Aneurysmal bone cyst of the ilium in a growing child is a rare finding. The treatment of such pathology also requires due consideration of the hip joint stability.
Dr. Mantu Jain, Department of Orthopedic, AIIMS, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Aneurysmal bone cysts (ABCs) are non-neoplastic expansile, vascular, osteolytic benign tumors in the long bone, spine, and sternum. The location in the pelvis is sparse.
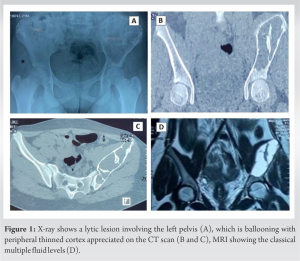
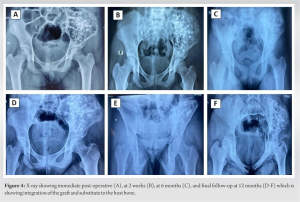
Case Report: A 12-year-old female presented with pain in her left pelvis for 6 months. On radiological examination, we found an expansile balloting lytic lesion involving almost the whole ilium and sparing the hip joint. There were multiple fluid levels seen on magnetic resonance imaging. The initial biopsy suggested ABC. Curettage and bone grafting were done along with electrocauterization and chemical cauterization. At 1-year follow-up, she is doing well without any complaints.
Conclusion: This case report demonstrates a rare ABC of the ilium that was managed with curettage and bone grafting.
Keywords: Pelvic iliac bone, aneurysmal bone cysts, curettage, chemical sclerotherapy, bone grafting.
An aneurysmal bone cyst (ABC) is a non-neoplastic expansile, vascular, osteolytic bone lesion that is classified as a benign tumor [1]. It causes bone destruction that can lead to pathological fractures and is associated with local recurrence post-treatment [2]. ABC commonly arises from the metaphyseal area of the long bone, the thorax’s membranous bones, or the spine’s posterior aspect [3]. ABC of the ilium is rare, with only few case reports [1, 2, 3, 4, 5, 6, 7]. The present case is one such report of a large ballooning ABC of the ilium in an adolescent female.
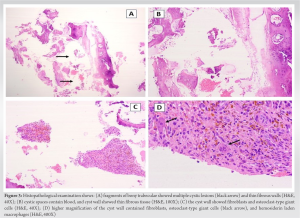
A 12-year-old female patient visited us due to pain in her left pelvis and hip joint for 6 months. The pain was dull and aching, and the patient walked with a slight limp. Other than this, there was radiating pain, and there was no numbness to the lower limb. Examinations showed that there was no local swelling of the left hemipelvis but slight pressure pain. The hip joint with a passive range of motion was normal. An anteroposterior radiograph of the pelvis showed expansile osteolytic lesions throughout the left iliac bone right up to the roof of the acetabulum (Fig. 1). A computed tomography (CT) confirmed the lesion to be expansile and with global ballooning of the ileac bone (Fig. 1). Magnetic resonance imaging (MRI) was done, which showed well-defined multi-lobulated cystic lesions with clear boundaries (12 × 10 × 5 cm) in the left iliac bone with multiple fluid-fluid surfaces suggestive of an ABC (Fig. 1). A three-phase bone scan revealed solitary heterogeneous uptake in the left iliac bone in the delayed phase, which on SPECT-CT showed a multilocular expansile cystic lesion with internal separation and a thin rim of the cortex without periosteal reaction hinting ABC. An initial biopsy revealed bony trabecula, spindle cells, hemosiderin-laden macrophages, and fluid-filled cavities confirming ABC. The patient was counseled for surgery.
