Extensively drug-resistant tuberculosis (Pre-XDR and XDR) in spondylodiscitis demands accurate diagnosis to avoid misclassification. Ensuring precision is crucial for implementing suitable drug-sensitive chemotherapy and, if needed, considering surgical intervention to achieve optimal outcomes.
Dr. Tanmay Avhad, Department of Orthopaedics, B.Y.L Nair Charitable Hospital, Mumbai, Maharashtra, India. E-mail: tanmayavhad@gmail.com
Introduction: Pre-extensively drug-resistant tuberculosis (TB) is characterized by resistance to either a fluoroquinolone (FQ) or a second-line injectable but not both. The urgent need for prompt diagnosis and targeted treatment is emphasized. This report aims to spotlight a case of spinal TB with insufficient assessment, resulting in delayed definitive treatment and an oversight contributing to heightened morbidity.
Case Report: An 18-year-old female who was initially diagnosed to have multidrug-resistant TB leading to a 2-year treatment which eventually resulted in multifocal involvement of the spine revealing TB relapse with FQ resistance, categorized as pre-extensively drug-resistant TB. Treatment was shifted to newer drugs, addressing challenges like bilateral psoas abscess, which lead to clinical improvement, allowing the patient to make a good recovery.
Conclusion: This case report emphasizes the significance of conducting culture and drug sensitivity testing in patients with tubercular spondylodiscitis. The aim is to prevent misdiagnosis and ensure informed decisions regarding definitive medical treatment or surgical management when necessary.
Keywords: Pre-extensively drug-resistant, tuberculosis, drug resistance, drug sensitivity testing.
Tuberculosis (TB) remains a major contributor to global health as the leading infectious cause of death worldwide [1, 2]. The diagnosis of drug-resistant spinal TB is often delayed, leading to the development of spinal deformities and neurological complications [3]. Multidrug-resistant TB (MDR-TB) refers to TB resistant to both rifampicin and isoniazid. Extensively drug-resistant TB (XDR-TB) is characterized by resistance to at least one fluoroquinolone (FQ) and one injectable agent used in MDR-TB treatment regimens, in addition to being MDR-TB [1]. Pre-XDR-TB is defined as MDR-TB with resistance to either an FQ or a second-line injectable, but not both [4]. The burden of PreXDR-TB is significant and poses a threat to MDR-TB control [5]. The increasing incidence of MDR Spine TB in various continents is not unexpected due to global migration trends. In the WHO European region, which comprises 53 member states, there is a notable variation in TB notifications, ranging from 2.8 cases/100,000 population in Italy to 123 cases in Kazakhstan in 2010. In a retrospective analysis of 967 patients treated for spinal TB, drug susceptibility these, 48.98% had MDR strains, and 2 had XDR strains [6, 7]. The aim of this report is to draw attention to a case of multilevel spinal TB that was insufficiently assessed, leading to delays in definitive treatment and an oversight that contributed to increased morbidity.
An 18 Consequently, empiric antitubercular therapy for 6 months (Category 1) was initiated given the geographical prevalence of the disease. Notably, the initial course of treatment resulted in clinical improvement, the patient remained asymptomatic for a period of 8 years when she developed a cervical lymph node swelling, prompting revaluation.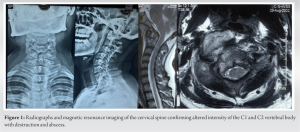

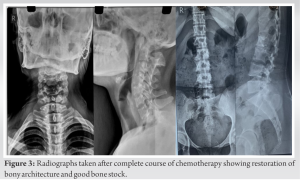
Pre-XDR-TB has emerged as a growing concern, posing a threat to global TB control efforts [4-6]. Drug resistance (DR) is seldom innate; instead, it typically arises due to inappropriate drug therapy and non-adherence to treatment protocols [8]. The diagnosis of DR TB spondylodiscitis is frequently delayed, with a time lag ranging from 6 months to 2 years [9]. In the study by Wang et al., an evaluation of GeneXpert, smear positivity, and histopathology in culture-positive cases of spinal TB revealed that GeneXpert exhibited the highest sensitivity at 98.79%, followed by histopathology (84.24%) and smear positivity (36.3%). Nevertheless, recent findings on GeneXpert analysis in drug-resistant spinal TB have indicated false-positive results for rifampicin resistance when compared to traditional DST. This underscores the importance of not solely relying on GeneXpert analysis and emphasizes the necessity of performing DST in all cases. Management of Pre-XDR-TB involves a multicentric and holistic approach. The success of treatment depends on various factors, including host immunity, the extent of DR, and the severity [10, 11]. Due to the absence of guidelines for managing spinal MDR-TB and the documented use of both surgical and conservative approaches, the current indications for surgery align with those for non-resistant spinal TB. These generally include a lack of response to chemotherapy, instability, deformity, gross neurological deficits, signs of the spine being at risk, and debilitating pain-hindering