Navigable percutaneous disc decompressor (L’DISQ-C) is safe, precise, less invasive, and effective in the treatment of symptomatic contained cervical disc herniations.
Dr. Ji Soo Ha, Yonsei Okay Hospital, Seoul, South Korea. E-mail: raj.sakhrekar1@gmail.com
Introduction: A new navigable percutaneous disc decompressor (L’DISQ-C, U&I Co., Uijeongbu, Korea), introduced in 2012, is designed to allow direct access to herniated disc material. The L’DISQ device can be curved by rotating a control wheel, directed into disc herniation treats, and decompresses contained herniated discs with minimal collateral thermal damage. This study reports the case of contained central disc herniation in a 34-year-old male with a 2-year follow-up successfully treated with navigable ablation decompression treatment (L-DISQ).
Case Report: A 34-year-old man presented to the outpatient department with a 6-month history of neck pain and bilateral upper limb radiation. His neck pain had increased progressively. At the time of presentation, his neck pain visual analog scale score was 7/10, and his neck disability index score was 30. The magnetic resonance images showed a single fluid-containing lesion with a hyperintense zone at the C4–5 levels with central disc herniation. The patient was successfully treated with the navigable ablation decompression treatment (L-DISQ) procedure.
Conclusion: The navigable ablation decompression treatment (L-DISQ) is a valuable technique in treating contained cervical disc herniation with rapid pain relief and improvements in functional outcomes without any significant injury to surrounding structures. It is safe, precise, and effective in the treatment of symptomatic cervical disc herniations. Large, randomized, and multicenter trials are needed to explore the potential of the same technique further.
Keywords: L-DISQ-C, visual analog scale score, neck disability index score, minimally invasive spine surgery.
Nucleoplasty was introduced in 1999 for decomposing lumbar disc herniation using a posterior lateral approach with minimal collateral thermal damage (ArthroCare Co., Sunnyvale, CA). It uses a bipolar radiofrequency technology applied to a saline conducting medium, which vaporizes nuclear tissue, helping in the removal of herniated disc tissue. The primary disadvantage of the nucleoplasty device is the inability to access the herniated nucleus easily, limiting the direct removal of herniated disc tissue [1, 2]. A new navigable percutaneous disc decompressor (L’DISQ-C, U&I Co., Uijeongbu, Korea), introduced in 2012, is designed to allow direct access to herniated disc material. The L’DISQ device can be curved by rotating a control wheel, directed into disc herniation treats, and decompresses contained herniated discs with minimal collateral thermal damage [2, 3, 4, 5]. This study reports the case of contained central disc herniation in a 34-year-old male with a 2-year follow-up successfully treated with navigable ablation decompression treatment (L-DISQ).
A 34-year-old man presented to the outpatient department with a 6-month history of neck pain and bilateral upper limb radiation. His neck pain had increased progressively. At the time of presentation, his neck pain visual analog scale (VAS) score was 7/10, and his neck disability index (NDI) score was 30. He had received non-steroidal anti-inflammatories for more than 6 months and an epidural injection elsewhere with minimal relief from symptoms. On physical examination, power in all limbs was 5/5 as per the medical research council grading, and deep tendon reflexes were normal, too. The past, personal, addiction, or familial history was not significant. The magnetic resonance images showed a single fluid-containing lesion with a hyperintense zone at the C5–6 levels with central disc herniation (Fig. 1).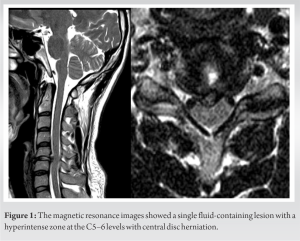
The procedure is performed under local anesthesia using lidocaine over the anterior cervical region, with monitored vital signs by an anesthesiologist. The patient was awake throughout the process and conversed with the team, giving input about the pain responses. The patient was positioned supine on a radiolucent table with the neck extended by placing a cushion beneath the shoulder and soft cushion support behind the neck. The anterior cervical region is prepped and draped in a sterile fashion. An aseptic technique must be used throughout the procedure. The target disc and appropriate skin site to needle trajectory are confirmed with fluoroscopic examination. The port cannula was placed into the right side through the midline through an anterolateral approach. Since the esophagus is on the left of the midline, a right-sided approach seems