Bizarre Parosteal Osteochondromatous Proliferation is a rare benign lesion that can be locally aggressive. Wide local resection is vital to prevent recurrence.
Dr. Fatema H Madan, Department of Trauma and Orthopedic Surgery, Salmaniya Medical Complex, Bahrain. E-mail: fatimadan@live.com
Introduction: Bizarre Parosteal Osteochondromatous Proliferation (BPOP) is a rare benign lesion commonly referred to as Nora’s lesion. It typically affects adults in their 20s–30s. Due to its aggressive local invasion, it can be confused with some malignant tumors, including chondrosarcoma. Nora’s lesion can be diagnosed radiographically, and its diagnosis is confirmed with an excisional biopsy.
Case Report: A 40-year-old Bahraini male complained of swelling over the metatarsal head of the second digit, increasing in size over a year. He also complained of a reduced range of motion of the second toe and a pins-and-needles sensation affecting the entire toe. Plain X-ray, computed tomography, and magnetic resonance imaging were done, showing findings suggestive of bizarre parosteal osteochondromatous. The lesion was encasing the flexor tendon of the second digit. He was treated with surgical excision, and histopathology confirmed the diagnosis of BPOP.
Conclusion: We report on a rare presentation of BPOP in the second proximal phalanx of a male in his 40 s. The patient underwent a wide local excision, and the diagnosis was confirmed with histopathology.
Keywords: Bizarre parosteal osteochondromatous proliferation, Nora’s lesion, bone tumors, benign tumors, flexor tendon.
Bizarre parosteal osteochondromatous proliferation (BPOP) is a rare benign lesion commonly referred to as Nora’s lesion. There have been fewer than 160 cases reported in the literature, and the exact etiology is yet to be known [1-3]. In 1983, while working at the Mayo Clinic, the pathologist Frederick E. Nora first described BPOPs; since then, the lesion has been commonly referred to as Nora’s lesion [4]. Due to its similarity in appearance to osteogenic tumors, Nora’s lesion can easily be misdiagnosed and mistreated. We report on a rare presentation of an atypical manifestation in a male patient in his 40s. The patient was diagnosed with BPOP (Nora’s Lesion) of the second proximal phalanx encasing the flexor tendon. The patient was treated with surgical excision, and the diagnosis was confirmed with histopathology.
A Bahraini male in his 40 s, with no known history of medical illness, presented to the outpatient clinic with complaints of a painful, gradually growing swelling that had manifested on the sole of the foot over the course of a year. The pain was moderate in intensity but exacerbated by prolonged standing, walking, and footwear. He also complained of a reduced range of motion of the second toe and a pins-and-needles sensation affecting the entire toe. He stated a history of previous trauma in the affected foot more than 1 year prior to the development of the swelling: a car had run over his foot, but at the time, he did not sustain any obvious fractures and was treated conservatively. He had no history of any other swellings throughout his body and no history of unexplained weight loss, night sweats, or fever. On clinical examination, we found a 3 cm*3 cm round firm swelling (Fig. 1) with clear margins in the plantar aspect of the second metatarsal head. The overlying skin was mobile and intact. The patient had a limited range of movement of the metatarsophalangeal joint of the second toe, but the capillary refill was intact. There was no erythema or tenderness.
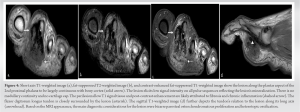
During the first clinic visit, a plain radiograph (Fig. 2) revealed an ossified lesion related to the proximal phalanx of the second digit at the plantar. A second lesion with similar radiographic characteristics but smaller in size and located in the medial aspect of the second metatarsal head was also seen. All blood investigations were within normal limits.
A computed tomography (CT) scan (Fig. 3) showed a fairly well-marginated, heavily calcified lesion seen in relation to the medial cortex of the second-digit proximal phalanx with no definite continuation to the medulla. There was a mild focal area of cortical thickening at the same level.
Magnetic resonance images (Fig. 4) showed a heavily calcified lesion within the plantar aspect of the first webspace related to the proximal phalanx of the second digit that shows minimal post-contrast enhancement. The lesion was encasing the flexor tendon of the second digit with evidence of surrounding subcutaneous soft tissue edema and fat stranding, most likely due to the pressure effect. There was no extension to the tendon, which appeared intact, with no evidence of tendinosis or tenosynovitis.
