Achieving optimal outcomes in fibrous dysplasia-related femoral shaft fractures requires a meticulous approach. Correcting The correction of the neck-shaft angle is prioritized takes precedence, with Seekh kebab osteotomy addressing to rectify the shaft deformities. In addition, the double-angled Dynamic Compression Screw (DCS) offers versatility for secure fixation of femoral neck fractures. Understanding these interventions is crucial for successful alignment restoration and fracture management in fibrous dysplasia cases, emphasizing a comprehensive strategy for favorable patient outcomes.
Dr. Dheeraj Makkar, Department of Orthopaedics, NC Medical College, Panipat, Haryana, India. E-mail: makkardheeraj@gmail.com
Introduction: Fibrous dysplasia (FD) is a benign skeletal disorder characterized by the replacement of normal bone tissue with disorganized fibrous tissue. Fractures are a significant complication of FD, particularly in the proximal femur, where deformities such as Shepherd’s crook deformity can increase the risk.
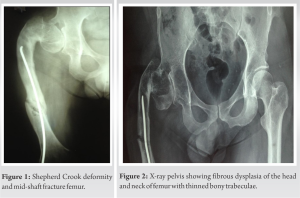
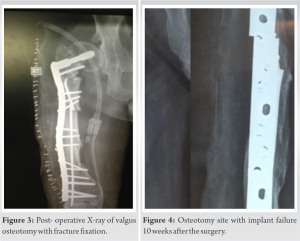
Case Report: We present a case study of a 44-year-old male with unilateral monostotic FD, Shepherd’s crook deformity, and a pathological femoral shaft fracture. The initial surgical approach involved valgus osteotomy, dynamic condylar screw (DCS) fixation, and multiple osteotomies of the femoral shaft. However, the patient experienced a refracture and implant failure, necessitating a second surgical intervention with a double-angled DCS and additional fixation. Post-operative follow-up revealed successful bone union and deformity correction, although a limb length discrepancy was noted.
Conclusion: This case highlights the challenges in managing FD-related fractures and the importance of addressing deformities and achieving optimal alignment. Individualized treatment approaches, careful implant selection, and post-operative rehabilitation are crucial for successful outcomes in FD-associated fractures.
Keywords: Fibrous dysplasia, femur, dynamic condylar screw, shepherd crook.
Fibrous dysplasia (FD) is a benign skeletal disorder that constitutes approximately 5–7% of all tumors [1]. It is characterized by the replacement of normal osseous tissue with disorganized and immature fibrous tissue [2, 3]. Impaired bone remodeling mechanisms underlie the pathogenesis of FD, resulting in inadequate mineralization of the affected bone [2, 3]. FD manifests in two distinct forms: monostotic, which affects a single bone, and polyostotic, which affects multiple bones. Despite differences in clinical presentation, both types exhibit comparable histological characteristics [4]. The development of FD is associated with a genetic mutation in the GNASI gene on chromosome 20 [4]. The monostotic subtype, commonly detected during initial diagnosis, is the most prevalent form of FD, primarily observed in children or young adults [4]. Dheenadhayalan et al. have extensively detailed the treatment approach for FD cases featuring Shepherd’s crook deformity accompanied by a femoral neck fracture [5]. We present a case study of a 44-year-old male with unilateral monostotic FD, exhibiting Shepherd’s crook deformity and a pathological fracture of the femoral shaft, along with the implant in situ. The treatment approach involved the implementation of a single-stage valgus osteotomy combined with a dynamic condylar screw (DCS) and multiple osteotomies of the femoral shaft to correct the deformity. However, the patient experienced a fracture recurrence at the osteotomy site, along with implant failure. Consequently, a second surgical procedure was performed; we fixed the fracture with a double-angled DCS and reinforced the osteotomy sites with an additional implant. The objective of this approach was to effectively address the deformity and achieve proper stabilization of the fractured bone [5].
The patient reported to us in 2017 and complained of persistent and worsening pain localized in the right thigh area of the region for 3 days. There was no history of trauma but a sudden giveaway while walking with support with a caliper, leading to severe pain. The pain, described as sharp and shooting, was aggravated by weight-bearing activities and worsened at night. On physical examination of the right lower limb, localized swelling, tenderness, shortening, external rotation, and crepitus in the right thigh were observed. In addition, shepherd crook deformity of the right femur was observed.
