Thoracotomy during childhood can lead to post-operative complications, it is essential to follow-up patients, especially to treat rapidly any iatrogenic complications like scoliosis.
Dr. David Popescu, Department of Orthopedic Surgery, Cliniques Universitaires de Saint Luc, Bruxelles, Belgium. Email: david.popescu@student.uclouvain.be
Introduction: This case report abstract discusses scoliosis, a multifactorial three-dimensional spinal deformity, including lateral curvatures on the frontal plane characterized by Cobb angle measurement, vertebral rotation on the axial plane and sagittal deformity. Scoliosis can be mild, moderate, or severe, and if left untreated, it can lead to further deformity and compromise cardiopulmonary function. Scoliosis is classified into early onset and late onset, with idiopathic scoliosis being the most common form. Early-onset scoliosis has various etiologies, including idiopathic, congenital, neuromuscular, and syndromic. Early management is crucial to minimize complications, such as restrictive ventilatory disorder and pulmonary dysplasia. This case report focuses on an iatrogenic cause of scoliosis due to rib synostosis, which is not included in the classification. Treatment options include non-operative management and surgical interventions, with the use of vertical expandable prosthetic titanium rib (VEPTR) thoracoplasty to correct the spinal deformity.
Case Report: This article illustrates the case of a 13-year-old girl who developed a left thoracic scoliosis caused by ribs fusion, following multiple right thoracotomies during childhood for esophageal atresia with tracheoesophageal fistula. No vertebral abnormalities were reported. Considering the young age of the girl, spinal fusion was not considered. A VEPTR associated with an excision of the fused ribs was used to treat this patient.
Conclusion: The aim of this article was to illustrate the importance of a regular follow-up for the patients who have undergone multiples thoracotomies during their childhood even without vertebral abnormalities and propose an early approach to avoid spinal fusion in early adulthood
Keywords: Scoliosis, esophageal atresia, growing rods, rib fusions, musculoskeletal deformity, thoracotomy.
Scoliosis is a complex three-dimensional spatial deformity of the spine. The severity of the disease is determined by the Cobb angle, which measures the degree of curvature on radiographic imaging. Mild scoliosis is characterized by a Cobb angle of <20°, while moderate scoliosis ranges from 20° to 50°. Severe scoliosis is defined by a Cobb angle >50°. Progressive scoliosis can lead to further spinal deformity, asymmetry, and potentially compromise cardiopulmonary function if left untreated [1]. It is typically classified into two groups based on the age of onset: Early onset (before 10 years) and late onset (after 10 years). The most common form of scoliosis (late-onset) is idiopathic in origin and occurs during adolescence, particularly during the peak of pubertal growth. Early-onset scoliosis accounts for approximately 10% of pediatric scoliosis cases and is usually divided into four categories based on their etiology [1, 2]:
• Idiopathic, when radiological and clinical findings confirm scoliosis without any definitive explanation
• Congenital scoliosis, involving vertebral anomaly due to failure of formation (hemivertebra) or failure of segmentation (vertebral bar). Congenital scoliosis may be associated with other malformations such as VACTERL that requires of at least three of the following congenital anomalies: Vertebral, anal, cardiac, tracheoesophageal, renal, and limb [3]
• Neuromuscular scoliosis, secondary to neurological or muscular diseases (cerebral palsy, Duchenne dystrophy, spinal muscular atrophy…)
• Syndromic scoliosis (neurofibromatosis, Prader–Willi, Ehlers–Danlos syndrome, Marfan, Trisomy 21,…)
The most feared complications of early-onset scoliosis include restrictive ventilatory disorder and pulmonary dysplasia during growth, which can limit lung volumes. Therefore, early management is crucial to minimize the consequences of scoliosis [4].
This case report highlights a rare etiology that occurs following rib synostosis and can be considered as an iatrogenic cause of scoliosis that is not included in the usual classification. During gestational follow-up or at birth, if esophageal atresia is diagnosed discovered, it is recommended to treat the malformation through thoracotomy and open surgery. Surgical treatment of esophageal atresia or other thoracic pathologies during childhood carries risks, including the development of scoliosis with concavity on the operated side. This risk is particularly significant if the procedure is repeated in the same area. The typical course of this complication begins around the age of 7 and progresses into adulthood, with an average Cobb angle of 20° [5]. In a series of 82 children who underwent esophageal atresia treatment (Gilsanz et al. [5]), 14 required a second intervention due to esophageal suture dehiscence. Among these 14 patients, 8 developed scoliosis with a Cobb angle >20°. To diagnose scoliosis as early as possible, it was essential to conduct regular radioclinical follow-up in patients who underwent such interventions and ensure proper spinal growth. The aim of this follow-up was primarily to initiate appropriate early treatment to prevent further progression of the scoliosis.
