Functional outcome of surgical treatment for spondylolisthesis using posterior stabilization and fusion techniques.
Dr. S Noordeen, Department of Orthopedics, Srinivasan Medical College and Hospital, Trichy, Tamil Nadu. India. E-mail: drnoordeens@gmail.com
Introduction: Spondylolisthesis is a spinal condition characterized by the forward displacement of one vertebra over another, leading to instability and associated symptoms. Surgical intervention is often recommended for patients with symptomatic spondylolisthesis unresponsive to conservative treatment. The objective of this study was to analyze the functional outcomes of surgical management utilizing posterior stabilization and fusion techniques in patients with spondylolisthesis.
Materials and Methods: This is a prospective study conducted on 30 patients who underwent surgical treatment for spondylolisthesis with posterior trans-pedicular screw fixation with conventional or reduction screws and fusion. Meyerding’s grade of listhesis, Japanese Orthopaedic Association (JOA) score, Oswestry disability index (ODI) score and pain scores such as visual analog scale (VAS), numerical rating scale 11 (NRS-11), and pain relief rate were used to analyze the functional outcome.
Results: Postoperatively, Meyerding’s grade of listhesis and the JOA score had improved significantly. The ODI score and pain scores such as VAS, NRS-11, and pain relief rate were better after surgical interventions. There was full motor recovery in 13 patients and 14 patients had full sensory recovery, while six patients had sensory blunting at the time of the time of the last follow-up. Twenty-six (80.7%) patients had clinically successful results and radiological/clinical fusion while four of the patients did not achieve a clinically successful result and radiological/clinical fusion. The average time for bony fusion was 5.58 months with the earliest being 4 months and the latest 12 months. Intraoperatively, one patient had screw slippage and one had a dural tear. Postoperatively, four patients had infection, two patients were presented with deep infection, and the instrumentation had been removed.
Conclusion: This study demonstrated favorable functional outcomes and improvements in pain, disability, and quality of life measures following surgical intervention.
Keywords: Low back pain, spondylolisthesis, posterior stabilization and fusion, functional outcome.
Low Back pain is one of the common causes for patients visiting orthopedic outpatient clinics in our country. In only 5–10% of the cases a specific cause such as degenerative conditions, inflammation, infection, neoplasm, metabolic bone disease, referred pain, psychogenic pain, trauma, or congenital disorders may be identified. The majority of cases are non-specific musculoskeletal disorders. Causes of mechanical back pain include lumbar strain, herniated discs, spondylosis, spondylolisthesis, spinal stenosis, and fractures. Spondylolisthesis is relatively a common spinal disorder characterized by the anterior displacement of one vertebra in relation to the adjacent vertebrae. It can lead to spinal instability, nerve compression, and debilitating symptoms such as back pain, radiculopathy, and neurogenic claudication. The degenerative spondylolytic variety of spondylolisthesis is found to be the most common type with a prevalence of 19.1–43.1% and 3.7–11.5%, respectively [1]. When conservative treatments fail to provide sufficient relief, surgical intervention becomes necessary to address the underlying instability and alleviate symptoms. The significance of surgical intervention in degenerative spondylolisthesis has been widely recognized in medical literature [2-4]. While decompression surgery has demonstrated favorable results in addressing degenerative spondylolisthesis, fusion remains a central component in the management of this condition. Although, posterior stabilization and fusion techniques are commonly employed surgical procedures in the management of spondylolisthesis [5-7], studying the functional outcomes over an extended period can help determine the sustainability and durability of the benefits achieved through posterior stabilization and fusion. This study can contribute to the existing body of knowledge by evaluating the benefits and limitations of posterior stabilization and fusion in comparison to other surgical methods. Assessing the functional outcomes allows for an examination of the incidence and impact of post-operative complications. This information is critical for refining surgical techniques, minimizing complications, and improving overall patient safety. This study aimed to evaluate the functional outcomes of patients who underwent surgical treatment with posterior stabilization.
This descriptive study was conducted on 30 patients who underwent surgical treatment for spondylolisthesis with posterior transpedicular screw fixation with conventional or reduction screws and fusion. The patients included in the study were based on following inclusion and Exclusion criteria.
