The diagnosis and treatment protocol outlined in this article for the management of cysticercosis of the muscle belly is important to be aware of otherwise can be missed for a long time.
Dr. Dhruv A Shah, Department of Orthopaedics, MGM Medical College, Navi Mumbai – 410 209, Maharashtra, India. E-mail: dr.dhruvshah96@gmail.com
Introduction: Cysticercosis leads to a cyst formation known to occur due to the Taenia solium parasite. Patients normally present with seeding and formation of the cysts in the central nervous system (CNS) as neurocysticercosis (NCC). Intramuscular cysts are rare presentations and are mostly incidental findings in NCC patients. We present a rare case of a rapidly progressing isolated cysticercosis of the flexor digitorum profundus (FDP) muscle leading to a pseudotumor and presenting with pseudo-Volkmanns contracture and a positive Volkmanns sign.
Case report: A 26-year-old right-hand dominant vegetarian female presented with a 3-month-old progressive swelling on her right forearm with no antecedent trauma history. A positive Volkmann’s sign was present. Radiographs were normal, and ultrasonography showed a cysticercus cyst in the FDP muscle belly with a multiseptated abscess around the tendons of the middle, ring, and little fingers at the musculotendinous junction. Bones and nerves were spared. After ruling out CNS involvement and providing oral antiparasitic cover, she underwent a successful surgical exploration with cyst excision, debridement, and freeing of the involved tendons. Immediately post-operatively, she was able to completely extend the three involved fingers without flexion at the wrist joint (resolving Volkmann’s sign). She reported significant improvements in the functions of daily life. She was protected with a splint for 2 weeks. There was no recurrence, and the swelling subsided. Histo-pathology reports depicted cysts with visible scolices.
Conclusion: It is important to consider the possibility of ‘Myoparasitism’ in atraumatic cases showing contractures. Clinching the right diagnosis is essential and best done with a multidisciplinary approach with ultrasonography, magnetic resonance imaging, electromyography, and nerve conduction velocity studies. It is essential to rule out life-threatening NCC beforehand and offer prophylaxis. Surgical exploration is generally indicated to regain normal function and free the involved structures.
Keywords: Volkmanns contracture, cysticercosis, pseudotumor, cyst.
Cysticercosis is a parasitic infection that occurs due to the larvae of Taenia solium [1]. Cysticercosis occurs worldwide but has a higher prevalence in developing countries due to poor access to sanitation facilities and close interaction between humans and animals, especially pigs. It is the most common human parasitic infection of the nervous system in immunocompetent individuals [2]. Isolated muscular involvement is extremely rare, and if present, is often underreported due to a high threshold for suspicion and being a neglected disease [3]. Often, the disease is part of the spectrum in which a neural cyst is present along with a muscular cyst [4]. In contrast to neurocysticercosis (NCC), the musculoskeletal involvement is generally not fatal [5]. The muscular form has been described in three forms: the myalgic type, the mass type, and the pseudohypertrophic type [6]. The patient may be afebrile and can range from asymptomatic to presenting with a painful, tender swelling, and rarely, as we report, can present with pseudo-Volkmanns contracture. Head, neck, trunk, and upper limb involvement are seen more commonly than lower limb involvement [7]. The diagnosis of intramuscular cysticercosis is often missed due to nonspecific clinical presentations and can have several clinical differentials, such as lipomas, epidermoid cysts, neuroma, neurofibromas, pseudoganglia, sarcoma, myxoma, pyomyositis, a cold abscess, or tuberculous lymphadenitis [6].
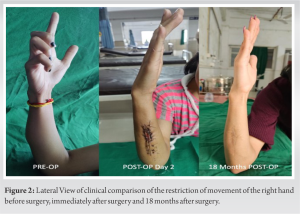
A 26-year-old healthy female right-hand dominant vegetarian female presented to our orthopedic outpatient clinic with the complaints of a 3-month-old progressive swelling that suddenly appeared on the medial aspect of her forearm and had gradually progressed in size over the past 3 months. She had no antecedent trauma history. She had difficulty extending her right middle, ring, and little finger and was kept in a flexed position at the metacarpophalangeal and interphalangeal joints, with a more severe deformity of the little finger than the middle finger (Fig. 1 and 2).
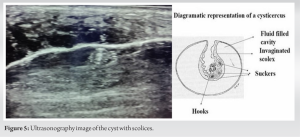
Plain orthogonal radiographs were taken of the forearm, and any bony injury or abnormality was ruled out. A specialized ultrasonography was undertaken of the forearm by a musculoskeletal sonologist and was suggestive of a well-defined hypoechoic multiseptated cystic lesion measuring 6.5 cm × 3.8 cm × 2.2 cm with a central echogenicity suggestive of a scolex. On a color Doppler, the mass and wall showed increased vascularity. The lesion was located at the musculotendinous junction of the flexor digitorum profundus (FDP) muscle, with the tendons of the medial three fingers passing through the lesion. The overlying ulnar artery and nerve were spared. An electromyography-nerve conduction velocity was done to confirm the non-involvement of the nerves of the forearm (Fig. 5).