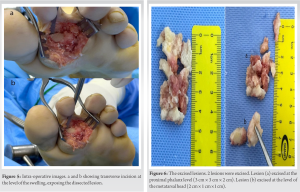
The patient was admitted, and an excisional biopsy of the lesion was performed under general anesthesia. A transverse incision was made in the plantar aspect of the tarsometatarsal joint, directly over the swelling (Fig. 5). A hard sclerotic bony lesion was seen to be extending over the left metatarsophalangeal joint, encasing and surrounding the flexor tendon and bilateral neurovascular bundle (Fig. 6). A complete excision was performed. To achieve a complete resection, the flexor tendon could not be preserved, mainly because it was too deeply embedded within the lesion. The lesion was sent to histopathology.
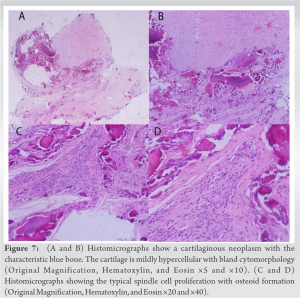
Histopathology of the specimen (Fig. 7) confirmed the clinically suspected diagnosis of BPOP. Two sections of the lesion were examined. The first section showed the proliferation of irregular, benign osteoid fragments and a very focal proliferation of chondroid fragments that appeared to be maturing into the bone with focal irregular ossification and multifocal areas of irregular calcifications. Adjacent to these fragments was a proliferation of benign-looking spindled-fibrous tissue with focal myxoid changes. The other section showed multiple benign mature bony trabeculae intervened by vascular spaces, focal spindle cell proliferation, a few multinucleated giant cells, and sparse chronic inflammation. No cytological atypia, or increased mitoses, or necrosis were seen. No malignancy was detected in the sections studied.
The patient was discharged the day after surgery. He had follow-up examinations in the clinic, and his sutures were removed after 2 weeks. At 3 months, he is still complaining of reduced sensation and limited range of motion in the affected toe and is undergoing physiotherapy; otherwise, he stated reduced pain after surgery.
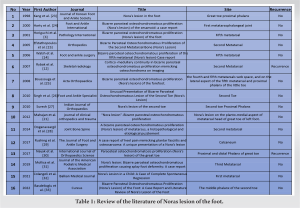
Beginning of the paragraph Bizarre Parosteal Osteochondromatous Proliferation (BPOP) is a relatively rare reactive mineralizing mesenchymal lesion that typically involves the short bones of the hand and foot. The hand is 4 times more likely to be involved than the foot [1, 2]. BPOP can develop in any age group, regardless of gender, but most patients are in their 20 s and 30 s when it appears. This lesion is characterized by local invasion, resulting in misleading diagnoses of malignant lesions such as osteochondroma, especially with atypical imaging findings. The pathogenesis of BPOP is still a matter of controversy. Some theories have considered traumatic causes: Horiguchi et al. [3] considered BPOP a healing process following periosteal injury. He pointed out that many patients reported having experienced trauma at the location of the lesion [4, 5, 6], and this corresponds to our patient’s history of trauma 1 year prior to presentation. Moreover, the presence of basic fibroblast growth factor, vascular endothelial growth factor, and chondromoduline I in the cartilaginous cap was thought to contribute to the osseocartilaginous formation. Furthermore, some refer to the etiology as neoplastic in nature [7]. However, some chromosomal anomalies have been found in BPOP, such as t(1;17) (q32;q21) [8] and t(1;17) (q42;q23) [9]. Patients typically present with complaints of a painful swelling growing in size over months or years [3, 10]. Clinical examination shows a rapidly growing, firm swelling sparing the skin [11]. Pain might result from the compression effect [12]. BPOP is considered a benign lesion with an aggressive local invasion. There have been no cases of metastasis reported [13]. On X-rays, the lesion is typically a well-marginated, ossified mass originating from cortical bone [9, 14]. A CT scan is superior to a plain radiograph in determining the disrupted continuity between the cortex and medulla and the absence of periosteal reactions [15, 16]. Magnetic resonance imaging shows the heterogeneous low signal intensity on T1 sequences, and the lesion is directly derived from the cortical surfaces of the affected bone. These lesions do not manifest any medullary involvement or cortical flaring, which are characterizers of osteochondroma [6, 9]. The lesion spreads throughout the cortical surface and has no continuity with the normal medulla. Histologically, it is distinguished by an exophytic outgrowth from the cortical surface, a heterogeneous mixture of bone, cartilage, and fibrous tissue [17]. Differential diagnosis includes osteochondroma, parosteal