Inclusion criteria
The following criteria were included in the study:
1. All the spondylolisthesis patients aged above 35 years undergoing posterior surgical fixation with instrumentation and fusion with bone grafting during the period of study in our hospital.
Exclusion criteria
The following criteria were excluded from the study:
1. Patients with any other spinal pathologies.
2. Patients who have had earlier surgeries on their spine.
3. Patients who did not have a regular follow-up for a period of minimum 6 months.
4. Patient details, including demographic information, pre-operative symptoms, radiographic data, surgical details, and follow-up assessments, were recorded. All the patients had the routine blood investigations done that are required for surgery. They all had X-rays of the lumbosacral spine – anteroposterior, lateral, oblique as well as the flexion and extension views. All the patients had an MRI of the spine. All the patients had undergone posterior decompression with fusion and bone grafting.
Analysis of results
The results of the surgical procedures were analyzed based on improvement in Japanese Orthopaedic Association (JOA) Score and Meyerding’s grade of listhesis. The results of JOA score were classified as having achieved clinical success or not. They were mainly assessed for low back pain, leg pain, gait, Straight leg raising test, motor, and sensory disturbances. Patients who had JOA score of more than 12 out of 15 were classified as having achieved clinical success. Neurological outcomes were noted in all patients. Pre-operative and post-operative scores were compared to evaluate the effectiveness of the surgical intervention. The disability index was scored for individual patients using an Oswestry Disability Index (ODI) Assessment Questionnaire. The patient’s pain perception was noted on visual analog scale (VAS) and numerical rating scale (NRS) scores, and the degree of pain relief was assessed by the PRR score. VAS is a 10 cm scale (scored as “10” = worst pain imaginable and “0” = no pain), NRS has endpoints “0” (no pain), and “10” (worst pain imaginable). Pain Relief Rate: “< 25%” = unrelieved, “25–49%” = mere relief, “50–74%” = moderate relief, “75–99%” = significant relief, and “100%” = complete relief) was also assessed. VAS score, NRS score, and ODI score were assessed preoperatively, 3 months, and 12 months postoperatively, and PRR was assessed at 3 months and 12 months postoperatively.
Surgical procedure
Under general anaesthesia, the patient is placed on the spinal frame under c-arm. A standard posterior midline incision was made and the paraspinal musculature detached and freed to the outer margins of the transverse processes. If indicated, extensive decompression and laminectomy are carried out at single or multiple levels with care taken not to injure the underlying dura of spinal nerves. Each nerve root is then inspected at the predetermined levels and wide and extensive decompression was carried out, including osteotomy of facet joint. Under direct visualization and with the aid of c-arm, the pedicles of each vertebra are identified, and a small awl is used to ream a small canal into the vertebral body through its pedicle. The pedicle screw is inserted until the large cancellous threads are buried into the body and pedicle. It is important to keep the plane of the screw perpendicular to the longitudinal axis of the spine at each level. Remaining pedicle identified and pedicle screw inserted and checked under c-arm. Fixation of screw in the first and second sacral segment deserve special mention. First sacral pedicle is located caudal to the superior sacral facet. Second sacral pedicle screw can be inserted 45°lateral inclination into sacral ala. Mass Miami rod is bent to normal lordotic curvature after measurement. Prior to insertion of rod, bone graft is placed over the previously prepared transverse process, pedicle and over the facet joint. Then, rod is inserted over the pedicle screw and posterior tapered nuts screwed on. These are further tightened with the help of additional wrench to ensure a rigid fixation. Wound closed in layer with drain incision. Total operative time is about 3 h. Post-operative antibiotic prophylaxis continued. Post-operative care involves positioning the patient in a supine position and providing sufficient pain relief for the initial 48 h. The drainage tube is removed on the 2nd day after the surgery. Intravenous antibiotics are administered for a duration of 3 days, after which they are transitioned to oral antibiotics for an additional 3 days. On the day following the surgery, the patient is encouraged to sit and walk, and mobilization is facilitated without the use of a brace. Routine dressings are applied, and sutures are taken out on the 14th day. On discharge, patients receive instructions not to engage in heavy lifting activities for a period of 6 months.
