Total knee replacement improves patient well-being by managing valgus deformity from severe osteoarthritis, irrespective of age, or deformity.
Prof. Dr. Pervez Ahsan, Professor and Head, Department of Orthopedic Surgery, Ibn Sina Medical College Hospital, Dhaka, Bangladesh. E-mail: pervezahsan60@yahoo.com
Introduction: Valgus deformity is characterized by an outward angulation of the knee joint. The most common cause of valgus deformity is osteoarthritis (OA), a prevalent progressive joint disease that causes chronic pain and functional limitations. Total knee replacement (TKR) is rarely done in patients with grade-I valgus deformity and young age. To the best of our knowledge, this is the first case report of its kind.
Case Report: A 34-year-old man presented to us with 15 years of persistent, progressively worsening right knee pain that was interfering with his daily activities. No non-operative treatment could alleviate his severe pain. Physical examination revealed a positive valgus stress test, limited knee extension, and an asymmetrical gait. He was diagnosed with a grade-I valgus deformity of the right osteoarthritic knee. History, physical examination, and radiological findings confirmed the diagnosis. In consideration of severe pain and impaired quality of life, we opted to perform TKR using a medial parapatellar approach. Regular follow-ups were done after the procedure. He experienced no pain or recurrence of deformity. He was very satisfied with the result. His Western Ontario and McMaster Universities OA Index score at 12 months following surgery was 5, indicating a favorable outcome.
Conclusion: This case exhibits the effectiveness of TKR in treating grade-I valgus deformity of the osteoarthritic knee with severe pain in a young adult, resulting in improved pain alleviation, mobility, joint alignment, and overall quality of life.
Keywords: Valgus deformity, osteoarthritic knee, total knee replacement, medial parapatellar approach.
Valgus knee, also known as knock knee, is a deformity of the knee that occurs when the knee joint angles out and away from the midline of the body. This deformity is referred to as a valgus angle or Q angle [1]. There are several classifications for valgus deformity of the knee, which are usually based on the severity of deformity and soft-tissue involvement. Ranawat’s classification consists of three grades: grade-I (80% of cases) with 6–10° axial deviation, passively correctable, with lateral soft-tissue contracture but no elongation of the medial collateral ligament (MCL); grade-II (15% of cases) with 10–20° axial deviation, contracted lateral structures, and an elongated but functional MCL; grade-III (5% of cases) with an axial deformity exceeding 20°, tight lateral structures, and dysfunctional medial stabilizers [2]. The most common cause of valgus deformity is osteoarthritis (OA); however, post-traumatic arthritis, rheumatoid arthritis, rickets, and renal osteodystrophy can also play a role in the development of a valgus knee [3]. Knee OA comprises a significant portion of the global OA burden and is a common progressive multifactorial joint disease that causes chronic pain and functional impairment, with a higher prevalence in older individuals and those who are obese [4, 5]. The prevalence of knee OA symptoms among young adults is increasing [6]. Globally, the prevalence of knee OA was 16% in those aged ≥15 and 22.9% in those aged ≥40, resulting in approximately 654.1 million individuals (≥40 years) with knee OA in 2020, while the global incidence was 203 per 10,000 person – years for those aged ≥20, resulting in around 86.7 million new cases worldwide in 2020, with prevalence and incidence ratios of 1.69 for females and 1.39 for males [7]. Symptoms of valgus OA knee include knee pain, swelling, stiffness, reduced range of motion, instability, and gait alterations [8, 9]. Physical examinations used for evaluating valgus deformity in an OA knee involve gait analysis, assessment of coronal deformity through valgus and varus stress tests, assessment of sagittal deformity through flexion and extension assessment, anteroposterior laxity testing with the anterior and posterior drawer tests, and the squat test [10]. Radiological evaluation includes X-rays and computed tomography scans [10]. The diagnosis is typically established through the patient’s history and clinical examination, and it can be confirmed further by X-rays [11, 12]. During the early stages of the disease, pain can be alleviated with exercise, weight loss, bracing, physiotherapy, and medication, but surgery becomes required later on [13]. The surgical choices for OA valgus knees consist of bone realignment osteotomies (e.g., HTO), unicompartmental knee replacement, and total knee replacement (TKR) (13). TKR is the pre-eminent surgical choice for knee OA due to its excellent combination of cost-effectiveness and high success rates [14]. Approximately 20% of patients who undergo TKR have a valgus deformity (2). It is typically performed on elderly patients since young patients with long life expectancy face prosthesis longevity issues, requiring revision surgery, and higher demand leading to lower implant survival rates [15]. We discussed a case of a 34-year-old male patient who exhibited an unusual presentation of osteoarthritic knee with grade-I valgus deformity. This case report focuses on the distinct clinical features, diagnostic evaluations, and successful management of TKR in a relatively young adult, resulting in a significant improvement in the patient’s mobility and overall quality of life.