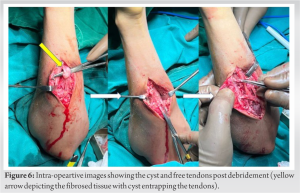
After consulting with an infectious diseases specialist, the patient underwent magnetic resource imaging (MRI) of the brain to rule out any NCC, along with an MRI of the forearm. The patient was advised oral praziquantel thrice daily and albendazole twice daily for 14 days to assist in the involution of the cyst, and a trial was given to manage the patient conservatively. Unfortunately, after 8 days of treatment with the above antiparasitic drugs, the cyst wall burst, and there was a yellowish discharge from the skin from the center of the swelling. The patient was admitted, and after an anesthetic workup, surgical exploration and debridement were planned. After administering general anesthesia and aseptic preparation of the patient under a tourniquet, a 10 cm incision was made on the antero-medial aspect of the forearm, centered over the swelling. The soft tissue was dissected, the FDP tendon was approached, and the cyst was visualized. The cyst was incised and opened, and the purulent sample was collected. The necrotic tissue and all visible material of the cyst were debrided, and the tendons were visualized and freed. A thorough wash was given to remove all the necrotic material from the wound. The tendons were visualized, and their free movement was appreciated by passively extending and flexing the fingers of the hand. The ulnar nerve and artery were explored, and their non-involvement was confirmed. The wound was closed over an 8-Fr negative suction romovac drain with a polyamide monofilament suture. A sterile dressing was applied. The drain was removed on the following day of the surgery. She had no neurovascular compromise post-surgery and was started on active and passive physiotherapy on day 2 after surgery (Fig. 6: yellow arrow depicting the fibrosed tissue with a cyst entrapping the tendons). The patient had a return of range of movement and a resolving Volkmann’s sign. The flexion and contracture of the fingers were reduced immediately! The middle and ring fingers returned to near full extension, and the little finger also improved. She was discharged on post-operative day 4 with regular daily physiotherapy, a cover of Praziquantel and Albendazole for a further 2 weeks, and advice for a regular follow-up. The intra-op histopathological sample came positive for T. solium, with its characteristic hooklets and suckers being identified. She was regularly followed up at 3 monthly intervals, and at 1 year post-op follow-up, she had full resolution of the disease and a complete range of movement with no flexion or contracture of any of the fingers and no systemic manifestations.
Cysticercosis is a disease occurring due to the infestation with the larval form of the T. solium parasite. This infection occurs mostly in developing countries due to the consumption of infected food and water. The most common presentations are headaches and seizures due to neural involvement and the formation of a space-occupying lesion in the brain. This being said, isolated intramuscular involvements of cysticercosis are also seen. In previously reported English literature, this single unilocular or multilocular cyst has been reported only 5 times in the biceps brachii muscle [8], flexor digitorum profundus [9], psoas [10], extensor carpi ulnaris [11], and the tendoachilles tendon sheath [12]. It is documented that, while the larvae grow inside the cyst, they may remain minimally antigenic until the host response or chemotherapy causes gradual death of the cyst accompanied by marked inflammation and pericystic edema [13]. Only once before has the involvement of Flexor digitorum profundus been reported. A swelling of the forearm with contracture of the wrist or fingers with no previous history of trauma should warrant an investigation for the possibility of a pseudotumor formation due to cysticercosis infestation. This report aims to appraise the orthopedic surgeon regarding the presentation of this condition and the available investigation and management options. A radiograph would only be able to show a soft tissue shadow or, rarely, can show a calcified cyst. These can sometimes be found as incidental findings in asymptomatic patients. High-resolution ultrasonography remains the investigation of choice, with the ability to visualize the cyst and underlying soft-tissue structures with accuracy and a lower cost. The only possible limitation is the intra-observer bias in sonography diagnosis. The scolex of the parasite within an oval or round, well-defined cystic lesion, if visualized, becomes the diagnostic feature. MRI remains a gold standard technique for intramuscular cysticercosis. MRI is superior to a computed tomography scan in evaluating the disease stages and edema. Laboratory studies can aid in the diagnosis, viz., erythrocyte sedimentation rate and C-reactive protein. At some centers, there may be a possibility to confirm diagnosis with the help of indirect hemagglutination, enzyme-linked immunosorbent assays, and enzyme-linked immunoelectrotransfer blots by diagnosing specific antibodies in the serum [14]. They help in diagnosing an active or inactive phase of the disease. All patients with suspected cysticercosis infection should undergo some sort of neuroimaging to rule out any cyst or infestation in the brain. For management, treatment is indicated for patients with live cysticerci. It is most commonly treated with praziquantel (50 mg/kg for 15–30 days) or albendazole (10–15 mg/kg for 10–15 days) [15]. The inflammation may be reduced by the administration of concomitant corticosteroids at a low dose. There may be a need for a cover with an antiepileptic drug. For cysts that are outside the central nervous, system the most appropriate approach is a surgical resection of the lesion, which should be done under the cover of medical therapy [16].