In our study, a total of 30 patients with 22 (73%) females and 8 (27%) males were included. The age was ranging from 35years to 65 years with the average age at the time of surgery being 56.13 ± 6.02 years. The duration of symptoms ranging from 1 month to 10 years with a mean period of 25.7 months. Most of the patients were housewives followed by heavy manual worker. All 30 patients had low back pain with radicular pain (67%), limp (60%), numbness (43%), weakness (33%), and bladder bowel disturbances (6%). Most of the patients had previous treatment with NSAIDS being the most common while being hospitalized and taking rest, traction, and physiotherapy being the other modes of treatment.
Pre-operative observations
The most common level of spondylolisthesis was observed at the L5-S1 (70%), followed by L4-L5 level (30%). Most patients (80%) had degenerative spondylolisthesis. All the patients had para spinal spasm and 26 (87%) had spinal tenderness while some of them had scoliosis (27%), kyphosis (20%), transverse furrow (13%), and palpable step (70%). All the patients had reduced spinal movements. A total of 23 patients had motor deficits with left and right lower limbs having an almost equal distribution. Twenty-four patients had sensory deficits with distribution in the L5 (36%), L4/L5 (23%), L5/S1 (6%), S1 (6%), and L4 (6%) dermatomes. Eleven patients had a retarded ankle reflex. All the patients had a positive straight leg raising test, bowstring test, and Lassegue test. Twenty (67%) patients had Grade III, 8 (27%) had Grade II, and 2 (6%) had Grade I Meyerding’s grade of listhesis. The mean follow-up duration was 12 months. The patients had a JOA Score ranging from 6 to 9 with mean score of 7.65. Functional outcomes significantly improved following surgical intervention.
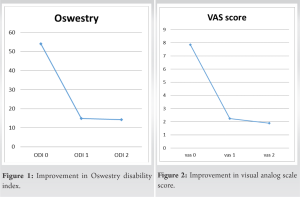
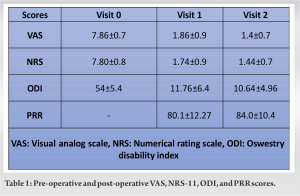
Post-operative observations
Postoperatively, Meyerding’s grade of listhesis has improved. 13 (43%) patients became normal, 12 (40%) patients had Grade I, 5 (17%) patients had Grade II, and none of the patient have Grade III (Table 2). The JOA score had improved from range 6–9 to 7–15 with an average score of 13.11. The mean pre-operative ODI score (Table 1 and Fig. 1) of 54 ± 5.4 decreased to 10.64 ± 4.96 at the final follow-up (P < 0.001). The VAS pain scores (Table 1and Fig. 2) improved from a mean of 7.86 ± 0.7 to 1.4 ± 0.7 (P < 0.001). The NRS-11 pain scores improved from a mean of 7.80 ± 0.8 to 1.44 ± 0.7 (P < 0.001). The overall pain relief rate scores showed a substantial improvement of 80.1 ± 12.27 and 84.0 ± 10.4. Fig. 3 shows illustrative case of Grade 2 degenerative spondylolistheses treated with transforaminal lumbar interbody fusion with pedicle screw stabilization.
Eight patients had low backache, while four had radiculopathy and three had a limp at the time of their last follow-up. There was full motor recovery in 13 patients while eight patients improved their motor power. Three patients had the same while the motor power of one1 patient deteriorated. Fourteen patients had full sensory recovery, while six patients had sensory blunting at the time of the time of the last follow-up. Twenty-six (80.7%) patients had clinically successful result and radiological/clinical fusion while four of the patients did not achieve a clinically successful result and radiological/clinical fusion. The average time for bony fusion was 5.58 months with the earliest being 4 months and the latest being 12 months.
Complications
In this study, 4 (23%) patients out of 30 had developed complications. Intraoperatively, one patient had screw slippage and one had a dural tear.