osteosarcoma, subungual exostosis, myositis ossificans, and florid reactive periostitis. Nora’s lesion can also be misdiagnosed as a malignant lesion such as chondrosarcoma [18], parosteal chondrosarcoma [11], and conventional osteosarcoma [11, 18]. While osteochondroma is the most common benign lesion, it is rarely found in distal bones as it is most commonly found in long bones [11, 19, 20]. Nora’s lesion can be differentiated from parosteal osteosarcoma by its lobular architecture: slim, short, and irregular bony trabeculae with distinct blue tinctorial osteoid [9, 20]. BPOP can be treated conservatively if it is asymptomatic. On the other hand, if it is causing pain and compressive symptoms, it is treated with wide local excision and decortication of the affected bone. There have been reports of high recurrence rates following excision, reaching 20–50% [11, 13, 20]. Berber et al. [13] found a recurrence rate of 27%. Furthermore, Nora et al. noted a 51% rate of primary recurrence and a 22% rate of secondary recurrence. They also reported that recurrence occurred within 2 years of follow-up [11]. However, it has been proposed that recurrence rates are lower in patients who underwent excision of the pseudocapsule, periosteal tissue, and any abnormal areas of the cortex [9]. A few similar cases were reported in the literature, such as Mahajan et al. [21] discussing Nora’s lesion involving the first metatarsal head; as in our case, the patient underwent a wide local excisional biopsy, and histopathology confirmed the diagnosis of BPOP. Walsh et al. [14] reported a male in his 50s who developed a swelling between the fourth and fifth metatarsals. However, only one case reported tendon involvement in such a lesion, where Soejima and Ogata [22] reported the presentation of an extensor pollicis longus tendon rupture caused by BPOP in a 58-year-old woman. Otherwise, there were no reported cases of similar manifestations like in our patient, where the lesion was adhering, encasing, and surrounding the flexor tendon of the digit, resulting in disruption of the tendon following complete. A literature review of Nora’s lesion of the foot is summarized in Table 1.
In summary, BPOP is a rare benign lesion affecting the small bones of the hand and feet. The etiology is still to be confirmed. However, our patient’s history of trauma might support the parosteal reparation theory. The diagnosis requires a high level of suspicion and can be made using imaging modalities and histopathology. The recommended treatment is a complete excision.
BPOP are rare lesions that can manifest by local invasion of the surrounding tissue, mimicking malignant lesions such as osteochondroma. BPOP can be treated conservatively, but surgical excision is indicated in symptomatic patients. This lesion is associated with a high recurrence rate; therefore, complete excision and surveillance are critical.
References
- 1.Torreggiani WC, Munk PL, Al-Ismail K, O’Connell JX, Nicolaou S, Lee MJ, et al. MR imaging features of bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Eur J Radiol 2001;40:224-31. [Google Scholar]
- 2.Orui H, Ishikawa A, Tsuchiya T, Ogino T. Magnetic resonance imaging characteristics of bizarre parosteal osteochondromatous proliferation of the hand: A case report. J Hand Surg 2002;27:1104-8. [Google Scholar]
- 3.Horiguchi H, Sakane M, Matsui M, Wadano Y. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of the foot. Pathology international 2001;51:816-23. [Google Scholar]
- 4.Bandiera S, Bacchini P, Bertoni F. Bizarre parosteal osteochondromatous proliferation of bone. Skelet Radiol 1998;27:154-6. [Google Scholar]
- 5.De Lange EE, Pope TL, Keats T, Fechner R. Case report 428: Bizarre parosteal osteochondromatous proliferation (BPOP). Skelet Rad 1987;16:481-3. [Google Scholar]
- 6.Ly JQ, Bui-Mansfield LT, Taylor DC. Radiologic demonstration of temporal development of bizarre parosteal osteochondromatous proliferation. Clin Imaging 2004;28:216-8. [Google Scholar]
- 7.Zambrano E, Nosé V, Perez-Atayde AR, Gebhardt M, Hresko MT, Kleinman P, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parosteal osteochondromatous proliferation (Nora lesion). Am J Surg Pathol 2004;28:1033-9. [Google Scholar]
- 8.Campanacci DA, Guarracino R, Franchi A, Capanna R. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion). Description of six cases and a review of the literature. Chir Organi Mov 1999;84:65-71. [Google Scholar]
