Neglected chronic knee dislocation leading to osteoarthritis is a rare entity and the management poses unique challenges. Pre-operative detailed clinical and radiological examination is indispensable and presence of constrained, and hinged prosthesis is recommended in the surgical armamentarium.
Dr. Adarsh Krishna K Bhat, Department of Orthopaedics, Apollo Hospitals, Bengaluru, Karnataka, India. E-mail: adarshbhat118@gmail.com
Introduction: A case of neglected anterior dislocation of the knee leading to instablity with severe secondary osteoarthritis is very rare to come across, and there are not many reported articles to the best of our knowledge. Due to the rarity of the occurrence, there are no proper treatment guidelines laid out yet.
Case Report: A 62-year-old hypertensive male with BMI 26.6 presents with an unstable lax right knee with severe osteoarthritis secondary to untreated chronic traumatic anterior dislocation of the knee that happened 12 years back. He was examined clinically and radiologically and further underwent total knee arthroplasty (TKA) for the same at our center.
Discussion: Knee dislocation is a very rare injury and a case of neglected dislocation leading to unstable osteoarthritic knee is even more rare. These cases need thorough planning which should include an extensive clinical examination followed by imaging studies and Doppler scan to study the status of the vasculature. TKA for such a case is challenging and the use of hinged prosthesis or a constrained prosthesis is recommended when unstable.
Keywords: Total knee arthroplasty, unstable knee, neglected knee dislocation.
Anterior knee dislocation is a rare injury and results from high-energy trauma [1]. Neglected dislocation of the knee joint is even more rare [2]. There is limited number of articles published addressing it, and hence, an algorithm for the management of such cases has not been developed yet. It is unlikely for a single surgeon in his career to have faced more than a few cases of knee osteoarthritis secondary to neglected traumatic dislocation [1]. Residual subluxation or dislocation is often rare, presumably because the injury often lends itself to accurate diagnosis and appropriate treatment in the acute setting. In most reviews on this subject, chronicity of dislocation is never mentioned [3-6]. We report here a case of secondary osteoarthritis of the knee with severe laxity due to chronic neglected anterior dislocation of the knee that was treated with total knee arthroplasty (TKA).
A 62-year-old male, known case of hypertension, presented to our department with complaints of swelling, deformity of the right knee, and inability to walk comfortably without the support of a cane. The patient presents with a history of trauma to the right knee – traumatic anterior dislocation, in a road traffic accident in rural India 12 years back for which he received treatment from local osteopaths. There was no other significant history and the patient did not receive any other formal treatment. Physical examination revealed a deformed right knee with anteroposterior (AP) enlargement and fullness in the suprapatellar pouch (Fig. 1).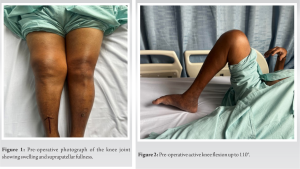
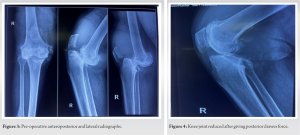

After detailed explanation of the risks and benefits to the patient and relatives, total knee replacement of the right knee was performed. A midline incision using the conventional medial parapatellar approach to the knee was made. Intraoperative examination revealed loss of articular cartilage with alteration in the morphology of both femoral and tibial condyles. Tibial posterior condyles had huge bony defects more in the posteromedial condyle (Fig. 6). The medial and lateral collateral complexes were found to be lax. The proximal tibial and femoral cuts were taken as per standard practice to achieve standard mechanical alignment. The posteromedial tibial defect was reconstructed with bone grafts and cement (Fig. 7). Further, to add stability, a metaphyseal sleeve with stem was used along with tibial base plate. The final implantation was done using DePuy Sigma®TC3 (Depuy Synthes, Warsaw, Indiana) cemented femoral component with distal augments and a 14 × 125 mm PFC® Sigma® fluted femoral stem, a DePuy MBT Revision Tibial Tray Rotating platform Cemented with 29-mm MBT Revision Cemented Metaphyseal Sleeve and 13 × 30 mm cemented modular stem. Stability was achieved using Sigma® Rotating platform TC3 Tibial Insert of size 17.5 mm (Fig. 8). The patella was resurfaced with Oval Dome Patella-3 peg of size 35 mm. The mediolateral and AP stability along with patella tracking were ascertained during trial implantation and after final implantation hence hinged fully constrained prosthesis was not used, even though it was kept ready in our surgical armamentarium. There was no residual hyperextension or fixed flexion deformity and passive flexion on table was up to 130° which was felt satisfactory. No major complications such as infection, wound breakdown, deep venous thrombosis, or vascular injury occurred.
The post-operative radiograph revealed a well-aligned and well-fixed prosthesis (Fig. 9). The patient was made to walk comfortable on the same day and was very satisfied with the final outcome. At the latest 3rd-month follow-up, the patient has a stable knee with a good range of motion of 0–110° (Fig. 10). 3rd-month radiographs show a well-fixed prosthesis (Fig. 11).
