Clinicians should keep infection in mind when treating patients with neck pain.
Dr. Jun Tanaka, Department of Orthopaedics, Fukuoka University Faculty of Medicine, 7-45-1 Nanakuma Jonan-ku, Fukuoka 814-0180, Japan. E-mail: jt0120jt@gmail.com
Introduction: There are few reports of cases with vertical subluxation. We report our experience of a vertical subluxation of the atlantoaxial joint caused by infection.
Case Report: A 63-year-old man had a 5-month history of neck pain. He was treated for rheumatoid arthritis by a local doctor. At admission to our hospital, he had neck pain and complained of dysphagia and hoarseness. His white blood cell count and C-reactive protein were 7200/mm3 and 4.86 mg/dL. Cervical X-ray showed atlantoaxial subluxation. Computed tomography showed osteolysis around the odontoid process, including the atlantooccipital and atlantoaxial joints, causing vertical subluxation. Magnetic resonance imaging showed spinal cord and brainstem compression and the presence of fluid. Gadolinium-enhanced magnetic resonance imaging showed enhancement around the odontoid process. We performed occipital-cervical spine fixation and C1 laminectomy. Following surgery, his symptoms completely resolved. Bone fusion was confirmed 6 months after surgery.
Conclusion: If subluxation of the upper cervical spine occurs rapidly, infection should be considered.
Keywords: Atlantoaxial vertical subluxation, pyogenic spondylitis, atlantoaxial joint, atlantooccipital joint.
Spinal infections are devastating diseases associated with high mortality when not correctly diagnosed. Osteomyelitis of the cervical spine is rare compared with infections of the thoracic and lumbar spine. Malawski and Lukawski reported that cervical spondylitis accounts for 5.8% of all spinal infections, while infections of the upper cervical spine have an even lower incidence (0.7%) [1]. There are several reports of atlantoaxial subluxation (AAS) due to infection around the odontoid process [2-4]. However, there are few reported cases with vertical subluxation (VS). Patients with VS are at risk of death due to compression of the dentary process on the brainstem [5]. Herein, we report a case of VS due to infection around the odontoid process, resulting in bulbar paralysis.
The patient provided informed consent for publication of these findings. A 63-year-old-man with a chief complaint of neck pain was examined at a local hospital. No neurological symptoms were observed. A cervical X-ray showed only degenerative findings (Fig. 1) and no instability, and he was treated conservatively for cervical osteoarthritis. However, his neck pain persisted after 1 month and computed tomography (CT) showed an AAS. Laboratory examinations were negative for rheumatoid factor and anti-cyclic citrullinated peptide antibodies, although C-reactive protein and matrix metalloproteinase were mildly elevated. A blood culture test was also negative. Due to his family history of rheumatoid arthritis (RA) (his daughter had RA) and the presence of an AAS, he was treated with steroids and methotrexate for seronegative RA. However, his symptoms did not improve. He was referred to our hospital at 4 months after his first visit because of the progression of AAS and the appearance of bulbar paralysis. At admission to our hospital, his body temperature was 36.1°C. He had pain from the occiput to the neck, although his neurological findings were normal (normal muscle strength, normal limb tendon reflexes, and no numbness in the extremities). He also complained of dysphagia, particularly with difficulty swallowing solid food, and had hoarseness. His white blood cell count and C-reactive protein were 7200/mm3 and 4.86 mg/dL, respectively.
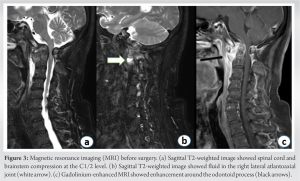
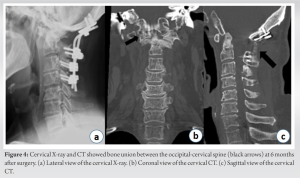
The lateral view of the cervical X-ray showed AAS, while CT showed osteolysis around the odontoid process, including the atlantooccipital and atlantoaxial joints, causing VS (Fig. 2). Magnetic resonance imaging (MRI) showed spinal cord and brainstem compression at the C1/2 level and fluid in the right lateral atlantoaxial joint on a T2-weighted image. Gadolinium-enhanced MRI showed enhancement around the odontoid process (Fig. 3). A blood culture test was performed again and methicillin-sensitive staphylococcus aureus was detected. We concluded that the AAS and VS were caused by infection around the odontoid process and surgical treatment was indicated.