Treatment options for early-onset scoliosis vary depending on the age of the patient, severity and progression of the curvature, and skeletal maturity. Non-operative management is usually preferred in children to preserve spinal growth with options that include observation and bracing. Spinal orthoses, such as the Boston brace or Milwaukee brace, are commonly prescribed to halt the progression of scoliosis during the adolescent growth spurt. Surgical treatment may be indicated even before end of spinal growth in severe cases, preferentially non-fusion procedures. Indications and techniques are still controversial and need to be adapted to the etiology [6, 7]. To address this iatrogenic type of complication, resection of fused ribs is often performed. In this case, vertical expandable prosthetic titanium rib (VEPTR) thoracoplasty was used in association with the resection of the fused ribs. This procedure increases gradually the size of the thorax, allowing pulmonary development and growth, and corrects the spinal deformity simultaneously [2].
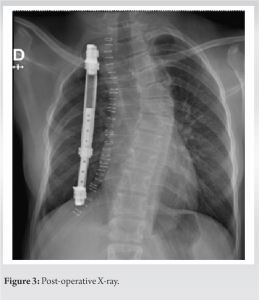
A 13-year-old girl was referred in the pediatric orthopedics department from a pediatrician for the management of a scoliosis. Her main complaints were back pain and cosmetic deformity. There was no family history of scoliosis. His restrictive lung disease was treated by the pulmonologist. Physical examination revealed a left thoracic curve, a well-healed right posterolateral thoracotomy scar, and a 1 cm shoulder asymmetry. No neurological deficits were noted. She was operated at the age of 2 months for esophageal atresia with tracheoesophageal fistula (EA-TEF) repair that was not included as part of a VACTERL syndrome. A right posterolateral thoracotomy was carried out between 4th and 5th rib without rib resection. Post-operative evolution was complicated by severe mediastinitis and empyema caused by a breakdown of the anastomosis, requiring two surgical drainages. Thereafter, six endoscopic dilatations were performed for anastomotic strictures during the 1st year of life. Full-spine EOS showed a 43° left convex scoliosis from T2 to T8, with the apex of the curve at T5 (Fig. 1) and ribs fusion between the posteriors ends of the fourth and fifth ribs and sixth and seventh ribs (Fig. 2). There was no r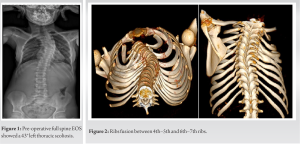
The natural history of congenital scoliosis with vertebral anomalies in patients operated for EA-TEF in the context of the VATER/VACTERL association has already been widely studied with an incidence of 9%–45% [8-11]. However, the onset of scoliosis after thoracotomy in infancy without associated vertebral anomaly is a less common complication. The incidence and pathogenesis have been poorly studied. Bisgard was the first to analyze in 1934 the development of spinal deformity following thoracic surgeries in the treatment of pulmonary pathologies such as chronic empyema, tuberculosis, and bronchiectasis. He defined the concept of “thoracogenic scoliosis” which he divided into two subgroups: The “thoracoplasty scoliosis” caused by multiple ribs resection and the “pleural scoliosis” which results from an inflammatory hyperreaction following a chronic infection. He observed that for the “thoracoplasty scoliosis,” the convexity was toward the side of thoracotomy, and for the “pleural scoliosis,” the convexity was on the opposite side [12]. Gilsanz et al. reported in 1983 a series of 8 patients who developed thoracic scoliosis after thoracotomy for EA-TEF. All the eight patients had suffered post-operative complications such as mediastinitis, empyema, requiring re-interventions in childhood, and all of them developed scoliosis with concavity toward the thoracotomy site. They also observed that the severity of scoliosis was correlated with the number of thoracotomies undergone. They proposed for four patient’s excision of fused ribs with spinal fusion and conservative treatment for the other four patients [5]. Durning et al. reported two patients who developed scoliosis after thoracotomy for EA-TEF and were treated by ribs resection [13].Dunlay et al. described a case of severe scoliosis secondary to rib fusion following tracheoesophageal fistula repair and treated with posterior spinal fusion with segmental instrumentation from T2 to L1 [14]. Korovessis et al. [15] and Wong-Chung et al. (1990) [16] also mentioned a case of left thoracic scoliosis after a right thoracotomy in childhood for EA-TEF treated conservatively (Korovessis et al.) [15] and by rib resection (Wong-Chunget al. ) [16]. Chetcuti et al. studied chest wall deformity in patients with repaired esophageal atresia. He observed a 19% incidence of scoliosis, for most of them (20/30), with the convexity toward the opposite side of the thoracic approach. The author concluded that the main predictive factor for the development of scoliosis is the number of thoracotomies which undergone during childhood, more than the existence of post-operative empyema [17]. In 2020, Mishra published a systematic review including fourteen articles, in which he reported the prevalence of secondary scoliosis after thoracotomy repair of EA-TEF at 13%, after excluding infants with congenital musculoskeletal anomalies (primary scoliosis). Of this cohort of 1338 children, only eight children had a Cobb angle >40° and only 10 had undergone spinal surgery [18].