Post-operatively, three patients had deep infection while one patient had superficial infection. In two patients with deep infection, the instrumentation had been removed while with the others were controlled with broad spectrum antibiotics.
Spondylolisthesis is a spinal disorder associated with significant pain and disability, often limiting patients’ daily activities and overall quality of life. When conservative treatments fail to provide adequate relief, surgical intervention becomes necessary. The present study aimed to analyze the functional outcome of surgical management of spondylolisthesis using posterior stabilization and fusion techniques. Population-based studies have suggested that the prevalence of spondylolisthesis is 6% in adult [8, 9]. Among them 25%, experience at least a period of significant back pain in their lifetime. Even in our study, almost all the 30 patients had back pain. Moreover, 20 of them had intolerable back pain. In our study, Meyerding classification was used. It describes spondylolisthesis in five grades depending on the amount of vertebral slippage on radiographs about the caudal vertebrae. < 25% slippage is Grade I, 26–50% Slippage is Grade II, 51–75% slippage is Grade III, 76–100% slippage is Grade IV, and Grade V is over 100% slippage. In our study, none of the subject had more than 75% slippage [10]. Usually, conservative management is enough for Grade I and Grade II spondylolisthesis whereas Grade III, IV, and V are treated with surgical management. However, according to Harris and Weinstein and Lundine et al. Studies, no significant difference was found in the comparison of surgical and conservative management in Grade III and IV and V spondylolisthesis patients [11, 12]. Zdeblick reported on a prospective study of 124 patients who underwent lumbar fusion for degenerative disorders. The overall fusion rate was 86% in patients with rigid instrumentation compared with 65% in patients with non-instrumentation fusion. Rigid instrumentation showed higher good to excellent results (95% vs.71%) than with non-instrumentation. The rate of revision surgery was 8% in non-instrumentation and 0% in rigid instrumentation. This study recommended the use of rigid pedicle screw fixation in patients undergoing fusion for degenerative spondylolisthesis [13,14]. The findings of our study also demonstrated that the surgical intervention utilizing these techniques leads to favorable functional outcomes, including improvements in pain, disability, and quality of life measures. Mochida et al. studied the success rate of bony fusion and the clinical results of rigid instrumentation and no instrumentation for a single-level lesion of degenerative spondylolisthesis. His study group had 67 patients. The patients with instrumentation had a forward reduction of 40% slippage and the success rate was 91% [15]. The present study had 80% bony fusion and 80% success rate. The choice of posterior stabilization and fusion as the surgical technique in this study is supported by its ability to restore stability to the affected spinal segment. Using pedicle screw fixation along with interbody fusion, the procedure aims to achieve spinal alignment, decompression of neural elements, and ultimately, reduction of pain, and improvement in function. The study also considered various factors that may impact the surgical outcomes. The level of spondylolisthesis, with most cases occurring at L5–S1 in isthmic type and L4–L5 in degenerative type, is consistent with the well-known distribution of this condition. This is like the study by Elmorsy et al. [16]. It is worth noting that this study has some limitations. First, it involves only small number of subjects. A prospective study design with a larger sample size and longer follow-up period would provide stronger evidence. In addition, the absence of a comparison group receiving alternative surgical techniques or non-surgical management restricts the ability to directly compare the outcomes. Moreover, while the functional outcomes improved significantly, it is crucial to acknowledge the potential complications associated with surgical intervention for spondylolisthesis. These may include infection, hardware failure, adjacent segment degeneration, and persistent or recurrent symptoms. Long-term studies assessing the durability of surgical outcomes and evaluating the occurrence of complications are necessary to fully understand the risks and benefits of this intervention. Although recent studies support evidences on TLIF that ensures successful fusion in spondylolisthesis patients [17], Posterior decompression and spinal fusion was also found as an effective way in the management of lumbosacral listhesis [18, 19].
The findings of this study support the effectiveness of surgical management utilizing posterior stabilization and fusion techniques for patients with spondylolisthesis. The significant improvements in functional outcomes, pain relief, and quality of life measures highlight the positive impact of this surgical approach. However, further research is needed to strengthen these findings, particularly through prospective studies with larger sample sizes and longer follow-up periods. In addition, evaluating long-term outcomes and potential complications will help guide treatment decisions and optimize patient care in the management of spondylolisthesis.