A 34-year-old male patient presented to us with a history of severe right knee pain that had persisted for the past 15 years. The onset of pain was gradual and progressively worsened over time. It was aggravating to do activities such as walking, sitting, squatting, and climbing stairs. Initially, the patient found some relief through rest and analgesics, but these measures were no longer helpful later on. This persistent, severe pain significantly affected his daily activities. He reported a history of multiple joint deformities since birth and underwent a THR on the left hip joint in 2015 due to ankylosing spondylitis. He was non-diabetic and normotensive.
On examination of the right knee, joint line tenderness was present, while the patellar tap for knee effusion was negative, and joint crepitus was absent. Increased intermalleolar distance, indicating asymmetry (Fig. 1). An asymmetrical gait caused by the left equinus foot. The valgus stress test showed a positive result (8°), while the varus stress test was negative. The knee was flexed up to 0–130°, but the extension was limited to 5°. Anterior and posterior drawer tests were negative. The squat test was omitted due to the patient’s history of left-sided THR. The sub-scale score for pain was 11, for stiffness was 3, for physical function was 37. The total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score on presentation was 51. Neurological (sensory) function was intact and systemic examination revealed normal findings. All blood tests performed as part of the pre-operative assessment were within normal ranges, with the exception of HLA B27 detection. X-rays of the right knee were taken from the anterior-posterior (A/P) and lateral views (Fig. 2).
Pre-operative X-ray (Fig. 2) findings, including both A/P and lateral views, revealed significant degenerative changes. The A/P view revealed reduced joint space, along with medial condyle sloping and reverse sloping of the proximal tibia, indicating altered alignment. The lateral view indicated significant osteoarthritic changes including complete articular destruction on the lateral condyle and evident fragmentation of the patellar articular surface.
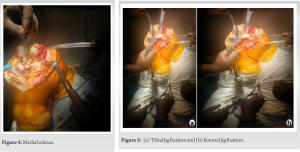
TKR was executed under a subarachnoid block and with strict aseptic precautions (Fig-. 3a). We employed a medial parapatellar approach. Arthrotomy was performed just medial to the patellar tendon (Fig-.3b). Following the medial release, the patella was dislocated laterally (Fig. 4). 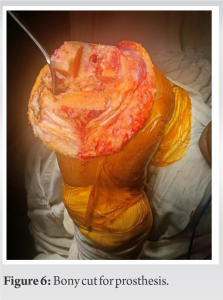
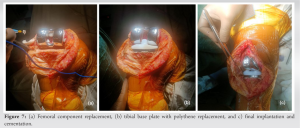
During the femoral bone cut, the medial condyle was found hypoplastic and underdeveloped, and a huge bone cyst was detected, raising worries about potential bone loss and further complications. To resolve this issue, the cyst was meticulously removed and no bone cut was done medially. In addition, the reverse slope of the tibial upper end further complicates the surgical procedure. Due to the increased risk of injuring posterior blood vessels and nerves, we avoided the posterior bone cut of the tibia. To mitigate these risks and adjust the alignment appropriately, a cautious approach was taken, necessitating a more precise and deliberate bone cut. During the fixation of the tibial tray, the bone of the upper tibia was found osteoporotic, and due to this, a tibial extender was used to prevent further periprosthetic fracture.