Scoliosis secondary to thoracotomies for other indications than EA-TEF has also been described by Kaito et al. for congenital heart disease [19], Roclawski et al. [20] and Van Biezen et al.[21] for aortic coarctation repairs, and Aydin et al. [22] for congenital diaphragmatic hernia. As this complication is relatively rare and not widely reported, no preventive technique has yet been published to limit the risk of iatrogenic scoliosis after thoracoplasty in childhood. However, we recommend clinical and radiological follow-up for any child who has undergone multiple thoracotomies in infancy, to initiate early treatment. This case report highlights another case of severe left thoracic scoliosis caused by rib fusion, following thoracotomy during childhood for EA-TEF. In our case, a severe post-operative infection had occurred requiring multiple re-interventions, increasing the inflammatory reaction. A thoracic curvature with a convexity opposite to the ribs fusion had progressively developed which can be described as pleural scoliosis following Bisgaard classification. We decided to treat it with the same principle as a spondylocostal dysplasia, using a growing rods system (VEPTR) associated with fused segments resection as described by Campbell [23]. The patient will have to undergo costal distractions each 6 months until the end of his spinal growth. With this device, we hope for a progressive correction of the curvature and to avoid spinal fusion at the end of puberty. This case illustrates the necessity to follow-up patients operated for EA-TEF during infancy, even without associated vertebral anomaly.
This case report highlights the importance of long-term follow-up for children who undergo thoracotomy for EA-TEF, even without associated vertebral anomalies. This rare case of severe left thoracic scoliosis caused by rib fusion following thoracotomy was treated using the VEPTR system. This approach allowed for progressive correction of the curvature and preserved spinal growth, avoiding spinal fusion. By closely monitoring these patients, complications like scoliosis can be detected early and appropriate treatment initiated. Further research and vigilance in post-operative care are crucial to optimize outcomes and ensure patient well-being during their developmental stages.
This article highlights the importance of post-operative follow-up and individualized treatment strategies in cases of early-onset scoliosis, such as the use of VEPTR, in managing complications and optimizing outcomes for patients who have undergone thoracotomy for EA-TEF. The case also demonstrates that VEPTR can be an effective approach for progressive curvature correction while preserving spinal growth, potentially avoiding the need for more invasive procedures like spinal fusion.