relatively safer, especially at lower cervical levels. Tight pressure was applied to the space between the trachea and the medial border of the sternocleidomastoid muscle to remove the trachea from the midline in a controlled manner. The middle and index fingers sensed the carotid artery to determine the entry point while preventing possible vascular injury and hematoma. In case of accidental complications, tampon pressure in case of hematoma and daily abundant fluid intake, additional caffeine-containing painkiller agent, IV hydration, and epidural blood patch were planned to treat the headache due to dural injury. The cannula was moved obliquely into the intervertebral disc area 3–4 cm away from the midline at the index level. The C-arm was placed to obtain a lateral view of the surgical field, and then, the cannula and trunk were advanced into the disc under fluoroscopic guidance. If both the anteroposterior and lateral views were located in the target area, a short test of electrical stimulation was performed by connecting the L’DISQ-C wand to the power generator to check the position of the cannula and to assess that the cannula was not near neural structures, which helps to prevent possible neural tissue damage(Fig. 2).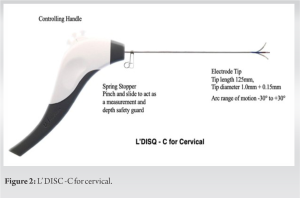
The patient’s pain and symptoms improved on post-procedure days 1, 2 weeks, one month, and six months. There was rapid pain relief on day 1, and VAS enhanced from 7 to 1. MRI done post-operatively on day 2 demonstrated significant disc decompression of the herniated disc. The VAS score was 0 at the 6-month follow-up, and the NDI improved from 30 to 3. These results were maintained at a 2-year follow-up with a telephone conversation. Patient satisfaction was surveyed using Odom’s criteria at each follow-up visit (at 1 week, 1 month, 6 months, and 2 years) and was found to be excellent. These cases demonstrated no early or late complications regarding neurologic deficits, infection, or epidural hematomas.
Over the last five to six decades, spine surgeons have strived to find less invasive procedures for treating patients with CDH, a midterm alternative treatment between conservative management and spine surgery. Various interventional techniques were used with variable success, which include chemonucleolysis, ozone, automated percutaneous lumbar discectomy, intradiscal laser discectomy, intradiscal electrothermal therapy, and percutaneous nucleoplasty [6, 7, 8, 9, 10]. Percutaneous procedures gathered all the interest due to their advantages, such as the lesser threat of secondary tissue damage, operability with local anesthesia, avoidance of the risks associated with general anesthesia, benefits in patients with severe co-morbidities, and earlier discharge. A newly available L’DISQ device is a navigable percutaneous decompression device that can be curved by rotating a control wheel and directed into the base of disc herniation in the posterior annulus fibrosus, helps to pass an electric current through the wand, heats the tissues surrounding the tip, and decompresses contained herniated discs with minimal collateral thermal damage(Fig. 3). 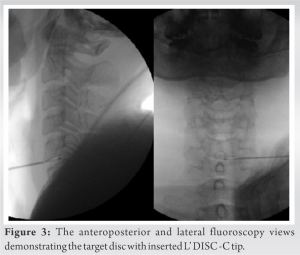
Potential complications associated with the procedure include esophageal, vascular, or neural injuries; hoarseness; Horner syndrome; infections; leakage of cerebrospinal fluid; neurological damage; increase in pain; muscle spasm; and retrosternal and retropharyngeal pain. Lee et al. in 2013 [2] reported successful outcomes with a reduction of VAS by more than 50% at 1-year follow-up. However, the need for a control group and a small sample size were limitations of the study. They concluded that patients with both cervical radicular and axial pain caused by protruded and extruded discs treated with L’DISQ-C had clinically significant pain improvement and decreased disability for patients.
Ceylan and Aşik in 2019 [17] concluded that L-DISQ provided better pain control than percutaneous disc coagulation therapy in the early period, while both methods were found to have similar effectivity in the long term.
The navigable ablation decompression treatment (L-DISQ) is a valuable technique in treating contained cervical disc herniation with rapid pain relief and improvements in functional outcomes without any significant injury to surrounding structures. It is safe, precise, and effective in the treatment of symptomatic cervical disc herniations. Large, randomized, and multicenter trials are needed to explore the potential of the same technique further.
Navigable percutaneous disc decompressor (L’DISQ-C) is safe, precise, less invasive, and effective in the treatment of symptomatic contained cervical disc herniations.