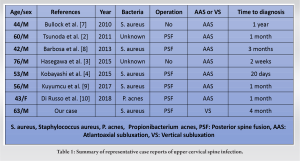
We performed occipital-cervical (O-C4) spine fixation and C1 laminectomy. The patient’s head was immobilized with a Mayfield skull clamp and the head was tractioned, retroflexed, and aligned while viewing X-ray fluorography. During surgery, we confirmed free-running electromyography using motor-evoked potentials and ensured that the spinal cord was not overloaded. We also biopsied the right lateral atlantoaxial joint and performed a culture test, which detected methicillin-sensitive staphylococcus aureus. Thus, the patient was administered intravenous cefazolin (6 g/day) after surgery. His neck pain and dysphagia improved immediately after surgery and he was able to swallow solid food. His hoarseness also improved and his inflammatory response completely resolved. X-ray and CT showed bone union between the O-C4 spine at 6 months after surgery (Fig. 4).
Osteomyelitis of the cervical spine is rare, while infections of the upper cervical spine have an even lower incidence (0.7%) [1]. In 1896, Makins and Abbott first reported two cases of odontoid osteomyelitis [6], while there are several reports of AAS due to infection around the odontoid process [2-4]. A summary of representative case reports is shown in Table 1 [2-4,7-10]. Most patients had AAS; to the best of our knowledge, no reports have described VS. In addition, most of the previously described patients had a shorter time from onset to diagnosis than our patient, suggesting that delayed diagnosis may be a risk factor for progression to VS. Early diagnosis and treatment of VS are important because when a patient develops VS, the neurological prognosis is worse than AAS and there is a risk of death due to compression of the dentary process on the brainstem [5, 11]. In general, AAS is thought to occur in RA, trauma, and congenital diseases, and is particularly common in RA patients. As AAS progresses to VS when the lateral atlantoaxial or atlantooccipital joint is destroyed [12], AAS or VS is often considered a result of RA. Nevertheless, Zhang et al. reported rates of progression of AAS, VS, and subaxial subluxation of four, six, and three lesions per 100 patients per year in RA patients, while the incidence of new or progressive cervical myelopathy was two cases per 100 patients with known cervical subluxations per year [13]. These findings suggest that AAS and VS are unlikely to progress rapidly in RA patients. Thus, if subluxation of the upper cervical spine occurs rapidly, other causes should be considered.
Non-traumatic AAS associated with inflammatory conditions of the upper cervical spine, especially secondary to inflammation of the otolaryngological region, is termed Grisel’s syndrome – this condition was first reported by Bell in 1830 and named by Grisel in 1930. The most widely accepted mechanism of Grisel’s syndrome is hyperemia following infection or trauma that leads to decalcification of the anterior arch of C1 and laxity of the transverse ligament [14]. In addition, Parke et al. reported that the upper cervical spine may be infected by congestion and effusion from the lymph and veins in the posterior pharynx. In that study, the authors also suggested that this condition is more common in children because the upper spine is more mobile than in adults and they have a hypertrophic status of the parapharyngeal lymphoid tissue, which is located in the area drained by the pharyngovertebral plexus [15]. In the present case, there were no fever or pharyngeal symptoms before the onset of neck pain. In addition, the patient had no history of trauma and had a family history of RA, which led to a false diagnosis and treatment with steroids – this may have also contributed to the progression of AAS and VS. These subluxations, which are caused by infection around the odontoid process, are very serious conditions because they can lead to paraplegia and death due to cervical cord and brainstem compression [5,7]. Therefore, early diagnosis is critical. However, diagnosis can sometimes be very difficult because these subluxations are caused by numerous factors, including RA, trauma, and congenital diseases, and have no specific clinical signs. In addition, the symptoms are varied and nonspecific, and can present with normal inflammatory markers [9]. In addition to careful physical examinations, imaging assessment is important for the diagnosis of AAS and VS. In the early stages of infection, radiographs are often normal. By contrast, MRI can be used to evaluate both the presence of spinal cord compression and osteomyelitis and soft tissues around the odontoid process. CT is also useful in differentiating crystal-induced arthritis. There is no consensus on the surgical strategy for osteomyelitis of the upper cervical spine. Ueda et al. reported that an accurate diagnosis is the most important step and that antibiotic treatment should be administered if the infection is in the early stages. If the patient is resistant to antibiotic treatment, or if neurological deficits, subluxation, or malalignment occur, then surgical treatment should be performed [16]. Our patient’s treatment was delayed by 5 months because of misdiagnosis. An early and accurate diagnosis of infection around the odontoid process would have likely avoided the requirement for surgical treatment.