ambulation. In cases without culture positivity where DST cannot be performed, surgery may be considered if there is no improvement after initiating chemotherapy [2]. Delamanid and bedaquiline, novel drugs increasingly employed in the treatment of MDR- and XDR-TB, are currently categorized in group D2 [12]. Their recommended use in adults is for a maximum duration of 6 months at the prescribed doses. Existing evidence in adults indicates that both delamanid and bedaquiline contribute to enhanced sputum smear and culture conversions, as well as increased success rates at the conclusion of treatment [13]. These are the newer drugs shown to be promising; however, more extensive research and studies are yet to be done to evaluate the pharmacodynamic and pharmacokinetics and their effect on such highly resistant strains of M. tuberculosis. Medical practitioners often exhibit a heightened level of suspicion and a propensity to initiate empirical antitubercular treatment promptly. However, this case underscores the crucial importance of conducting DST to assess the sensitivity pattern of the Mycobacterium strain and identify primary MDR or XDR TB strains. Failure to conduct DST can result in ineffective treatment and contribute to the continued emergence of DR. The case faced a significant challenge when the patient, diagnosed with MDR-TB through CBNAAT or GeneXpert, underwent inadequate therapy due to undiagnosed FQ resistance. This led to treatment failure and subsequent relapse over 2 years. Later, Pre-XDR TB affecting cervical and lumbar vertebrae was identified. The management approach involved initiating appropriate chemotherapy and source reduction through abscess pigtailing. Surgical correction might be considered if treatment fails or vertebral destruction causes neurodeficit and progressive deformity. Ongoing monitoring, including bracing and regular follow-ups, remains crucial for assessing therapy response.
This case report serves as a crucial reminder of the imperative need for culture and drug sensitivity testing in diagnosing tubercular spondylodiscitis. With the escalating incidence of Pre-XDR and XDR cases, it emphasizes the vital role of accurate diagnosis to avoid misclassification aiding the planning for definitive treatment.
The report highlights the importance of informed decision-making for both medical and surgical interventions, underlining the challenges in managing drug-resistant TB affecting the spine. Overall, it calls attention to the evolving landscape of TB and the necessity for comprehensive diagnostic approaches in clinical practice.
References
- 1.World Health Organization. Global Tuberculosis Report 2019. Geneva: World Health Organization; 2019. [Google Scholar]
- 2.Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: Current concepts. Global Spine J 2018;8:96S-108. [Google Scholar]
- 3.Jain AK, Jaggi KR, Bhayana H, Saha R. Drug-resistant spinal tuberculosis. Indian J Orthop 2018;52:100-7. [Google Scholar]
- 4.Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Am J Respir Crit Care Med 2010;182:113-9. [Google Scholar]
- 5.Singhal P, Dixit P, Singh P, Jaiswal I, Singh M, Jain A. A study on pre-XDR & XDR tuberculosis and their prevalent genotypes in clinical isolates of Mycobacterium tuberculosis in North India. Indian J Med Res 2016;143:341-7. [Google Scholar]
- 6.Dara M, Dadu A, Kremer K, Zaleskis R, Kluge HH. Epidemiology of tuberculosis in WHO European Region and public health response. Eur Spine J 2013;22:549-55. [Google Scholar]
- 7.Shi T, Zhang Z, Dai F, Zhou Q, He Q, Luo F, et al. Retrospective study of 967 patients with spinal tuberculosis. Orthopedics 2016;39:e838-43. [Google Scholar]
- 8.Disratthakit A, Prammananan T, Tribuddharat C, Thaipisuttikul I, Doi N, Leechawengwongs M, et al. Role of gyrB mutations in pre-extensively and extensively drug-resistant tuberculosis in Thai clinical isolates. Antimicrob Agents Chemother 2016;60:5189-97. [Google Scholar]
- 9.Suarez-Garcia I, Noguerado A. Drug treatment of multidrug-resistant osteoarticular tuberculosis: A systematic literature review. Int J Infect Dis 2012;16:e774-8. [Google Scholar]
- 10.Wang G, Dong W, Lan T, Fan J, Tang K, Li Y, et al. Diagnostic accuracy evaluation of the conventional and molecular tests for spinal tuberculosis in a cohort, head-to-head study. Emerg Microbes Infect 2018;7:109. [Google Scholar]
- 11.The Emerging Threat of Drug-Resistant Tuberculosis in Southern Africa: Global and Local Challenges and Solutions: Summary of a Joint Workshop. Available from: https://www.ncbi.nlm.nih.gov/ books/nbk55582 [Last accessed on 2016 Feb 04]. [Google Scholar]
- 12.World Health Organization. WHO Treatment Guidelines for Drug-Resistant Tuberculosis 2016 Update. WHO/HTM/TB 2016.04. Geneva: World Health Organization; 2016. [Google Scholar]
- 13.D’Ambrosio L, Centis R, Tiberi S, Tadolini M, Dalcolmo M, Rendon A, et al. Delamanid and bedaquiline to treat multidrug-resistant and extensively drug-resistant tuberculosis in children: A systematic review. J Thorac Dis 2017;9:2093-101. [Google Scholar]