Chronic knee dislocation and subluxation is a rare entity, presumably because most knee dislocations lend themselves to accurate diagnosis and appropriate treatment acutely [1]. There are multiple reports of open reduction for chronic knee dislocation with or without ligament reconstruction. The final results ranged from poor to excellent functional outcomes [6-12]. Arthroplasty and arthrodesis are 2 conventional methods of treatment for chronic posterior knee dislocation. We could find no previous article reporting on TKA for neglected anterior dislocations leading to unstable secondary osteoarthritis of the knee in the English literature. Petrie et al. reported two successful treatments with TKA and a constraining device for posterior knee dislocation 4 months after the initial injury [1]. Chen and Chiu reported the case of a TKA without constraining implants for a 56-year-old man with neglected knee dislocation injured 30 years previously, with severe arthritis, the evolution was complicated by a posterior dislocation 5 days postoperatively. Closed reduction was performed under spinal anesthesia, and a cylindrical cast was applied with the knee in 10° of flexion. The cast was removed 4 weeks later, and physical therapy with range of motion exercises restarted without any subluxation or instability thereafter. Hence, he recommended a constraining implant to avoid dislocation postoperatively [13]. In our case, we were able to achieve complete intraoperative stability using semiconstrained prosthesis and went ahead with the same. In the immediate post-operative period, the patient was fitted with rigid knee immobilizer while ambulation. He further underwent quadriceps strengthening exercises along with range of motion physiotherapy. Limitation of the report is the unavailability of the previous X-rays during initial trauma and the long-term follow-up results of the patient.
TKA for chronic knee dislocation is a challenging procedure. Total knee replacement is recommended for long-standing chronic dislocations with secondary osteoarthritis. A complete clinical and radiological examination is indispensable during the pre-operative period. A Doppler scan should be considered to ascertain the vascular status of the limb. Constrained, hinged prosthesis should be made available intraoperatively and be used whenever the stability of the knee is in question. Proper patient education and counseling regarding the chances of infection due to long operating hours, vascular injury, revision surgeries, and information about post-operative rehabilitation protocols are of paramount importance.
Managing chronic anterior dislocation of the knee with instability and significant bony defects can be challenging, due to the rarity of its occurrence and lack of consensus regarding management. TKA in elderly and with osteoarthritis can yield good results.
References
- 1.Petrie RS, Trousdale RT, Cabanela ME. Total knee arthroplasty for chronic posterior knee dislocation: Report of two cases with technical considerations. J Arthroplasty 2000;15:380-6. [Google Scholar]
- 2.Belmoubarik A, Abouchane M, Fahsi M, Benameur H, Fadili M, Nechad M. Total knee arthroplasty for chronic neglected posterior knee dislocation: Case report and literature review. Open Access Lib J 2015;2:e1976. [Google Scholar]
- 3.Sisto DJ, Warren RF. Complete knee dislocation. A follow-up study of operative treatment. Clin Orthop Relat Res 1985;198:94-101. [Google Scholar]
- 4.Taylor AR, Arden GP, Rainey HA. Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br 1972;54:96-102. [Google Scholar]
- 5.Thomsen PB, Rud B, Jensen UH. Stability and motion after traumatic dislocation of the knee. Acta Orthop Scand 1984;55:278-83. [Google Scholar]
- 6.Henshaw RM, Shapiro MS, Oppenheim WL. Delayed reduction of traumatic knee dislocation. A case report and literature review. Clin Orthop Relat Res 1996;330:152-6. [Google Scholar]
- 7.Karn NK, Khanal GP, Singh MP. Long-standing unreduced anterior dislocation of the knee-a case report. Int J Med Update 2010;5:51-53. [Google Scholar]
- 8.Said HG, Learmonth DJ. Chronic irreducible posterolateral knee dislocation: Two-stage surgical approach. Arthroscopy 2007;23:564.e1-4. [Google Scholar]
- 9.Saini R, Mootha AK, Goni VG, Dhillon MS. Neglected irreducible posterolateral knee dislocation. Indian J Orthop 2010;44:468-70. [Google Scholar]
- 10.Simonian PT, Wickiewicz TL, Hotchkiss RN, Warren RF. Chronic knee dislocation: Reduction, reconstruction, and application of a skeletally fixed knee hinge. A report of two cases. Am J Sports Med 1998;26:591-6. [Google Scholar]
- 11.Van Thiel GS, Baker CL 3rd, Bush-Joseph C. A chronic posterolateral knee and patella dislocation: Case report. J Orthop Trauma 2009;23:541-5. [Google Scholar]
- 12.Nystrom M, Samimi S, Ha’Eri GB. Two cases of irreducible knee dislocation occurring simultaneously in two patients and a review of the literature. Clin Orthop Relat Res 1992;277:197-200. [Google Scholar]
- 13.Chen HC, Chiu FY. Chronic knee dislocation treated with arthroplasty. Injury Extra 2007;38:258-61. [Google Scholar]