We experienced a case of vertical subluxation of the atlantoaxial joint caused by infection with a 5-month delay in treatment. The neck pain and bulbar paralysis were successfully treated with O–C4 spine fixation. Clinicians should consider the potential for infection when treating patients with neck pain.
If we see a patient with long-lasting neck pain, we should also keep in mind infection of the upper cervical spine. In particular, we should be aware that there are cases of rapid progression of subluxation of the atlantoaxial joint.
References
- 1.Malawski SK, Lukawski S. Pyogenic infection of the spine. Clin Orthop Relat Res 1991;272:58-66. [Google Scholar]
- 2.Tsunoda K, Iizuka H, Sorimachi Y, Ara T, Nishinome M, Takechi Y, et al. Atlanto-axial subluxation after pyogenic spondylitis of the atlanto-occipital joint. Eur Spine J 2011;20 (Suppl 2):S253-7. [Google Scholar]
- 3.Hasegawa A, Yagi M, Takemitsu M, Machida M, Asazuma T, Ichimura S. Atlantoaxial Subluxation after Pyogenic Spondylitis around the Odontoid Process. Case Rep Orthop 2015;2015:861403. [Google Scholar]
- 4.Kobayashi T, Miyakoshi N, Abe E, Abe T, Kikuchi K, Shimada Y. Acute neck pain caused by septic arthritis of the lateral atlantoaxial joint with subluxation: A case report. J Med Case Rep 2015;9:171. [Google Scholar]
- 5.Kaito T, Hosono N, Ohshima S, Ohwaki H, Takenaka S, Fujiwara H, et al. Effect of biological agents on cervical spine lesions in rheumatoid arthritis. Spine 2012;37:1742-6. . [Google Scholar]
- 6.Makins GH, Abbott FC. On acute primary osteomyelitis of the vertebrae. Ann Surg 1896;23:510-39 [Google Scholar]
- 7.Bullock R, Soares DP, James M. An infected branchial cyst complicated by retropharyngeal abscess, cervical osteomyelitis and atlanto-axial subluxation. BMJ Case Rep 2010;2010:bcr0420102933. [Google Scholar]
- 8.Barbosa TR, Pereira PM, Silva PS, Monteiro PM, Vaz RM. Osteomyelitis of the Atlanto occipital joint in an intravenous drug user: A case report and review of the literature. JBJS Case Connect 2013;3:e101. [Google Scholar]
- 9.Kuyumcu G, Simpfendorfer CS, Babic M, Kalfas IH, Teixeira-Johnson L, Winalski CS. Septic arthritis of an atlantoaxial facet joint with normal inflammatory markers: Case report and literature review. World Neurosurg 2017;98:870.e11-5. [Google Scholar]
- 10.Di Russo P, Tascini C, Benini ME, Martini C, Lepori P. C1-C2 arthrodesis after spontaneous Propionibacterium acnes spondylodiscitis: Case report and literature analysis. Surg Neurol Int 2018;9:14. [Google Scholar]
- 11.Shen FH, Samartzis D, Jenis LG, An HS. Rheumatoid arthritis: Evaluation and surgical management of the cervical spine. Spine J 2004:4:689-700. [Google Scholar]
- 12.Lipson SJ. Rheumatoid arthritis in the cervical spine. Clin Orthop Relat Res 1989;239:121-7. [Google Scholar]
- 13.Zhang T, Rope J. Cervical spine involvement in rheumatoid arthritis over time: Results from a meta-analysis. Arthritis Res Ther 2015;17:148. [Google Scholar]
- 14.Youssef K, Daniel S. Grisel syndrome in adult patients. Report of two cases and review of the literature. Can J Neurol Sci 2009;36:109-13. [Google Scholar]
- 15.Parke WW, Rothman RH, Brown MD. The pharyngovertebral veins: An anatomical rationale for Grisel’s syndrome. J Bone Joint Surg Am 1984;66:568-74. [Google Scholar]
- 16.Ueda Y, Kawahara N, Murakami H, Matsui T, Tomita K. Pyogenic osteomyelitis of the atlas: A case report. Spine 2009;34:E342-5. [Google Scholar]