In December 2008, the patient experienced a right femur fracture in Vadodara, Gujarat, managed with external fixation and healed within a few months. Subsequently, in January 2009, a hairline crack fracture occurred in Vadodara, which was treated with a cast for 1 month, achieving successful healing. Fast forward to January 2011, at the age of 17 in Chicago, USA, another slip led to a right femur refracture, addressed with elastic nail fixation without deformity correction. No abnormalities were observed in the metabolic bone profile evaluation or pigmentation, indicating the absence of any endocrine disturbances or alterations. The X-ray of the right thigh demonstrated the fracture of the femur with the broken implant in situ, and there was evidence of previously healed fractures along with a shepherd crook deformity (Fig. 1). The pelvic X-ray revealed the coxa vara and the thinned cortex of the femur (Fig. 2). A computed tomography scan of the limb further confirmed the X-ray findings. The patient underwent skin traction as a preliminary measure and a comprehensive surgical plan was developed with the following objectives in mind: (a) achieving local disease control through extended curettage accompanied by the application of phenol and subsequent histopathological examination of the excised tissue, (b) addressing the resulting bone defect by utilizing autogenous bone grafts or suitable alternatives, (c) ensuring fracture stability by employing a DCS plate, (d) rectifying any deformities observed in the neck (neck shaft angle was 95° in this case), proximal femur, and shaft while ensuring optimal fracture reduction, and (e) if feasible, removing the implant; otherwise, retaining it in its current position. The patient was positioned supine on the operating table with appropriate padding under the right hip to ensure optimal access and alignment. A lateral approach was employed, utilizing a carefully planned incision to expose the fractured area. An incision is performed along a line extending from the lateral femoral epicondyle to the greater trochanter, aligning with the length required for the fracture pattern, and mindful of the osteotomies for the deformity correction. The layers of tissue were meticulously dissected, and the vastus lateralis was carefully elevated from the intermuscular septum, exposing the bone. Meticulous curettage was performed to remove the FD tissues and sent for histopathology. Valgus osteotomy and seekh kebab osteotomies were executed to correct Shepherd’s crook deformity and restore the neck shaft angle. DCS fixation was utilized for stable internal fixation, whereas autologous bone grafting was employed to facilitate bone healing. Autologous cortical graft harvested from the iliac crest on the same side of the fracture was utilized in the surgical procedure (Fig. 3).
The patient received immediate post-operative care, which involved implementing rehabilitation exercises to improve the knee’s range of motion and strengthen the affected area. After being discharged with a hip orthosis, the sutures were removed on the 15th day. Progressive exercises were introduced to facilitate mobilization without bearing weight. Unfortunately, at the 10-week mark, the patient experienced a refracture at the osteotomy site and implant failure (Fig. 4). As a result, a subsequent surgical intervention was necessary, involving the utilization of a double-angle DCS and an additional broad DCP to achieve adequate fixation length and repeat bone grafting (Fig. 5).
The patient had a smooth post-operative course following the second surgery and was consistently monitored for 5 years (Fig. 5). Radiographic evaluation revealed successful bone union at 5 months and correction of the deformity. However, a limb length discrepancy of 1.5 cm was noted, which was effectively managed through the use of footwear modifications (Fig. 6). The donor site for obtaining the autologous cortical graft was contralateral iliac crest.
Fracture is a prominent and consequential complication frequently observed in FD cases. The distinct anatomical position of the proximal femur renders it particularly susceptible to both deformities and fractures, attributed to specific anatomical features that increase its vulnerability to FD-related effects [6]. The impact of Shepherd’s crook deformity on the patient’s quality of life and joint function has been significant. The onset of this deformity during adolescence and subsequent pathological fracture with an elastic nail in situ, implantation, and refracture in the fifth decade of life exemplify the challenges and unique characteristics associated with each instance of Shepherd’s crook deformity. Tailored and individualized approaches are essential to achieving proper alignment, optimizing functional outcomes, and improving the overall quality of life for the patient. While previous case reports and case series have addressed the management of fractures in the neck of the femur with deformity in FD, our case represents a unique and uncommon situation where a fracture occurred despite the presence of an implant in situ. Notably, the presence of the shepherd’s crook deformity, which places stress on the femoral shaft, can contribute to the occurrence of pathological fractures. These findings underscore the significance of thorough evaluation and meticulous management of deformities associated with FD to mitigate the risk of fractures [7, 8]. In our case, shepherd’s crook deformity coexisted with a pathological femoral shaft fracture, necessitating the use of a dynamic implant, such as a DCS, along with bone grafting. The DCS implant allows for the controlled collapse of the fracture at the proximal femur. We adopted the technique described by Li et al., as their research demonstrated the effectiveness of valgus osteotomy in combination with DHS internal fixation for managing FD associated with shepherd’s crook deformity. This approach restores the neck-shaft angle and mechanical alignment of the femur, leading to enhanced functionality [7]. The length of the side plate was customized based on the extent of the lesion to ensure comprehensive coverage and minimize the risk of recurrence. In addition, multiple seekh kebab osteotomies, similar to those used in osteogenesis imperfecta treatment, were performed to correct the varus of the femoral shaft resulting from previous fractures [9]. Our case report highlights a unique aspect of the management of FD -associated fractures. In our case, we performed an osteotomy of the shaft to correct the varus deformity resulting from previous fractures. This approach stands out when compared to other case reports. By addressing the varus deformity through the osteotomy, we aimed to achieve optimal alignment and improve functional outcomes for the patient [10]. In response to the patient’s refracture due to premature weight bearing, we modified the implant strategy by replacing it with a double-angled DCS. This change aimed to preserve the neck-shaft angle, a critical factor in maintaining proper anatomical alignment. Furthermore, an additional anterior plate was incorporated to achieve adequate fixation of the distal fragment at the osteotomy site, enhancing the stability and structural integrity of the fracture site.
