and unbalanced pelvis and advises reduction and fusion in case of an unbalanced pelvis for correction of biomechanical and global sagittal alignment. Reduction techniques should emphasize the restoration of lordosis rather than focusing on translation.
References
- 1.1. Meyerding HW. Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg 1956;26:566-91. [Google Scholar]
- 2.2. Tenny S, Gillis CC. Spondylolisthesis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 3.3. Tebet MA. Current concepts on the sagittal balance and classification of spondylolysis and spondylolisthesis. Rev Bras Ortop 2014;49:3-12. [Google Scholar]
- 4.4. Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis:A review and classification. Eur Spine J 2011;20 Suppl 5:641-6. [Google Scholar]
- 5.5. MEYERDING HW. Surg Gynecol Obstet 54 371-377, 1932 [Google Scholar]
- 6.6. Joelson A, Hedlund R, Frennered K. Normal Health-Related Quality of Life and Ability to Work Twenty-nine Years After in Situ Arthrodesis for High-Grade Isthmic Spondylolisthesis. J Bone Joint Surg Am 2014;96. https://doi.org/10.2106/JBJS.M.00064. [Google Scholar]
- 7.7. Joelson A, Danielson BI, Hedlund R, Wretenberg P, Frennered K. Sagittal Balance and Health-Related Quality of Life Three Decades After in Situ Arthrodesis for High-Grade Isthmic Spondylolisthesis. J Bone Joint Surg Am 2018;100:1357–65. [Google Scholar]
- 8.8. Poussa M, Remes V, Lamberg T, Tervahartiala P, Schlenzka D, Yrjönen T, et al. Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: Long-term clinical, radiologic, and functional outcome. Spine (Phila Pa 1976) 2006;31:583-90. [Google Scholar]
- 9.9. Lamberg T, Remes V, Helenius I, Schlenzka D, Seitsalo S, Poussa M. Uninstrumented in situ fusion for high-grade childhood and adolescent isthmic spondylolisthesis: Long-term outcome. J Bone Joint Surg Am 2007;89:512-8. [Google Scholar]
- 10.10. Bohlman HH, Cook SS. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Joint Surg Am 1982;64:415-8. [Google Scholar]
- 11.11. Jamshidi A, Levi AD. Reverse Bohlman technique for treatment of high-grade spondylolisthesis in an adult population. J Clin Neurosci 2019;69:230-6. [Google Scholar]
- 12.12. Smith JA, Deviren V, Berven S, Kleinstueck F, Bradford DS. Clinical outcome of trans-sacral interbody fusion after partial reduction for high-grade l5-s1 spondylolisthesis. Spine (Phila Pa 1976) 2001;26:2227-34. [Google Scholar]
- 13.13. Collados-Maestre I, Lizaur-Utrilla A, Bas-Hermida T, Pastor-Fernandez E, Gil-Guillen V. Transdiscal screw versus pedicle screw fixation for high-grade L5-S1 isthmic spondylolisthesis in patients younger than 60 years: A case-control study. Eur Spine J 2016;25:1806-12. [Google Scholar]
- 14.14. Ilharreborde B, Fitoussi F, Morel E, Bensahel H, Penneçot GF, Mazda K. Jackson’s intrasacral fixation in the management of high-grade isthmic spondylolisthesis. J Pediatr Orthop B 2007;16:16-8. [Google Scholar]
- 15.15. Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high-grade spondylolistheses based on pelvic version and spine balance: Possible rationale for reduction. Spine (Phila Pa 1976) 2007;32:2208-13. [Google Scholar]
- 16.16. Harrington PR, Tullos HS. Spondylolisthesis in children. Observations and surgical treatment. Clin Orthop Relat Res 1971;79:75-84. [Google Scholar]
- 17.17. Scaglietti O, Frontino G, Bartolozzi. Technique of anatomical reduction of lumbar spondylolisthesis and its surgical stabilization. Clin Orthop Relat Res 1976;117:165-75. [Google Scholar]
- 18.18. Bradford DS, Boachie-Adjei O. Treatment of severe spondylolisthesis by anterior and posterior reduction and stabilization. A long-term follow-up study. J Bone Joint Surg Am 1990;72:1060-6. [Google Scholar]
- 19.19. Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res 1984;189:125-41. [Google Scholar]
- 20.20. Karampalis C, Grevitt M, Shafafy M, Webb J. High-grade spondylolisthesis: Gradual reduction using Magerl’s external fixator followed by circumferential fusion technique and long-term results. Eur Spine J 2012;21 Suppl 2:S200-6. [Google Scholar]
- 21.21. Harms J. True spondylolisthesis reduction and monosegmental fusion in spondylolisthesis. In: The Textbook of Spinal Surgery. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1997. p. 1337-47. [Google Scholar]
- 22.22. Gaines RW. L5 vertebrectomy for the surgical treatment of spondyloptosis: Thirty cases in 25 years. Spine (Phila Pa 1976) 2005;30:S66-70. [Google Scholar]
- 23.23. Shufflebarger HL, Geck MJ. High-grade isthmic dysplastic spondylolisthesis: Monosegmental surgical treatment. Spine (Phila Pa 1976) 2005;30:S42-8. [Google Scholar]
- 24.24. Quraishi NA, Rampersaud YR. Minimal access bilateral transforaminal lumbar interbody fusion for high-grade isthmic spondylolisthesis. Eur Spine J 2013;22:1707-13. [Google Scholar]
- 25.25. Rajakumar DV, Hari A, Krishna M, Sharma A, Reddy M. Complete anatomic reduction and monosegmental fusion for lumbar spondylolisthesis of Grade II and higher: Use of the minimally invasive “rocking” technique. Neurosurg Focus 2017;43:E12. [Google Scholar]
- 26.26. Patel VH, Peshwattiwar VB. Grade III spondylolisthesis L5-S1 treated by minimally invasive spine transforaminal lumbar interbody fusion (MIS-TLIF) in a patient of rheumatoid arthritis. Indian Spine J 2020;3:91-6. [Google Scholar]