The diagnosis of cysticercosis of the muscle or myoparasitism should be considered in cases where a patient presents with swelling of the forearm, which may or may not have any contractures or movement abnormalities. Clinching the diagnosis is essential to begin treatment and allow further imaging to prevent any other complications.
The accurate diagnosis and treatment protocol outlined above in this article for the management of cysticercosis of the muscle belly are important to be aware of. Also, the importance of surgical management along with medical cover is essential in the treatment and prevention of any other untoward manifestations.
References
- 1.Del Brutto OH, Sotelo J. Neurocysticercosis: An update. Rev Infect Dis 1988;10:1075-87. [Google Scholar]
- 2.Del Brutto OH, Wadia NH, Dumas M, Cruz M, Tsang VC, Schantz PM. Proposal of diagnostic criteria for human cysticercosis and neurocysticercosis. J Neurol Sci 1996;142:1-6. [Google Scholar]
- 3.Zemeno-Alanis GH. A classification of human cysticercosis. In: Fissler A, Willms K, Laclette JP, editors. Cysticercosis: Present State of Knowledge and Perspectives. New York: Academic Press; 1982. p. 107-27. [Google Scholar]
- 4.Brown ST, Brown AE, Filippa DA, Coit D, Armstrong D. Extraneural cysticercosis presenting as a tumor in a seronegative patient. Clin Infect Dis 1992;14:53-5. [Google Scholar]
- 5.Brown HW, Neva FA, editors. Basic Clinical Parasitology. Extraintestinal Larval Tapeworms of Human Beings. 5th ed. Norwalk, Conn: Appleton-Century-Crofts; 1983. p. 191-205. [Google Scholar]
- 6.Meena D, Gupta M, Jain VK, Arya RK. Isolated intramuscular cysticercosis: Clinicopathological features, diagnosis and management-a review. J Clin Orthop Trauma 2016;7 Suppl 2:243-9. [Google Scholar]
- 7.Vianna LG, Macedo V, Costa JM. Musculocutaneous and visceral cysticercosis: A rare disease? Rev Inst Med Trop Sao Paulo 1991;33:129-36. [Google Scholar]
- 8.Nagaraj C, Singh S, Joshi A, Trikha V. Cysticercosis of biceps brachii: A rare cause of posterior interosseous nerve syndrome. Joint Bone Spine 2008;75:219-21. [Google Scholar]
- 9.Anderson GA, Chandi SM. Cysticercosis of the flexor digitorum profundus muscle producing flexion deformity of the fingers. J Hand Surg Br 1993;18:360-2. [Google Scholar]
- 10.Mittal A, Sharma NS. Psoas muscle cysticercosis presenting as acute appendicitis. J Clin Ultrasound 2008;36:430-1. [Google Scholar]
- 11.Agarwal S, Akhtar MN. Cysticercosis of externsor carpi ulnaris-a differential diagnosis for painful swelling at elbow. J Orthop Case Rep 2011;1:3-6. [Google Scholar]
- 12.Agarwal S, Gogoi P. An unusual case of cysticercosis of the tendon sheath of tendoachilles-a case report. Electron Physician 2010;2:45-8. [Google Scholar]
- 13.Kaur M, Joshi K, Ganguly NK, Mahajan RC, Malla NC. Evaluation of the efficacy of albendazole against the larvae of Taenia solium in experimentally infected pigs, and kinetics of immune response. Int J Parasit 1995;25:1443-50. [Google Scholar]
- 14.Proano-Narvez JV, Meza-Lucas A, Mata-Ruiz O, García-Jerónimo RC, Correa D. Laboratory diagnosis of Human neurocysticercosis: Double-blind comparison of Enzyme-linked immunosorbent assay and electroimmunotransfer blot assay. J Clin Microbiol 2002;40:2115. [Google Scholar]
- 15.Takayanagui OM, Jardim E. Therapy for neurocysticercosis. Comparison between albendazole and praziquantel. Arch Neurol 1992;49:290-4. [Google Scholar]
- 16.Ogilvie CM, Kasten P, Rovinsky D, Workman KL, Johnston JO. Cysticercosis of the triceps--an unusual pseudotumor: case report and review. Clin Orthop Relat Res. 2001 Jan;(382):217-21. doi: 10.1097/00003086-200101000-00029. PMID: 11153991. [Google Scholar]