The patient had a successful post-operative course and was released on the 5th day following TKR. Oral analgesics and physiotherapy facilitated a progressive recovery. Initially, the patient used a walker for non-weight-bearing ambulation, then progressed to crutches, and ultimately to independent walking without assistance. Following surgery, the patient experienced a progressive return to regular daily activities, with no recurrence of the valgus deformity. Of 12 months following surgery, the sub-scale score for pain was 0, for stiffness was 0, for physical function was 5. The total WOMAC score was 5, suggesting significant improvement. Furthermore, post-operative X-rays of the right knee acquired from both A/P and lateral views revealed that the mechanical axis was maintained and there was no loosening of the implant (Fig. 8), confirming the successful outcome of the procedure.
Different studies have provided various kinds of results. Usually, TKR is not done at a young age. Julin et al. found that TKR survival rates were 92% in patients aged ≤ 55, W-Dahl et al. similarly, interrogated the Swedish Register, which shows a 9% revision rate for patients under aged 55, Odland et al. studied 59 active patients aged 55 years or younger, finding 16% underwent revisions [16-18]. However, we performed TKR on a 34-year-old young male. While Ranawat’s classification suggests that grade-I valgus deformities are passively correctable [2], but we performed TKR for a grade-I valgus (8°) deformity in a 34-year-old male due to severe OA-related pain in the right knee. Ismailidis et al. reported a TKR case of a 90-year-old female with grade III valgus arthritis, having a valgus angle of 47° [19]. A study by Utomo et al. reported a 71-year-old female patient with grade III valgus (32°) arthritis who underwent TKR [20]. Triangga et al. performed TKR on a 56-year-old female with a grade-III (48°) valgus knee and a 62-year-old male with a grade-II (13°) valgus knee experiencing painful OA [21]. In our study, we observed knee flexion reaching 130°, with a limited extension of 5°, whereas Ismailidis et al. reported a maximal flexion of 100° and an extension deficit of 15° [19]. Utomo et al. noted a limited right knee range of motion from 10° to 145° of flexion [20]. In addition, Triangga et al. found a restricted right knee range of motion of 0–70° in a 56-year-old female with grade-III valgus deformity and 0–90° in a 62-year-old male with grade-II valgus deformity [21]. All the referenced studies [19-21], including our own, performed TKR in the medial parapatellar approach. The WOMAC score was first published by Bellamy and Buchanan in 1988 [22]. It is commonly used in outcome measures for hip and knee OA that consists of 24 questions divided into three categories: Pain (5 questions), stiffness (2 questions), and physical function (17 questions) [19, 22]. The instrument is available in 5-point Likert scale, 100-mm VAS, and 11-box numerical rating scale forms [22]. None (0), mild (1), moderate (2), severe (3), and extreme (4) are the options on the 5-point Likert scale [22]. The sub-scale scores can range from 0 to 20 points for pain, 0 to 8 points for stiffness, and 0 to 68 points for physical function. In this rating system, higher scores represent worse pain, stiffness, and functional limitations on a scale of 0–96 [22]. In our study, we identified a pre-operative WOMAC score of 51, which significantly improved to 5 after the intervention. Conversely, Ismailidis et al. reported a notably higher pre-operative WOMAC score of 91, which saw a reduction to 45 postoperatively [19]. At a 10–15-year follow-up, revision rates following TKR for valgus deformity in knee OA were reported to be between 0% and 17% [10, 23, 24]. Significant pre-operative deformity or poor surgical correction has been associated with a higher failure rate [25]. All the referenced studies [19, 20, 21], including our own, demonstrated favorable post-operative outcomes, resulting in improved patient mobility and overall quality of life.
Although TKR is uncommon in young adults with grade-I deformity, our case of TKR in a 34-year-old male with grade-I valgus deformity due to severe osteoarthritic pain highlights the effectiveness of the TKR. It demonstrates that TKR is a successful intervention, significantly improving pain relief, mobility, joint alignment, and overall quality of life in such cases.
TKR is effective in treating valgus deformity caused by severe OA, improving pain relief, mobility, joint alignment, and overall quality of life for patients of all ages and grades, though there is a chance of some adverse outcomes.