A window (1.5 × 5 cm) was made on the left iliac crest, and it was seen to be filled up with blood (Fig 2). A long curettage was used to palpate the inner side, which was hollow with few intervening septa but easily reached the hard bone of the roof of the acetabulum (Fig 2).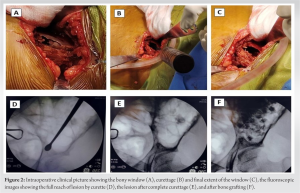
ABC in the pelvis is rare. Only 8–9% were found in the ilium in two of the largest series of the ABCs [2, 8]. More commonly, these affect younger females (<20 years), though Sharifa et al. have reported a case in a 51-year-old female [7]. It requires treatment owing to the risk of pathological fracture, which is largely guided by patients’ age, location, size, and degree of invasion. The exact pathogenesis of ABC is a matter of debate. However, an injury to the initial lesion having a network of capillaries has been postulated to trigger an increase in extravasated blood, leading to subsequent bone destruction [9]. Genetic linking to translocation between (16;17) has recently been identified [6]. Differential diagnosis includes other benign lesions such as simple bone cysts and a few tumorous conditions such as chondromyxoid fibroma, chondroblastoma, or even giant cell tumor [10]. The characteristic radiological finding for ABC has the presence of septa and fluid-fluid levels, which are well seen on MRI [11]. Nevertheless, histopathology examination is mandatory to differentiate between these radiological similar entities. Authors of management of the ABC of the ilium have described various treatment options. These include surgical resection (complete/partial), excision and curettage, and curettage and bone grafting [4, 7]. There are several challenges in a growing child owing to open physis, extensive bleeding, and the vulnerability of the acetabulum or sacroiliac joint [4]. Therefore, a balanced approach needs to be taken to keep the patient in confidence for a benign tumor that can be aggressive. Selective artery embolization has been found to be beneficial for extrapelvic ABC in reducing the recurrence rate, but in pelvic ABC, it is not recommended owing to the risk of ischemia to nerves and adjoining structures [12]. Therefore, alternate treatment with chemicals and electrocautery is another option, as was done in our case. Percutaneous injection of a fibrosing agent is a recent technique but has its complication and is expensive [13]. The recurrence rate reported in the literature is 13% over 7-year period [14]. Age <16 years and size of lesion >5 cm are among the few risk factors predisposing to recurrence. Therefore, long-term follow-up is mandatory.
ABC of the ilium in a growing child can be treated with curettage and bone grating. Long-term follow-up is required to look for any recurrences.
ABC of the ilium is a rare location that commonly affects growing children, predominantly females. The extensive involvement of the ilium mandates treatment which must also consider the stability of the adjoining hip joint. In growing age, bone grafting and curettage are recommended, but follow-up is necessary to look for recurrences.
References
- 1.Kim CG, Kweon SH. Primary aneurysmal bone cyst in the iliac bone: A case report. Hip Pelvis 2014;26:202-5. [Google Scholar]
- 2.Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH. Treatment of aneurysmal bone cysts of the pelvis and sacrum. J Bone Joint Surg 2001;83:1674-81. [Google Scholar]
- 3.Huang TL, Chen WM, Chen WY, Chen TH. Huge aneurysmal bone cyst of iliac bone in a mid-aged female. J Chin Med Assoc 2004;67:99-103. [Google Scholar]
- 4.Agarwal A, Goel P, Khan SA, Kumar P, Qureshi NA. Large aneurysmal bone cyst of iliac bone in a female child: A case report. J Orthop Surg Res 2010;5:24. [Google Scholar]
- 5.Alalawi HH, Alfadhel S, Khan M, Bobseit A. Pelvic aneurysmal bone cyst in an adolescent: A case report and literature review. Cureus 2020;12:e9534. [Google Scholar]
- 6.Noordin S, Ahmad T, Umer M, Allana S, Hilal K, Uddin N, et al. Aneurysmal bone cyst of the pelvis and extremities: Contemporary management. Int J Surg Oncol 2019;4:71. [Google Scholar]
- 7.Sharifah M, Hazla N, Suraya A, Tan S. Pelvic aneurismal bone cyst. Biomed Imaging Interv J 2011;7:24-6. [Google Scholar]
- 8.Cottalorda J, Kohler R, Sales De Gauzy J, Chotel F, Mazda K, Lefort G, et al. Epidemiology of aneurysmal bone cyst in children: A multicenter study and literature review. J Pediatr Orthop B 2004;13:389-94. [Google Scholar]
- 9.Clough JR, Price CH. Aneurysmal bone cyst: Pathogenesis and long term results of treatment. Clin Orthop Relat Res 1973;97:52-63. [Google Scholar]
- 10.Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg 2012;20:233-41. [Google Scholar]
- 11.Chung JW, Lee HS. Secondary aneurysmal bone cystic change of the chondroblastoma, mistaken for a primary aneurysmal bone cyst in the patella. Knee Surg Relat Res 2014;26:48-51. [Google Scholar]
- 12.Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, Staals EL, et al. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol 2010;39:161-7. [Google Scholar]
- 13.Yildirim E, Ersözlü S, Kirbaş I, Ozgür AF, Akkaya T, Karadeli E. Treatment of pelvic aneurysmal bone cysts in two children: Selective arterial embolization as an adjunct to curettage and bone grafting. Diagn Interv Radiol 2007;13:49-52. [Google Scholar]
- 14.Capanna R, Bertoni F, Bettelli G, Present D, Biagini R, Ruggieri P, et al. Aneurysmal bone cysts of the pelvis. Arch Orthop Trauma Surg (1978) 1986;105:279-84. [Google Scholar]