References
- 1.Chen CH, Chiu YP, Ji HR, Wu CY, Guo JH, Jaw FS, et al. Analysis of the clinical and radiological outcomes of percutaneous cervical nucleoplasty: A case-control study. PLoS One 2022;17:e0278883. [Google Scholar]
- 2.Lee SH, Derby R, Sul DG, Hong JW, Kim GH, Kang S, et al. Efficacy of a new navigable percutaneous disc decompression device (L’DISQ) in patients with herniated nucleus pulposus related to radicular pain. Pain Med 2011;12:370-6. [Google Scholar]
- 3.Hong YK, Derby R, Wolfer LR, Kim SU, Kang BS, Kim NH, et al. An assessment of a new navigatable percutaneous disc decompression device (l’DISQ) through histologic evaluation and thermo-mapping in human cadaveric discs. Pain Med 2012;13:1000-3. [Google Scholar]
- 4.Lee SH, Derby R, Sul D, Hong YK, Ha KW, Suh D, et al. Effectiveness of a new navigable percutaneous disc decompression device (L’DISQ) in patients with lumbar discogenic pain. Pain Med 2015;16:266-73. [Google Scholar]
- 5.Hong Y, Yoo S, Kim NH, Kim Y, Sohn S, Yoon SY, et al. Feasibility of navigable percutaneous disk decompressor (L’DISQ-C) for cervical disk herniation. J Neurol Surg A Cent Eur Neurosurg 2018;79:231-8. [Google Scholar]
- 6.Singh V, Benyamin RM, Datta S, Falco FJ, Helm S, Manchikanti L. Systematic review of percutaneous lumbar mechanical disc decompression utilizing Dekompressor®. Pain Physician 2009;12:589-99. [Google Scholar]
- 7.Pandolfi M, Galli F, Borelli A, Gurgitano M, Liguori A, Carrafiello G. Percutaneous cervical coblation as therapeutic technique in the treatment of algo-dysfunctional pain of discal herniation. Radiol Med 2021;126:860-8. [Google Scholar]
- 8.Manchikanti L, Singh V, Falco FJ, Calodney AK, Onyewu O, Helm S, et al. An updated review of automated percutaneous mechanical lumbar discectomy for the contained herniated lumbar disc. Pain Physician 2013;16:SE151-84. [Google Scholar]
- 9.Hong Y, Yoon SY, Sohn S, Kim NH, Kim Y, Lee S. Evaluation of the resection efficiency and safety of an enhanced power plasma generator using cadaveric intervertebral discs. Biomed Eng Lett 2023;13:57-64. [Google Scholar]
- 10.Lee MY, Boudier-Revéret M, Cho HK, Chang MC. The successful treatment of herniated lumbar discs that are refractory to repeated epidural steroid injection by using a navigable percutaneous disc decompression device: A case series. J Pain Res 2020;13:1869-73. [Google Scholar]
- 11.Case RB, Choy DS, Altman P. Change of intradisc pressure versus volume change. J Clin Laser Med Surg 1995;13:143-7. [Google Scholar]
- 12.Ranu HS. Multipoint determination of pressure-volume curves in human intervertebral discs. Ann Rheum Dis 1993;52:142-6. [Google Scholar]
- 13.O’Neill CW, Liu JJ, Leibenberg E, Hu SS, Deviren V, Tay BK, et al. Percutaneous plasma decompression alters cytokine expression in injured porcine intervertebral discs. Spine J 2004;4:88-98. [Google Scholar]
- 14.Kuelling FA, Foley KT, Liu JJ, Liebenberg E, Sin AH, Matsukawa A, et al. The anabolic effect of plasma-mediated ablation on the intervertebral disc: Stimulation of proteoglycan and interleukin-8 production. Spine J 2014;14:2479-87. [Google Scholar]
- 15.Kim NH, Hong Y, Lee SH. Two-year clinical outcomes of radiofrequency focal ablation using a navigable plasma disc decompression device in patients with lumbar disc herniation: Efficacy and complications. J Pain Res 2018;11:2229-37. [Google Scholar]
- 16.Goupille P, Mulleman D, Mammou S, Griffoul I, Valat JP. Percutaneous laser disc decompression for the treatment of lumbar disc herniation: A review. Semin Arthritis Rheum 2007;37:20-30. [Google Scholar]
- 17.Ceylan A, Aşik İ. Percutaneous plasma laser disc coagulation and navigable ablation decompression in the treatment of cervical disc herniation: A single center experience. Turk J Med Sci 2019;49:258-64. [Google Scholar]