References
- 1.Lotke PA, Lonner JH. Master Techniques in Orthopaedic Surgery: Knee Arthroplasty. 3rd ed. United States: Lippincott Williams and Wilkins; 2012. [Google Scholar]
- 2.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 2005;87:271-84. [Google Scholar]
- 3.Nikolopoulos D, Michos I, Safos G, Safos P. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop 2015;6:469-82. [Google Scholar]
- 4.Vos T, Allen C, Arora M. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1545-602. [Google Scholar]
- 5.Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019;27:1578-89. [Google Scholar]
- 6.National Collaborating Centre for Chronic Conditions (UK). Osteoarthritis: National Clinical Guideline for Care and Management in Adults. London: Royal College of Physicians (UK); 2008. [Google Scholar]
- 7.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine 2020;29-30:100587. [Google Scholar]
- 8.Eustice C. Valgus vs. Varus Knee Alignments: What are the Differences? Verywell Health; 2008, https://www.verywellhealth.com/what-is-varus-or-valgus-knee-deformity-2552048. [Google Scholar]
- 9.Qasımov E. Causes of Knee Deformities and Their Treatment. Dr Elviz Qasımov; 2022, https://elvizgasimov.com/en/causes-of-knee-deformities-and-their-treatment/. [Google Scholar]
- 10.Apostolopoulos AP, Nikolopoulos DD, Polyzois I, Nakos A, Liarokapis S, Stefanakis G, et al. Total knee arthroplasty in severe valgus deformity: Interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop Traumatol Surg Res 2010;96:777-84. [Google Scholar]
- 11.Knee Osteoarthritis. Physiopedia. Knee Osteoarthritis, Physiopedia, https://www.physio-pedia.com/Knee_Osteoarthritis [Google Scholar]
- 12.Valgus knee. Physiopedia. https://www.physio-pedia.com/Valgus_Knee [Google Scholar]
- 13.Liu W, Lin B, Zhang X, Zhou T, Liu W, Wang L, et al. The effect of femoral component valgus/varus angle on the mid-term efficacy of unicondylar knee arthroplasty. Biotechnol Genet Eng Rev 2023;Mar 10 1-14. [Google Scholar]
- 14.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: A systematic review. Can J Surg 2008;51:428. [Google Scholar]
- 15.Sutton PM, Holloway ES. The young osteoarthritic knee: Dilemmas in management. BMC Med 2013;11:14. [Google Scholar]
- 16.Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis: A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop 2010;81:413-9. [Google Scholar]
- 17.W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients: A Swedish register study. Acta Orthop 2010;81:161-4. [Google Scholar]
- 18.Odland AN, Callaghan JJ, Liu SS, Wells CW. Wear and lysis is the problem in modular TKA in the young OA patient at 10 years. Clin Orthop Relat Res 2011;469:41-7. [Google Scholar]
- 19.Ismailidis P, Kernen R, Mueller SA. Total knee arthroplasty in severe Valgus osteoarthritis excellent early results in a 90-year-old patient with a Valgus deformity of 47. Case Rep Orthop 2017;2017:9301017. [Google Scholar]
- 20.Utomo DN, Mahyudin F, Yanuar A, Widhiyanto L, Hernugrahanto KD. Correction of severe valgus deformity of knee osteoarthritis with non-constrained total knee arthroplasty implant: A case report. Int J Surg Case Rep 2018;53:218-22. [Google Scholar]
- 21.Triangga AF, Magetsari RM, Purnomo G, Rahmansyah N, Riyadli M, Sibarani T. A case series of total knee arthroplasty with a non-constrained implant in 2nd and 3rd degree valgus deformity in knee osteoarthritis and medial collateral ligament insufficiency. Int J Surg Case Rep 2023;106:108162. [Google Scholar]
- 22.Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol 1986;5:23141. [Google Scholar]
- 23.Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe Valgus deformity: Five to fourteen-year follow-up. J Bone Joint Surg Am 2004;86:2671-6. [Google Scholar]
- 24.Rajgopal A, Dahiya V, Vasdev A, Kochhar H, Tyagi V. Long-term results of total knee arthroplasty for Valgus knees: Soft-tissue release technique and implant selection. J Orthop Surg (Hong Kong) 2011;19:60-3. [Google Scholar]
- 25.Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, et al. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 2013;95:126-31. [Google Scholar]