IA thorough assessment and precise surgical technique selection are imperative when managing fractures in individuals afflicted with FD. The prioritization of correcting underlying deformities precedes the intervention for fractures, ensuring optimal outcomes. Retaining intramedullary implants with sustained bone contact, employing autogenous bone grafts, and refraining from immediate weight-bearing due to the prolonged healing process associated with FD are pivotal considerations. Managing shaft deformity, particularly in varus deformity cases, entails Seekh kebab osteotomy with an extramedullary implant. The number of osteotomies is contingent on the extent of deformity. Post-operative rehabilitation plays a crucial role in minimizing muscle weakness and averting contracture formation. The initiation of weight-bearing activities is guided strictly by radiological evidence of sufficient bone healing. Adhering to these principles facilitates effective management of FD-related fractures, fostering successful healing and promoting functional recovery.
The primary objective of femoral shaft fracture fixation in FD is to achieve alignment of the neck and shaft, stabilize the fracture, and restore the overall alignment of the proximal femur. While union at the osteotomy site carries some risk, proper alignment typically leads to a successful union. The specific location of the osteotomy depends on the extent of the lesion within the proximal femur. By implementing a single-stage correction for shepherd’s crook deformity, including fracture fixation and early rehabilitation; we can aim to reduce patient morbidity. The incorporation of the double-angled DCS presents an alternative implant solution, offering versatility for both deformity correction and secure fixation of femoral neck fractures in cases of FD.
References
- 1.Polyostotic Fibrous Dysplasia. JAMA Surgery. JAMA Network. Available from: https://jamanetwork.com/journals/jamasurgery/article-abstract/543604 [Last accessed on 2023 May 19]. [Google Scholar]
- 2.DiCaprio MR, Enneking WF. Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am 2005;87:1848-64. [Google Scholar]
- 3.Marie PJ, de Pollak C, Chanson P, Lomri A. Increased proliferation of osteoblastic cells expressing the activating Gs alpha mutation in monostotic and polyostotic fibrous dysplasia. Am J Pathol 1997;150:1059-69. [Google Scholar]
- 4.Riminucci M, Liu B, Corsi A, Shenker A, Spiegel AM, Robey PG, et al. The histopathology of fibrous dysplasia of bone in patients with activating mutations of the Gs alpha gene: Site-specific patterns and recurrent histological hallmarks. J Pathol 1999;187:249-58. [Google Scholar]
- 5.Dheenadhayalan J, Avinash M, Lakhani A, Rajasekaran S. Shepherd’s crook deformity: How to set it straight. A five-step surgical guide. J Orthop Surg (Hong Kong) 2019;27:2309499019834362. [Google Scholar]
- 6.Stanton RP, Ippolito E, Springfield D, Lindaman L, Wientroub S, Leet A. The surgical management of fibrous dysplasia of bone. Orphanet J Rare Dis 2012;7:S1. [Google Scholar]
- 7.Wang Y, Luo Y, Min L, Zhou Y, Wang J, Zhang Y, et al. The West China hospital radiographic classification for fibrous dysplasia in femur and adjacent bones: A retrospective analysis of 205 patients. Orthop Surg 2022;14:2096-108. [Google Scholar]
- 8.Tathe PV, Banik S, Mandal S. Surgical treatment modalities in pediatric monostotic fibrous dysplasia of proximal femur - a case series. J Orthop Case Rep 2022;12:13-8. [Google Scholar]
- 9.Abulsaad M, Abdelrahman A. Modified Sofield-Millar operation: Less invasive surgery of lower limbs in osteogenesis imperfecta. Int Orthop 2009;33:527-32. [Google Scholar]
- 10.Majoor BC, Leithner A, van de Sande MA, Appelman-Dijkstra NM, Hamdy NA, Dijkstra PD. Individualized approach to the surgical management of fibrous dysplasia of the proximal femur. Orphanet J Rare Dis 2018;13:72. [Google Scholar]