References
- 1.Ruiz G, Torres-Lugo NJ, Marrero-Ortiz P, Guzmán H, Olivella G, Ramírez N. Early-onset scoliosis: A narrative review. EFORT Open Rev 2022;7:599-610. [Google Scholar]
- 2.LeFever D, Menger RP. Infantile and juvenile scoliosis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 3.Quan L, Smith DW. The VATER association. Vertebral defects, Anal atresia, T-E fistula with esophageal atresia, Radial and Renal dysplasia: A spectrum of associated defects. J Pediatr 1973;82:104-7. [Google Scholar]
- 4.Yang S, Andras LM, Redding GJ, Skaggs DL. Early-onset scoliosis: A review of history, current treatment, and future directions. Pediatrics 2016;137:???. [Google Scholar]
- 5.Gilsanz V, Boechat IM, Birnberg FA, King JD. Scoliosis after thoracotomy for esophageal atresia. AJR Am J Roentgenol 1983;141:457-60. [Google Scholar]
- 6.Kim G, Sammak SE, Michalopoulos GD, Mualem W, Pinter ZW, Freedman BA, et al. Comparison of surgical interventions for the treatment of early-onset scoliosis: A systematic review and meta-analysis. J Neurosurg Pediatr 2022;31:342-57. Erratum in: J Neurosurg Pediatr 2023;31:388. [Google Scholar]
- 7.Bydon M. Erratum. Comparison of surgical interventions for the treatment of early-onset scoliosis: A systematic review and meta-analysis. J Neurosurg Pediatr 2023;31:388. Erratum for: J Neurosurg Pediatr 2022;31:342-57. [Google Scholar]
- 8.Soliman HA, Faure C, Berubé G, Mac-Thiong JM, Barchi S, Parent S. Prevalence and natural history of scoliosis and associated congenital vertebral anomalies in patients operated for esophageal atresia with or without tracheoesophageal fistula. J Pediatr Surg 2019;54:1308-11. [Google Scholar]
- 9.Keckler SJ, St Peter SD, Valusek PA, Tsao K, Snyder CL, Holcomb GW 3rd, et al. VACTERL anomalies in patients with esophageal atresia: An updated delineation of the spectrum and review of the literature. Pediatr Surg Int2007;23:309-13. [Google Scholar]
- 10.Westfelt JN, Nordwall A. Thoracotomy and scoliosis. Spine (Phila Pa 1976) 1991;16:1124-5. [Google Scholar]
- 11.Sistonen SJ, Helenius I, Peltonen J, Sarna S, Rintala RJ, Pakarinen MP. Natural history of spinal anomalies and scoliosis associated with esophageal atresia. Pediatrics 2009;124:e1198-204. [Google Scholar]
- 12.Bisgard JD. Thoracogenic scoliosis. Influence of thoracic disease and thoracic operations on the spine. Arch Surg 1934;29:417-45. [Google Scholar]
- 13.Durning RP, Scoles PV, Fox OD. Scoliosis after thoracotomy in tracheoesophageal fistula patients. A follow-up study. J Bone Joint Surg Am 1980;62:1156-9. [Google Scholar]
- 14.Dunlay RP, Jones KB, Weinstein SL. Scoliosis caused by rib fusion following thoracotomy for tracheoesophageal fistula: Case report. Iowa Orthop J 2007;27:95-8. [Google Scholar]
- 15.Korovessis P, Papanastasiou D, Dimas A, Karayannis A. Scoliosis by acquired rib fusion after thoracotomy in infancy. Eur Spine J 1993;2:53-5. [Google Scholar]
- 16.Wong-Chung J, France J, Gillespie R. Scoliosis caused by rib fusion after thoracotomy for esophageal atresia: Report of a case and review of the literature. Spine (Phila Pa 1976) 1992;17:851-4. [Google Scholar]
- 17.Chetcuti P, Myers NA, Phelan PD, Beasley SW, Dickens DR. Chest wall deformity in patients with repaired esophageal atresia. J Pediatr Surg 1989;24:244-7. [Google Scholar]
- 18.Mishra PR, Tinawi GK, Stringer MD. Scoliosis after thoracotomy repair of esophageal atresia: A systematic review. Pediatr Surg Int 2020;36:755-61. [Google Scholar]
- 19.Kaito T, Shimada M, Ichikawa H, Makino T, Takenaka S, Sakai Y, et al. Prevalence of and predictive factors for scoliosis after surgery for congenital heart disease in the first year of life. JB JS Open Access 2018;3:e0045. [Google Scholar]
- 20.Roclawski M, Sabiniewicz R, Potaz P, Smoczynski A, Pankowski R, Mazurek T, et al. Scoliosis in patientswith aortic coarctation and patent ductus arteriosus: Does standard posterolateral thoracotomy play a role in the development of the lateral curve of the spine? Pediatr Cardiol 2009;30:941-5. [Google Scholar]
- 21.Van Biezen FC, Bakx PA, De Villeneuve VH, Hop WC. Scoliosis in children after thoracotomy for aortic coarctation. J Bone Joint Surg Am 1993;75:514-8. [Google Scholar]
- 22.Aydın E, Özler O, Burns P, Lim FY, Peiró JL. Left congenital diaphragmatic hernia-associated musculoskeletal deformities. Pediatr Surg Int 2019;35:1265-70. [Google Scholar]
- 23.Campbell RM Jr. VEPTR: Past experience and the future of VEPTR principles. Eur Spine J 2013;22:S106-17. [Google Scholar]