- 9.Michelsen H, Abramovici L, Steiner G, Posner MA. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) in the hand. J Hand Surg 2004;29:520-5. [Google Scholar]
- 10.Rastogi R. Musculoskeletal. Indian J Radiol Imaging 2007;17:308-9. [Google Scholar]
- 11.Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol 1983;7:245-50. [Google Scholar]
- 12.Rybak LD, Abramovici L, Kenan S, Posner MA, Bonar F, Steiner GC. Cortico-medullary continuity in bizarre parosteal osteochondromatous proliferation mimicking osteochondroma on imaging. Skelet Radiol 2007;36:829-34. [Google Scholar]
- 13.Berber O, Dawson-Bowling S, Jalgaonkar A, Miles J, Pollock R, Skinner J, et al. Bizarre parosteal osteochondromatous proliferation of bone: Clinical management of a series of 22 cases. J Bone Joint Surg Br 2011;93:1118-21. [Google Scholar]
- 14.Walsh J, Murphy D, Freihaut R, O’Keane J, Stephens M. Bizarre parosteal osteochondromatous proliferation of the fifth metatarsal (Nora’s lesion)-case report. Foot Ankle Surg 2006;12:211-4. [Google Scholar]
- 15.Efstathopoulos NE, Papagelopoulos PJ, Lazarettos IT, Savvidu OD, Kaseta MA, Giannakou N, et al. Bizarre parosteal osteochondromatous proliferation of the second metatarsal bone (Nora’s lesion). Orthopedics 2005;28:168-70. [Google Scholar]
- 16.Soon J, Chang H, Sim C, Teoh L, Low C. A case of bizarre parosteal osteochondromatous proliferation of the hand. Singapore Med J 2003;44:27-30. [Google Scholar]
- 17.Gruber G, Giessauf C, Leithner A, Zacherl M, Clar H, Bodo K, et al. Bizarre parosteal osteochondromatous proliferation (Nora lesion): A report of 3 cases and a review of the literature. Can J Surg 2008;51:486-9. [Google Scholar]
- 18.Smith NC, Ellis AM, McCarthy S, McNaught P. Bizarre parosteal osteochondromatous proliferation: A review of seven cases. Aust N Z J Surg 1996;66:694-7. [Google Scholar]
- 19.Abramovici L, Steiner GC. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion): A retrospective study of 12 cases, 2 arising in long bones. Hum Pathol 2002;33:1205-10. [Google Scholar]
- 20.Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol 1993;17:691-7. [Google Scholar]
- 21.Mahajan S, Chandra R, Lal YM. Nora lesion”-Bizarre parosteal osteochondromatous proliferation. J Clin Orthop Trauma 2012;3:119-21. [Google Scholar]
- 22.Soejima O, Ogata TI. Case reports extensor pollicis longus tendon rupture caused by a bizarre parosteal osteochondromatous proliferation of the wrist. Hand Surg 1998;3:277-81. [Google Scholar]
- 23.Kang HJ, Cho NH, Park JH, Ha JW. Nora’s lesion in the foot. J Korean Foot Ankle Soc 1998;2:48-51. [Google Scholar]
- 24.Harty J, Kelly P, Niall D, O’Keane J, Stephens M. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of the sesamoid: A case report. Foot Ankle Int 2000;21:408-12. [Google Scholar]
- 25.Boussouga M, Harket A, Bousselmame N, Lazrak K. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of the forefoot. Acta Orthop Belg 2008;74:562-5. [Google Scholar]
- 26.Singh R, Jain M, Siwach R, Rohilla RK, Kaur K. Unusual presentation of bizarre parosteal osteochondromatous lesion of the second toe (Nora’s lesion). Foot Ankle Spec 2010;3:347-51. [Google Scholar]
- 27.Suresh S. Nora’s lesion of the second toe. Indian J Orthop 2010;44:342-4. [Google Scholar]
- 28.Doganavsargil B, Argin M, Sezak M, Kececi B, Pehlivanoglu B, Oztop F. A bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of metatarsus, a histopathological and etiological puzzlement. Joint Bone Spine 2014;81:537-40. [Google Scholar]
- 29.Rushing CJ, Rogers DE, Spinner SM, Gajzer DC. A case report of heel pain mimicking plantar fasciitis and osteosarcoma: A unique presentation of a Nora’s lesion. J Foot Ankle Surg 2017;56:670-3. [Google Scholar]
- 30.Nayak AR, Yamsani AK, Pathan AA. Paraosteal osteochondromatosis proliferation (Nora’s lesion) of the great toe. Int J Orthop Sci 2017;3:111-3. [Google Scholar]
- 31.Mollica AJ, Getz B, Ezike C, Brannick B, Mollica AJ. Nora’s lesion: Bizarre parosteal osteochondromatous proliferation causing splay foot deformity: A case report. J Am Podiatr Med Assoc 2019;109:463-6. [Google Scholar]
- 32.Colangeli M, Spinnato P, Zarantonello P, Bendandi B, Donati DM. Nora’s lesion in a child: A case of complete spontaneous regression. Balkan Med J 2021;38:57-8. [Google Scholar]
- 33.Başdelioğlu K, Yıldırım AN, Reddy K, Özkan K. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of the foot: A case report and literature review of Nora’s lesion of the foot. Cureus 2022;14:e24197. [Google Scholar]