Findings from our study underscore the positive functional outcomes achieved through surgical intervention utilizing posterior stabilization and fusion for spondylolisthesis, highlighting its potential as an effective treatment approach to enhance patient quality of life and alleviate symptoms.
References
- 1.Wang YX, Zoltán K, Deng M, Leung JC. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat 2017;11:39-52. [Google Scholar]
- 2.Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 2007;356:2257-70. [Google Scholar]
- 3.Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. J Am Acad Orthop Surg 2014;22:203-13. [Google Scholar]
- 4.Inui T, Murakami M, Nagao N, Miyazaki K, Matsuda K, Tominaga Y, et al. Lumbar degenerative spondylolisthesis: Changes in surgical indications and comparison of instrumented fusion with two surgical decompression procedures. Spine 2017;42:E15-24. [Google Scholar]
- 5.Matz PG, Meagher RJ, Lamer T, Tontz WL Jr., Annaswamy TM, Cassidy RC, et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 2016;16:439-48. [Google Scholar]
- 6.Herkowitz HN. Spine update. Degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 1995;20:1084-90. [Google Scholar]
- 7.Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 2016;374:1424-34. [Google Scholar]
- 8.Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 1984;66:699-707. [Google Scholar]
- 9.Virta L, Ro¨nnemaa T, Osterman K, Aalto T, Laakso M. Prevalence of isthmic lumbar spondylolisthesis in middle-aged subjects from eastern and western Finland. J Clin Epidemiol 1992;45:917-22. [Google Scholar]
- 10.Meyerding HW. Low backache and sciatic pain associated with spondylolisthesis and protruded intervertebral disc: Incidence, significant, and treatment. J Bone Jt Surg 1941;23:461-70. [Google Scholar]
- 11.Harris IE, Weinstein SL. Long-term follow-up of patients with grade III and IV spondylolisthesis. Treatment with and without posterior fusion. J Bone Jt Surg 1987;69:960-9. [Google Scholar]
- 12.Lundine KM, Lewis SJ, Al-Aubaidi Z, Alman B, Howard AW. Patient outcomes in the operative and nonoperative management of high-grade spondylolisthesis in children. J Pediatr Orthop 2014;34:483-9. [Google Scholar]
- 13.Zdeblick TA. A prospective, randomised study of lumbar fusion-priliminary results. Spine 1993;18:983-91. [Google Scholar]
- 14.Simmons EH, Capicotto WN. Posterior transpediculate instrumentation of the lumbar spine. Clin Orthop Relat Res 1988;236:180-91. [Google Scholar]
- 15.Mochida J, Suzuki K, Chiba M. How to stabilize a single level lesion of degenerative lumbar spondylolisthesis. Clin Orthop Relat Res 1999;368:126-34. [Google Scholar]
- 16.Elmorsy SE, Abulnasr HA, Hassan Y, Samra M, Eissa EM. Functional outcome of surgical management of low mid-grade lumbar spondylolisthesis when considering the sagittal balance parameters preoperatively: A prospective study. Chin Neurosurg J 2022;8:35. [Google Scholar]
- 17.Jambukeswaran PS, Somasundaram AK, Jeyaraman M. Does functional outcome mandate fusion in spondylolisthesis management? A retrospective analysis of 76 cases with one year follow-up. Indian J Orthop Surg 2021;7:1-8. [Google Scholar]
- 18.Angachekar D, Deshpande S, Gudhe M, Samal N, Khan S, Gupta S. Clinical and functional outcome analysis of posterior decompression and spinal fusion surgery in the management of lumbar and sacral listhesis: A prospective cohort study. J Datta Meghe Inst Med Sci Univ 2020;15:407-13. [Google Scholar]
- 19.Omidi-Kashani F, Hassankhani EG, Shiravani R, Mirkazemi M. Surgical outcome of reduction and instrumented fusion in lumbar degenerative spondylolisthesis. Iran J Med Sci 2016;41:13-8. [Google Scholar]